MIS posterior short segment fixation with pedicle screws
1. Introduction
Preliminary remarks
MIS reduces the surgical trauma for the patient, potentially resulting in a quicker recovery while providing similar clinical mid to long term results.
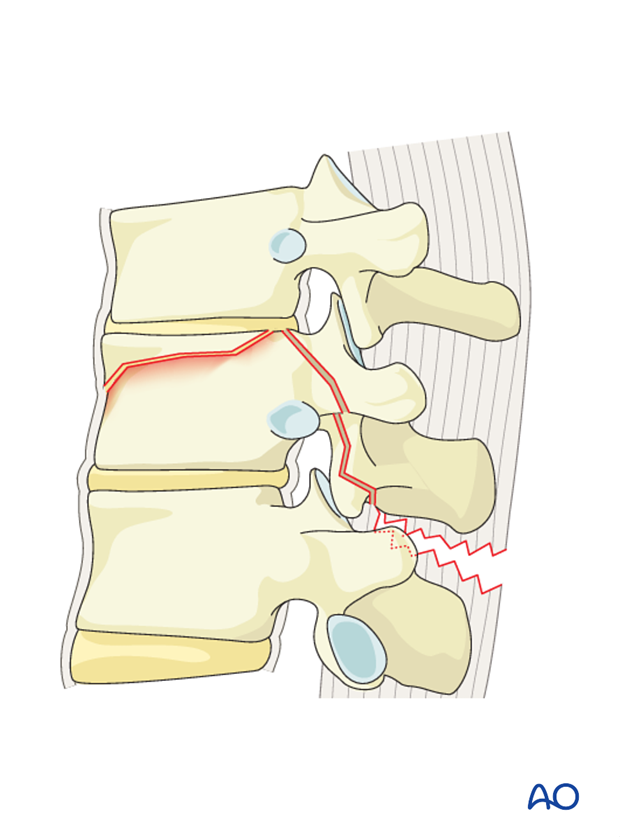
Decompression
In cases where neurological deficit is observed and compression of the spinal canal is assumed, decompression has to be performed. It should be understood that this is a step that can also result in deterioration of neurology unless very meticulously performed.
Decompression can be performed anteriorly or posteriorly. Posteriorly decompression can be indirect or direct.
Indirect decompression may be tried before performing direct decompression.
Please refer to Decompression techniques for a detailed discussion of indications for the posterior decompression techniques. ( Posterior decompression)
Repair of dural laceration
More details on repair of dural laceration can be found here.
2. Patient preparation and approach
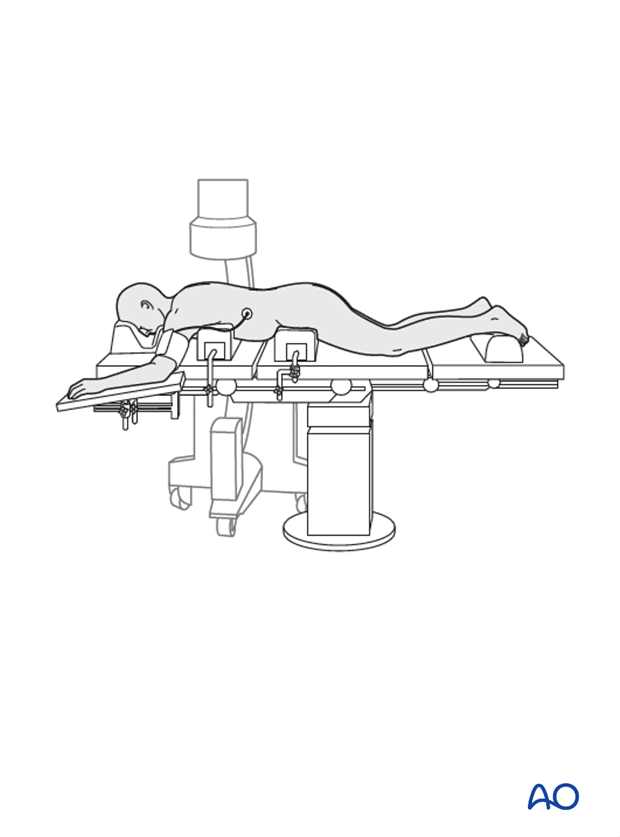
Percutaneous posterior approach for pedicle screw placement is used together with the appropriate patient preparation.
3. Closed reduction
Primary reduction is performed by positioning of the patient onto a frame to create lordosis or kyphosis as needed by the fracture type and the level of the injury.
4. Reduction with pedicle screws (MIS)
Preliminary remarks
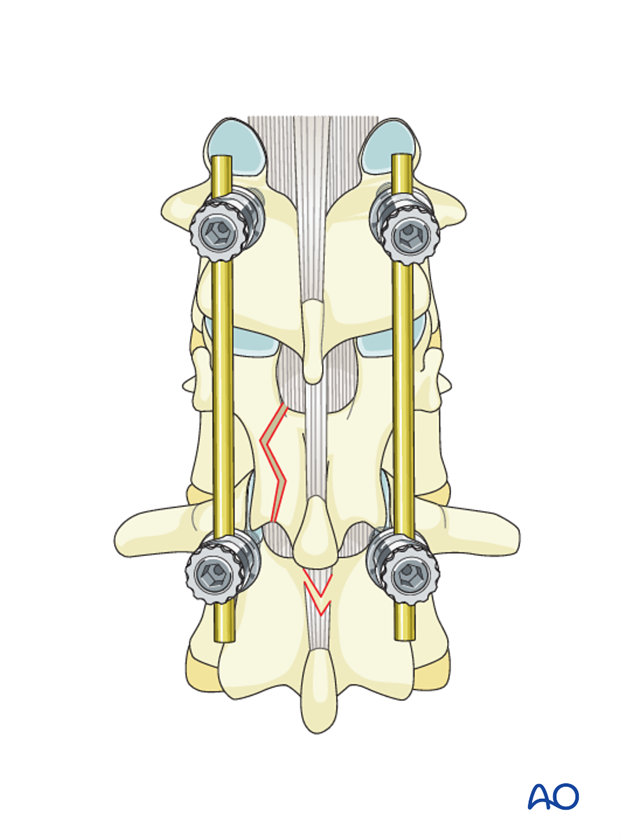
Due to the fact that bilateral instrumentation is necessary in all cases, all steps described below are repeated on the opposite side, unless described differently.
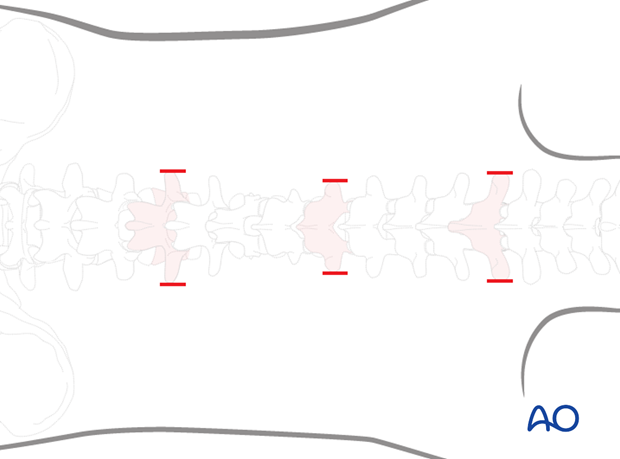
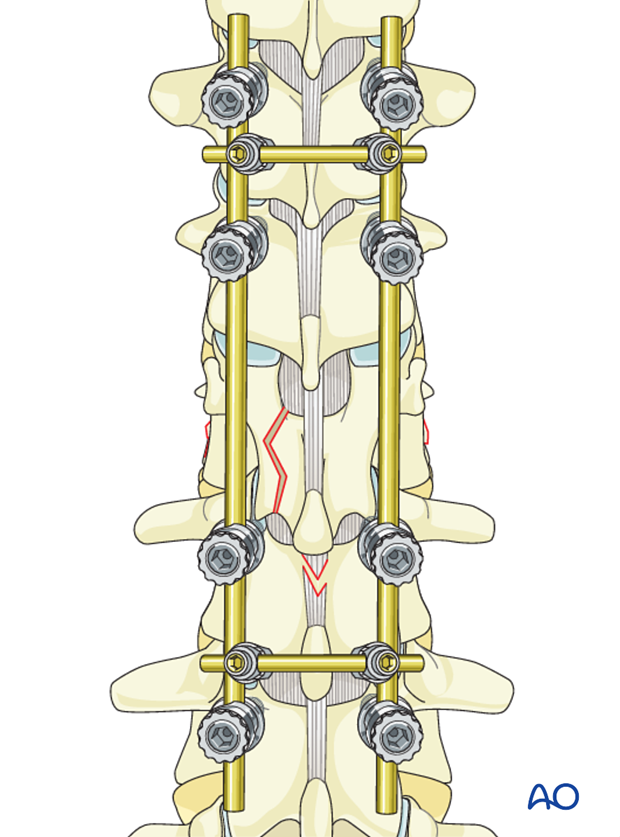
Pitfall: Multisegmental stabilization
In the thoracic spine, multisegmental stabilization is recommended, because reduction is more complicated and loss of mobility is less critical due to the relative rigidity of the thoracic spine.
If multisegmental stabilization is necessary, add screws in the adjacent caudal and cranial vertebrae.
Pedicle screw insertion
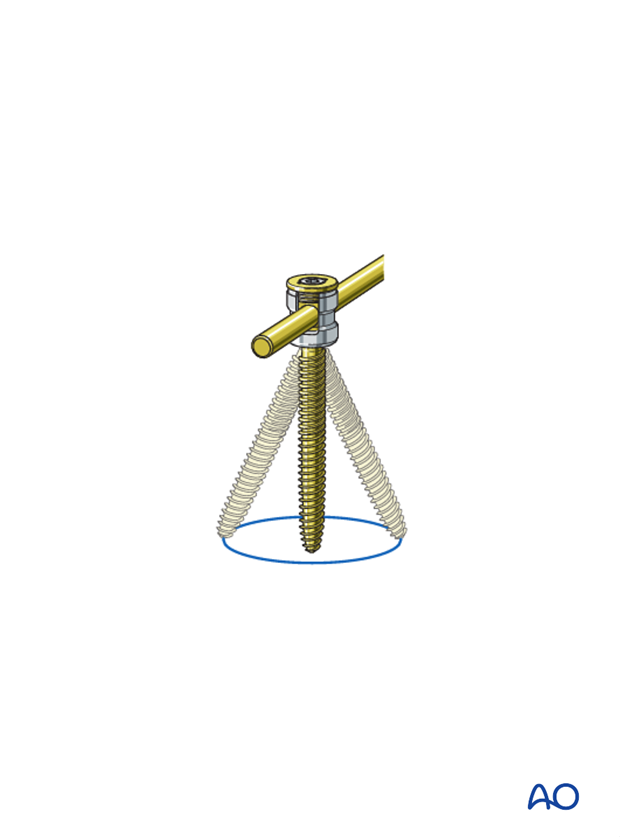
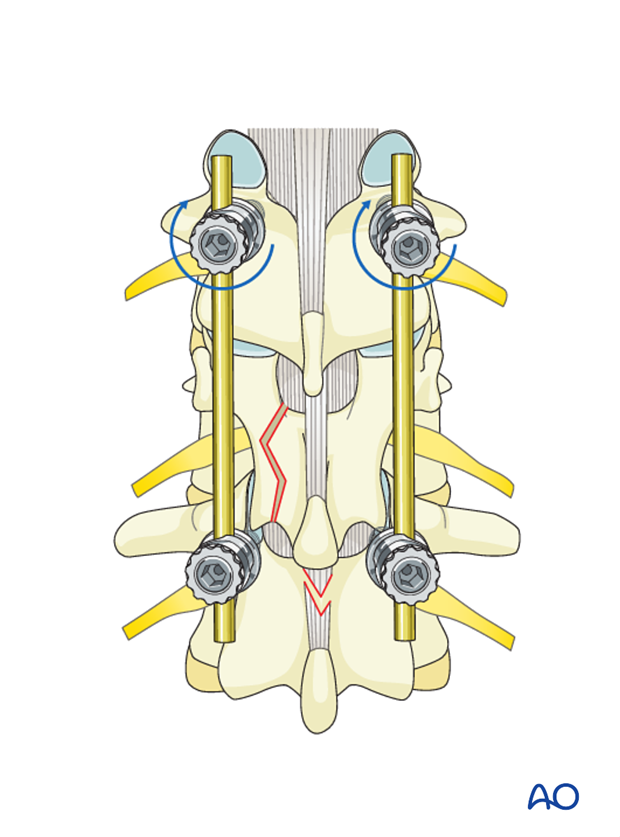
Pedicle screws are inserted into the vertebrae cephalad and caudal to the fracture level on both sides. Mono- or polyaxial top or side loading screws can be used in any combination.
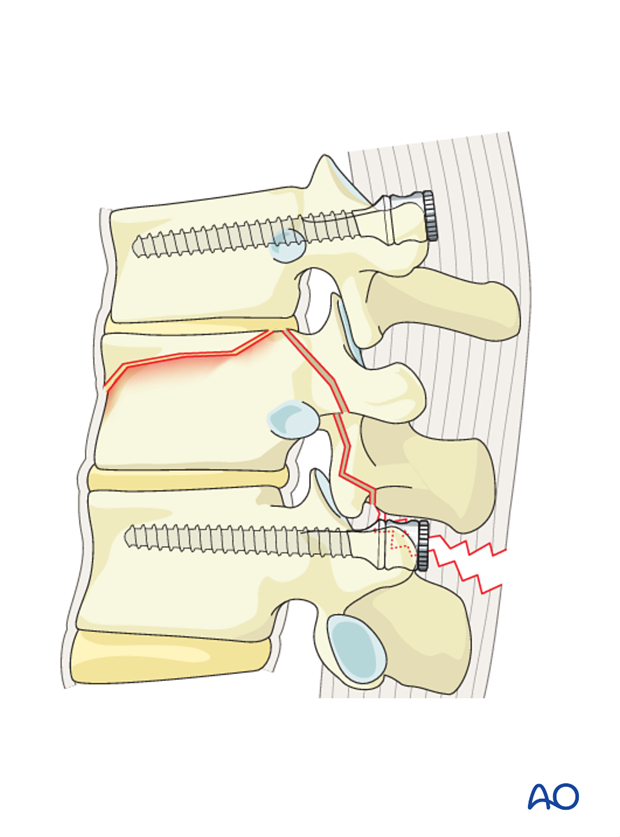
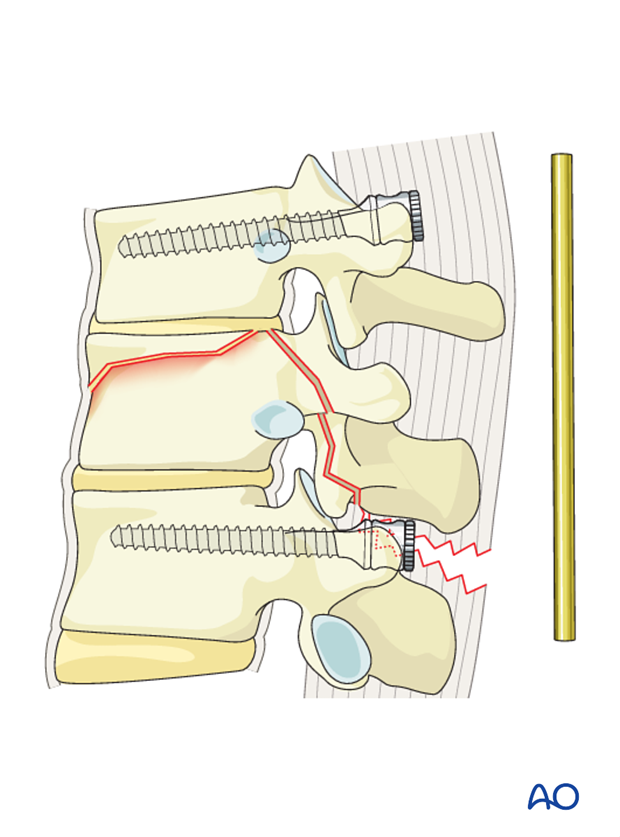
Rod contouring
The amount of lordotic/kyphotic reduction is defined by the pre-bending of the rod. This restores the height of the vertebral body, especially in the anterior part.
Multiple attempts to bend the rod correctly might be necessary.
Rod insertion
The rods are introduced to the distal screw heads on both sides and tightened.
The rod is then inserted into the proximal screw heads without tightening.
Decompression
If it is decided to perform an indirect decompression, this is done at this stage. If indirect decompression proves to be insufficient, a direct decompression eg, posterior or transpedicular decompressions are undertaken. Refer to the Posterior Decompression techniques for detailed instructions. ( Posterior decompression)
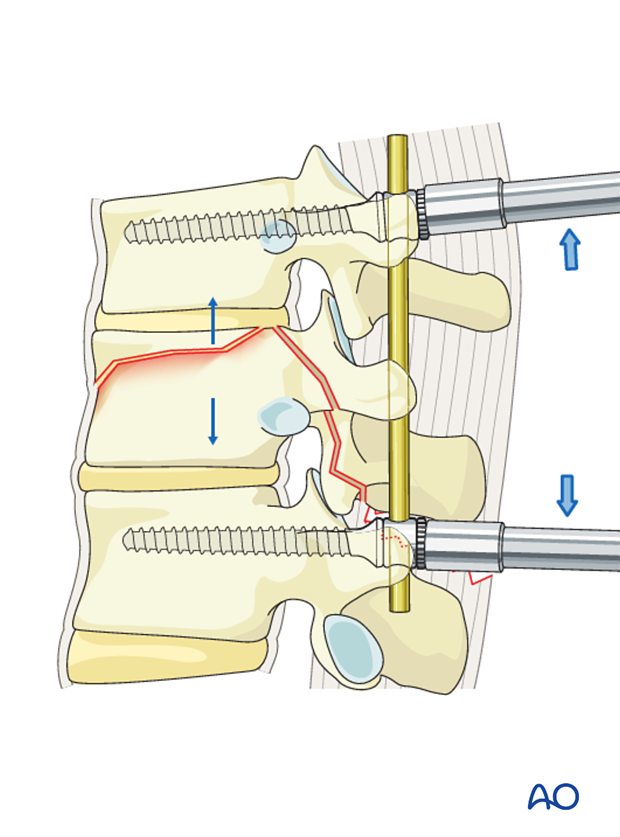
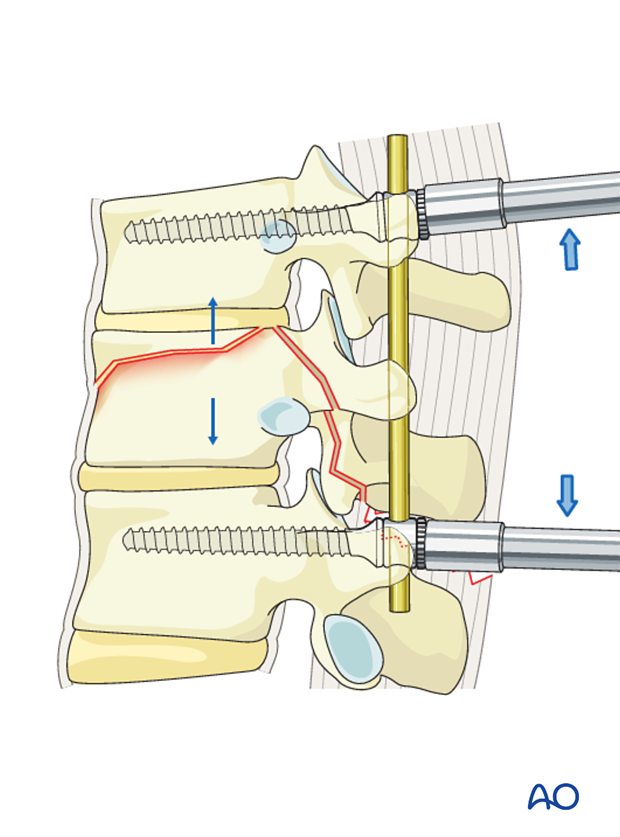
5. Distraction
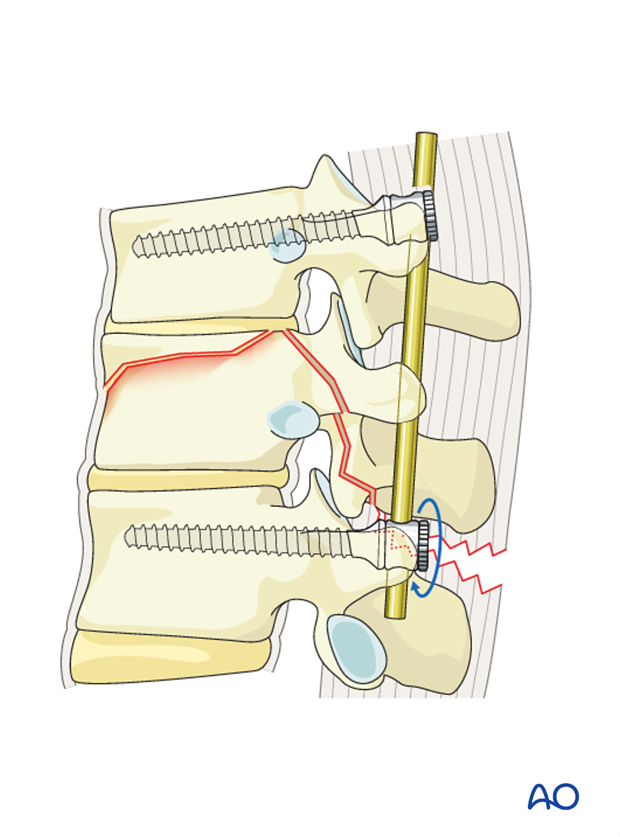
Monoaxial toploading screws
Distraction of the monoaxial screws is performed using a distraction device. This restores the height of the vertebral body, especially in the posterior part.
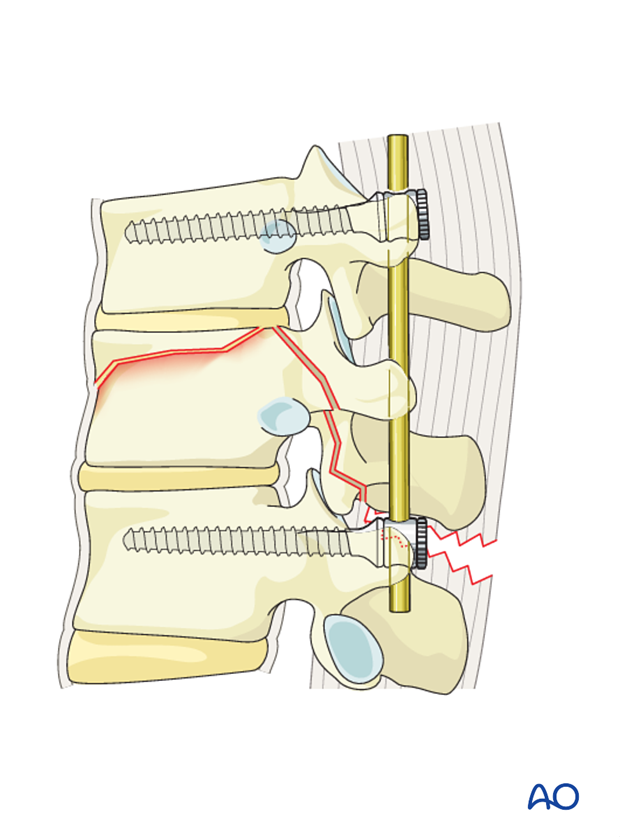
Polyaxial toploading screws
Polyaxial toploading fixation should only be used if adequate closed reduction could be achieved.
Lordotic/kyphotic reduction is not possible with polyaxial toploading screws.
Distraction of the fractured vertebra using polyaxial screws is performed using a distraction device.
The screw heads are tightened with the inner nuts to secure the reduction achieved.
The final construct is shown from a lateral view.

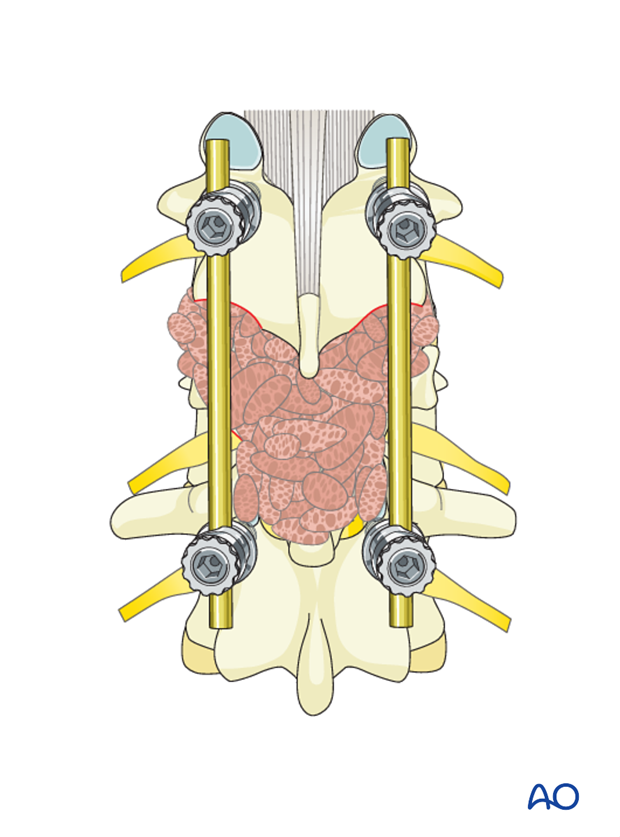
6. Fusion
Decision
Although fusion was routinely performed for all spinal fractures, its indications are now being restricted to fractures that are highly unstable.
Nonfusion fixations can be performed for A3, A4, and B1 type injuries. Fusion is routinely performed for A2, B2, B3 and all C injuries as they are unstable injuries with extensive soft tissue and ligamentous disruption.
If the surgeon plans for a fusion, the facet capsule is excised and the joint cartilage surfaces are denuded/curetted.
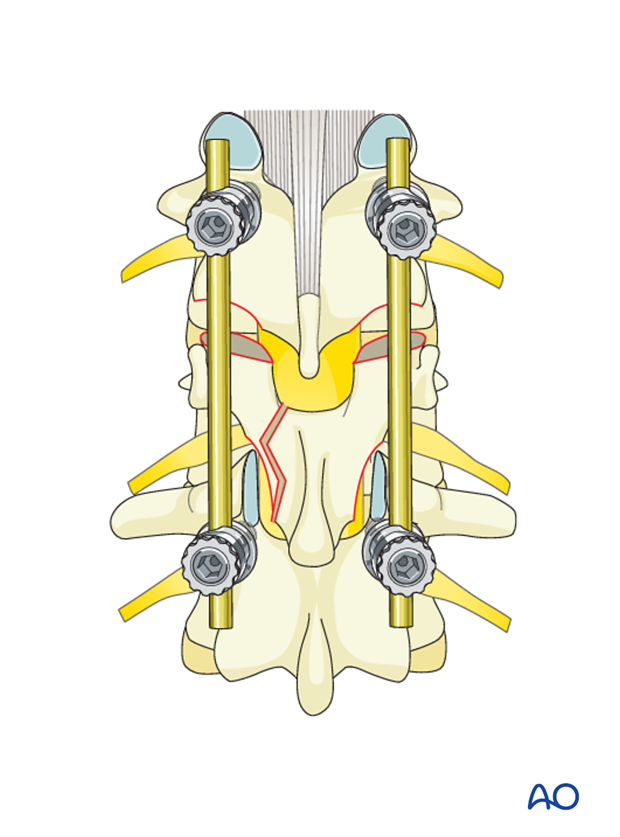
Pieces of bone graft (autograft, allograft) are inserted into the decorticated facet joint for fusion.
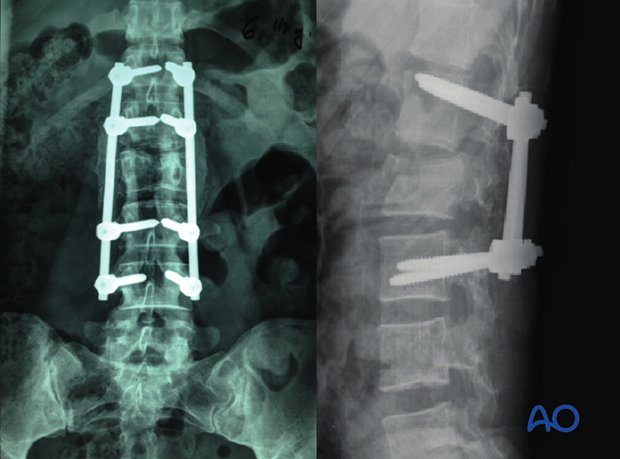
7. Intraoperative imaging
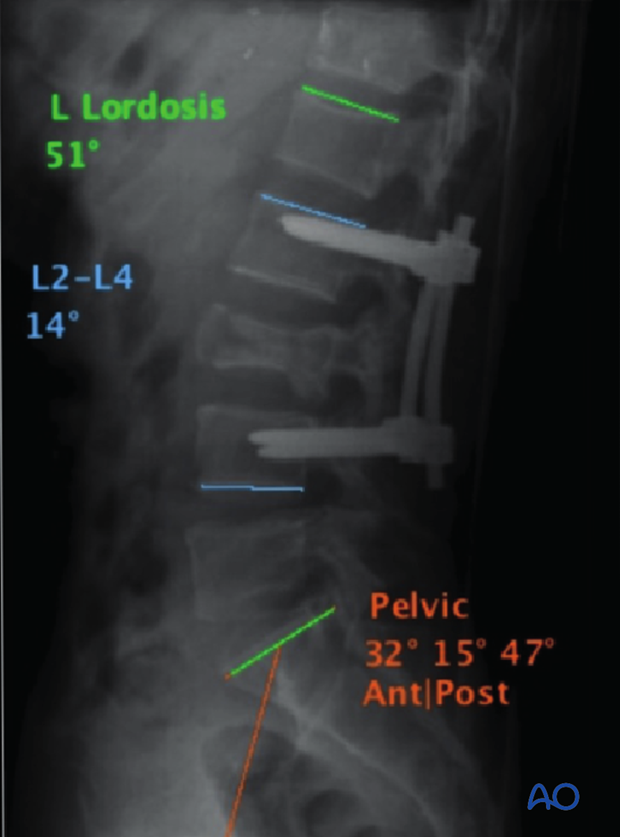
Prior to wound closure, intra-operative imaging is performed to check the adequacy of reduction, position and length of screws and the overall coronal and sagittal spinal alignment.
8. Aftercare for posterior procedures
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional. Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year. Normally, 5-10 degrees of loss of kyphosis can be observed within the first 6 months, which does not affect the functional outcomes. For nonfusion surgeries, the implants can be removed once fusion is confirmed.