Posterior endoscopic cervical foraminotomy (PECF)
1. Introduction
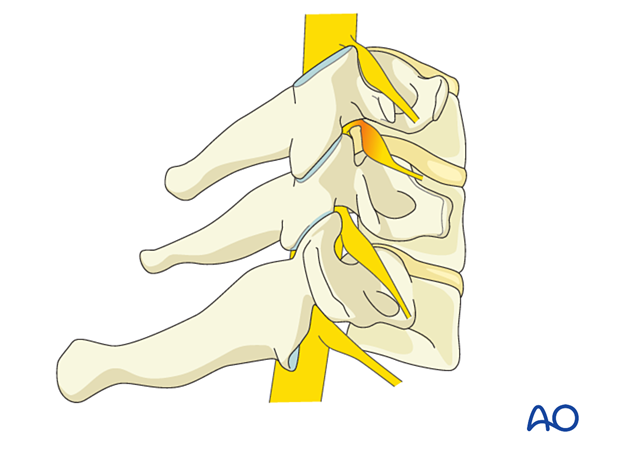
It may not always be clear from imaging whether the compression is caused by disc hernia and/or bony stenosis.
Thus, the sequence of this procedure is first to perform bony decompression to expose the nerve root. In some cases, this may be adequate.
However, inspection for disc herniation should always be performed and addressed if indicated. Additional bony decompression may be needed in cases of calcified discs or osteophytes.
To prevent instability, no more than 50% of the facet joint should be removed.
2. Required instruments
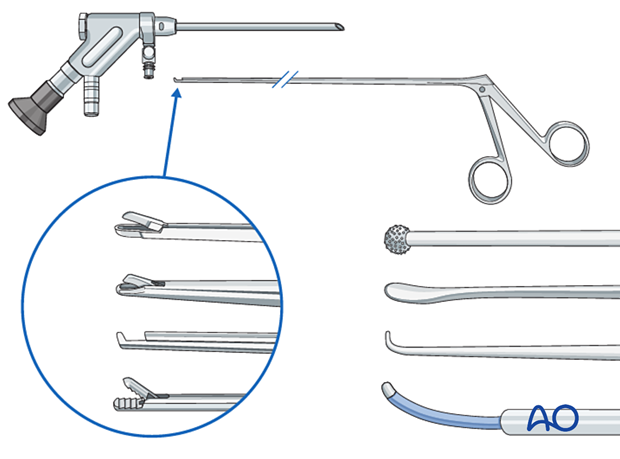
The following specialized instruments are recommended for this procedure:
- Endoscopy cart (video, pump (40 mmHg), radiofrequency unit, drill)
- Cervical endoscope
- Blunt dissector
- Micro-punch
- Grasping forceps
- Kerrison rongeur
- Bipolar coagulator
- Side-cutting drill
- Burr
- C-arm
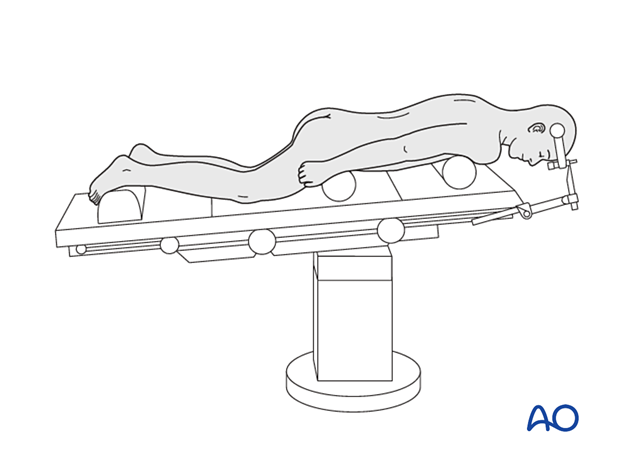
3. OR set up and patient positioning
The patient is placed in a prone position with the head in a Mayfield head holder, with slight flexion of the neck in a reversed Trendelenburg position.
4. Fluoroscopic identification of target level after draping
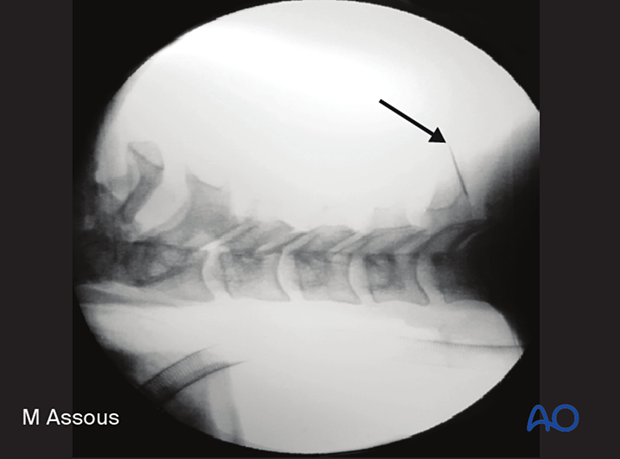
The correct operative level is determined using a spinal needle and AP and lateral fluoroscopy or navigation.
Aim the needle parallel to the disc space, directly at the facet joint.
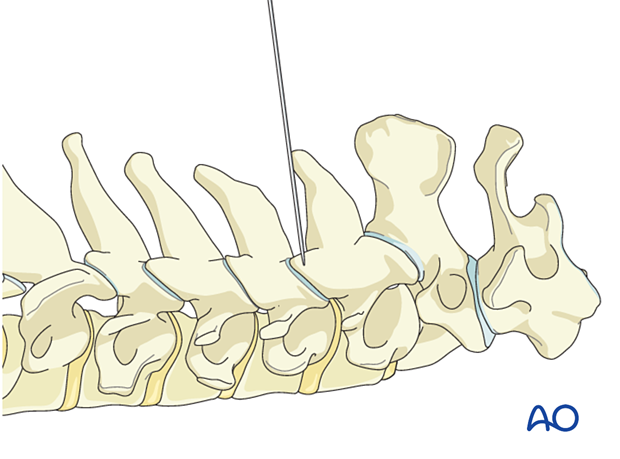
Alternatively, use 3D navigation to localize the correct level throughout the procedure.
5. Visualization of the surgical field
Incision
The skin can be infiltrated as per the surgeon's preference.
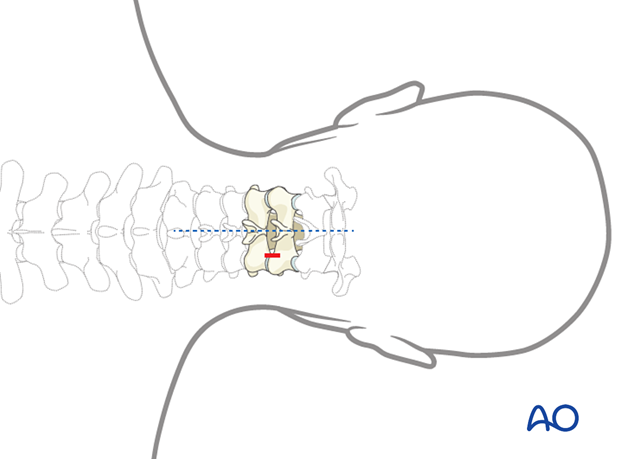
Perform a 1 cm paramedian incision on the symptomatic side. Typically, this will be 1.5–3 cm lateral to the midline.
Given the dense layers of the neck muscles, the blade should be used to open the fascia carefully.
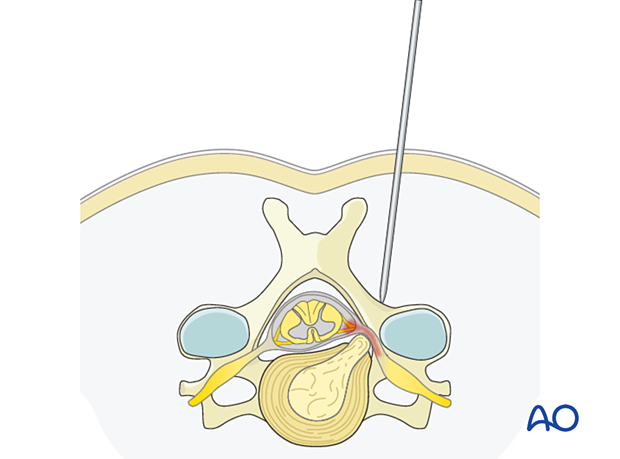
The trocar is advanced through the incision along the planned trajectory under fluoroscopic guidance down to the lateral inferior edge of the cranial lamina.
Insertion of dilators
Insert dilators to expand the soft tissue corridor.
Finally, insert the working channel with the bevel facing medially.
The working channel should be docked firmly on bone at the level of the juxtaposed lamina.
Controlled downward pressure should be maintained at all times to prevent muscle creep into the field of view.
Visualization
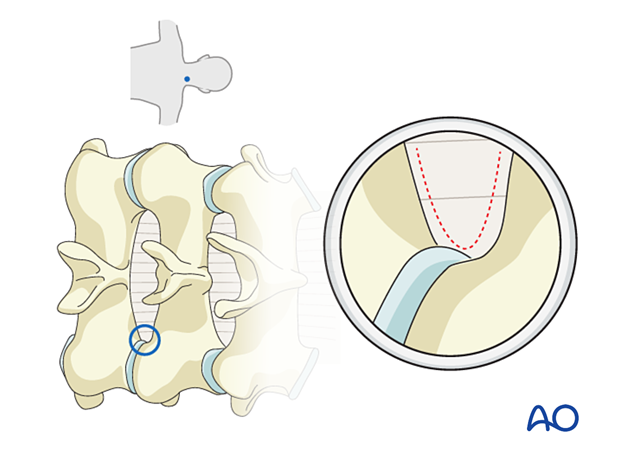
Insert the endoscope and use a bipolar coagulator to clean off the soft tissues and identify the characteristic V-shape comprised of the inferior edge of the cranial lamina and the superior edge of the caudal lamina.
The medial aspect of the inferior and superior articular process also needs to be visualized.
Verify the correct level using fluoroscopy.
6. Decompression
Using a diamond burr, the inferior edge of the cranial lamina is drilled along the attachment of the ligamentum flavum.
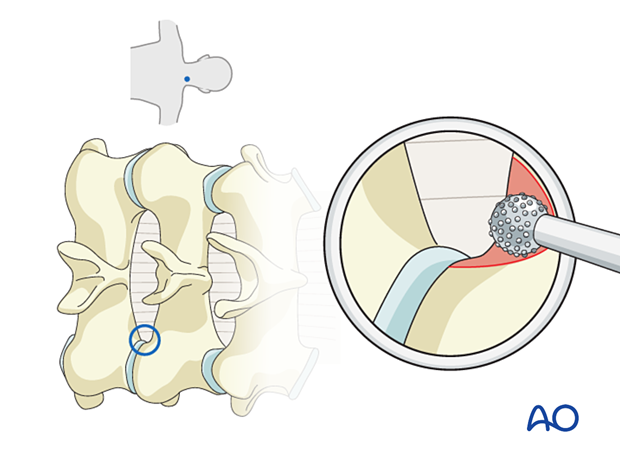
The hemilaminotomy is completed by drilling the superior edge of the caudal lamina.
Care should be taken as the ligamentum flavum is thinner at the level of the caudal lamina and thus offers less protection of the neural elements.
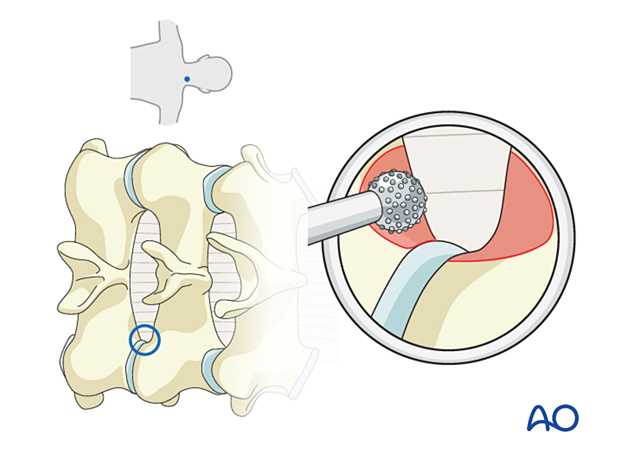
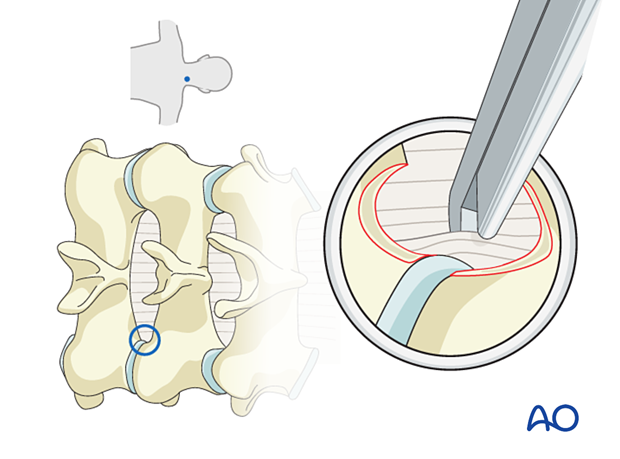
When thinned sufficiently, continue the hemilaminotomy using a 1–2 mm Kerrison rongeur to expose the lateral margin of the ligamentum flavum (LF).
The lateral aspect of the LF may be visualized, and is dissected using a blunt nerve hook.
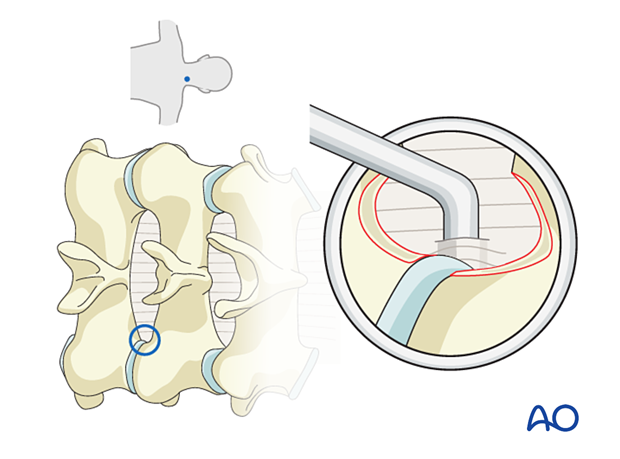
Alternatively, a 1 mm Kerrison rongeur may be used from medial to lateral to resect exposed LF.
Use bipolar diathermy on a low setting before completely removing the LF to reduce venous bleeding, which is very common at this stage.
The use of hemostatic agents may be required.
Keep in mind that the intraforaminal nerve root is not typically covered by the LF and can therefore be injured if entered unexpectedly with the drill.
Foraminal decompression
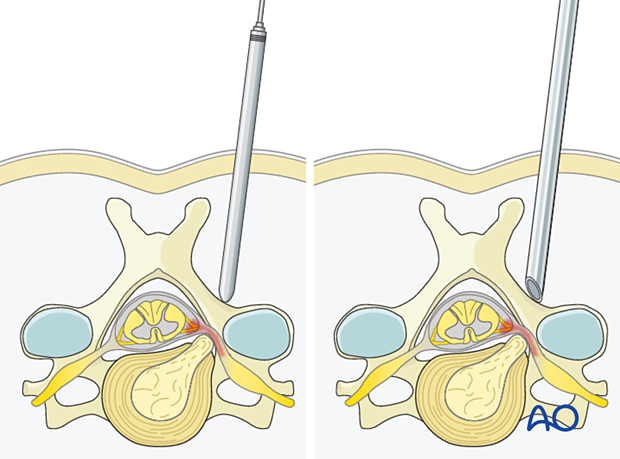
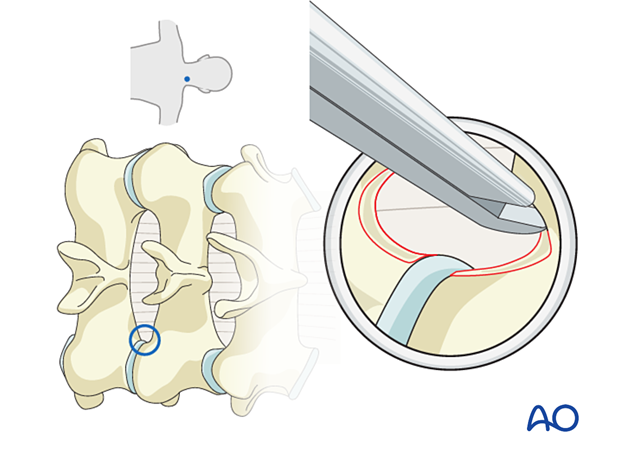
The hemilaminotomy is completed once the underlying nerve root and dura are visualized.
The exiting nerve root is typically most compressed underneath the superior articulating process. Care should be taken to thin this out with the burr.
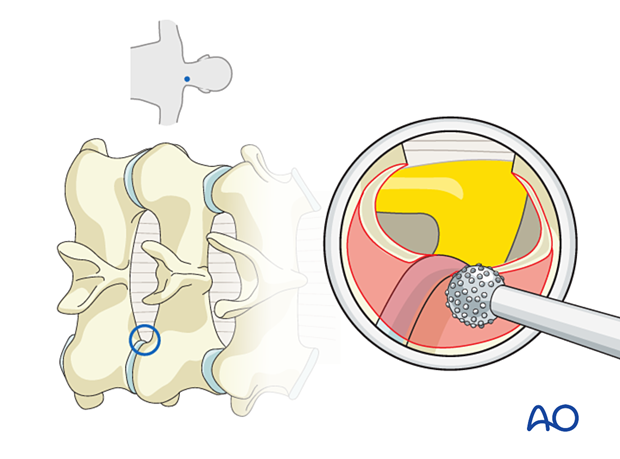
The smallest size Kerrison is used when decompressing the nerve in order to avoid unnecessary nerve root compression.
A blunt nerve hook can be used to palpate the caudal and cranial pedicles to confirm adequate decompression.
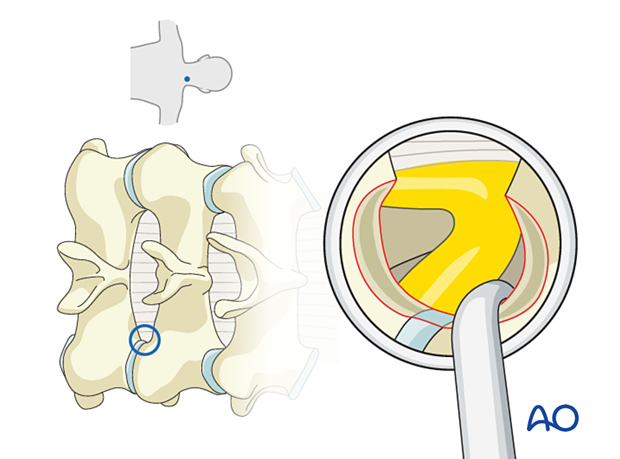
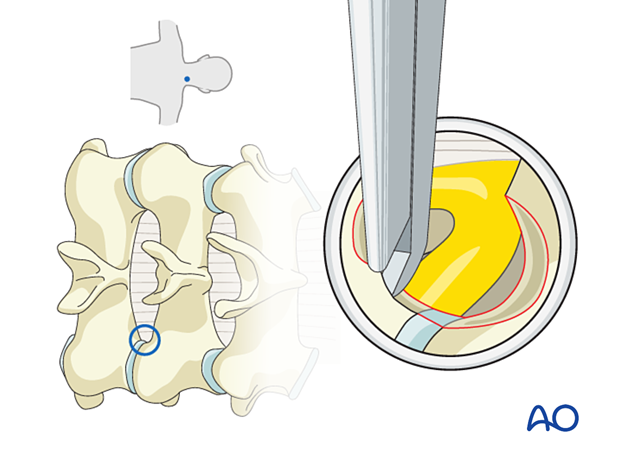
Ensuring there is enough cranial decompression, the nerve root can be slightly mobilized cranially to explore the disc.
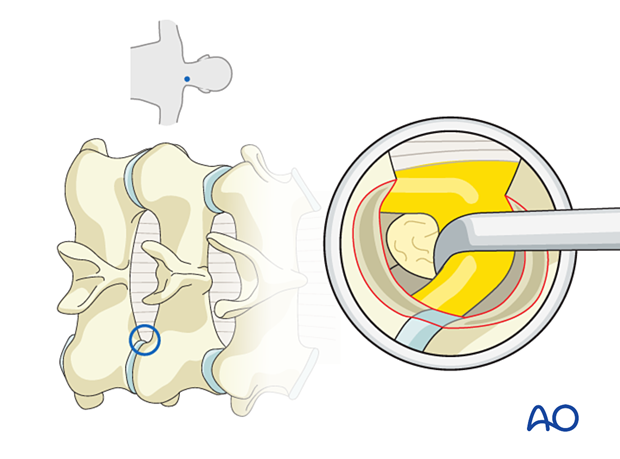
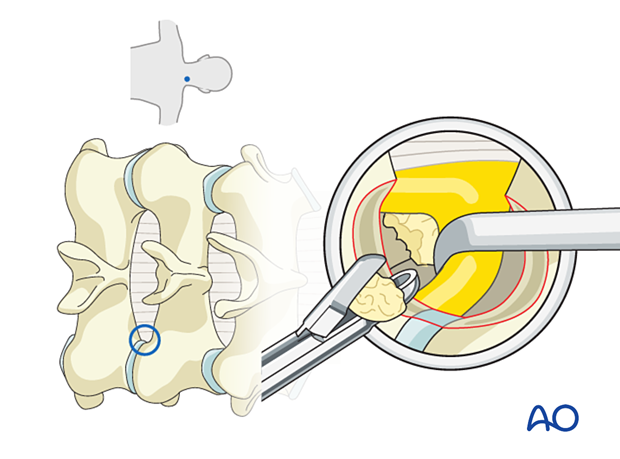
In cases of posterolateral disc herniation, pituitary rongeurs can be used to extract the fragment.
7. Endoscope removal and closure
Hemostasis is achieved with hemostatic agents or bipolar cautery.
The endoscope is slowly removed. Any muscular bleeding should be identified and cauterized.
The fascia is typically closed using an interrupted suture.
Standard multilayer closure of subcutaneous layers and skin is performed.
A drain may be used if necessary.
8. Aftercare
The patient can usually be discharged on the day of surgery or the following day.
Cervical immobilization is not required.
Patients may feel incisional or muscular pain that usually subsides within a few days.













