Posterior Screws - With direct vertebral body derotation
1. Introduction
The aims of surgery are to:
- improve the spinal curve
- improve the three dimensional alignment of the spine
- prevent progression of the curve in the future
- improve cosmesis
- reduce pain
- optimize pulmonary function
- maintain neurological integrity
This is achieved by correction of the deformity and creation of a solid arthrodesis of the deformed part of the spine.
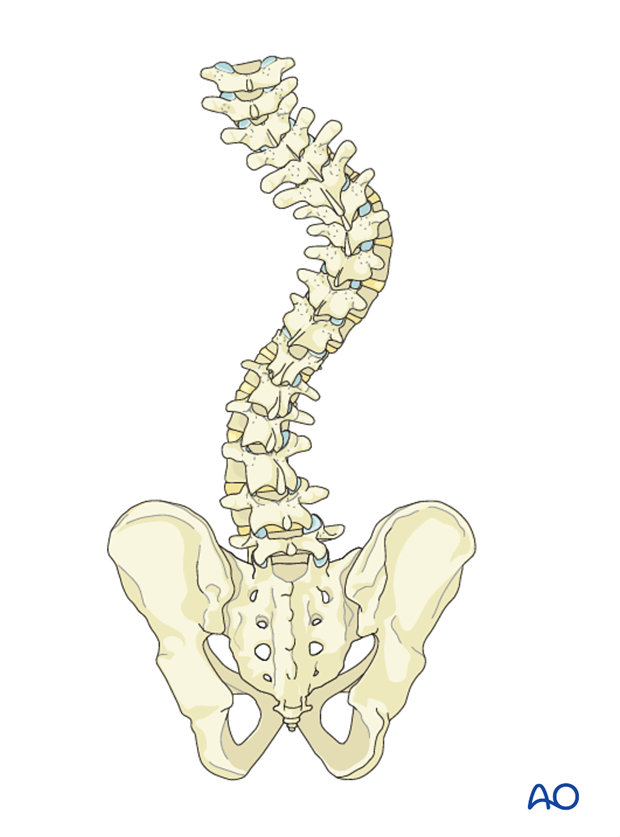
For this procedure we will assume a right thoracic and a left lumbar curve.
Details on selection of fusion levels can be found here.
2. Approach and preparation
The procedure is performed through a posterior approach with the patient in the prone position. The lengths of the incision will depend on the levels being fused.
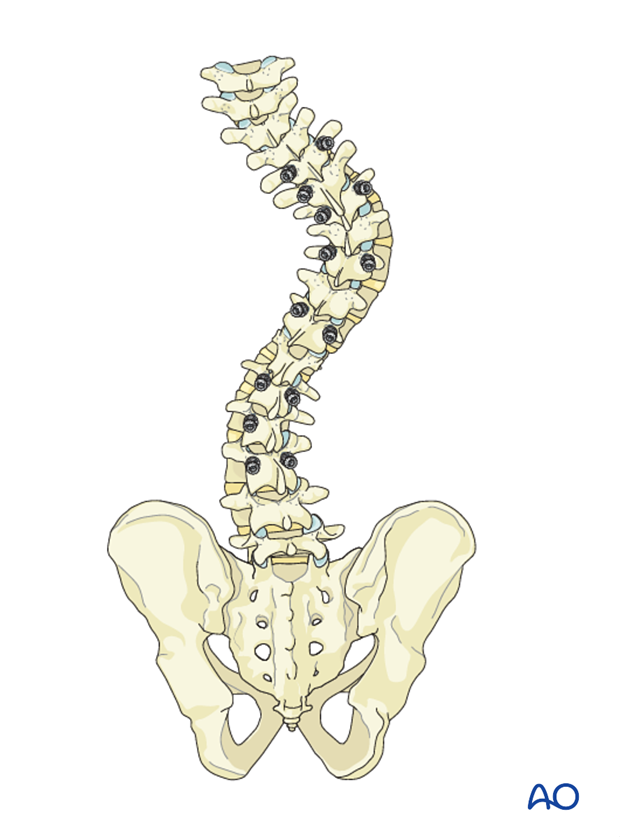
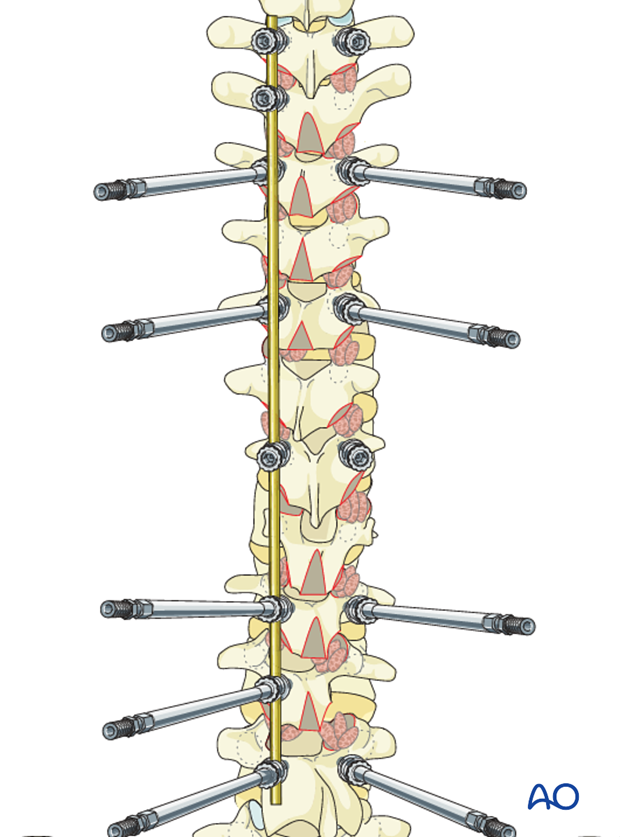
3. Pedicle screw insertion
Pedicle screw density would depend on surgeon's preference and preoperative planning. Typically less screws are utilized on smaller and more flexible curves, while more screws are utilized on larger and stiffer curves up to a maximum of segmental screws bilaterally.
4. Release
Indications for release
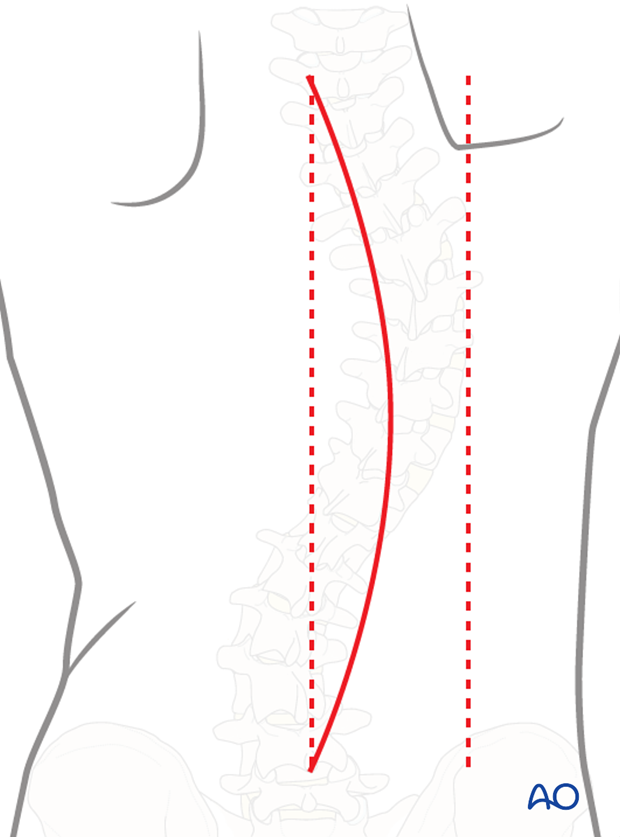
Depending on flexibility findings, the release can be carried out only at the apex of the curve, which is usually the stiffest, or the whole length of the instrumented spine.
A release is generally performed if the spine cannot easily align to the rod during surgery. This can be predicted preoperatively based on the bending X-ray. For stiff curves, fulcrum bending X-ray and the traction X-ray under general anaesthesia is the method of choice for determining flexibility.
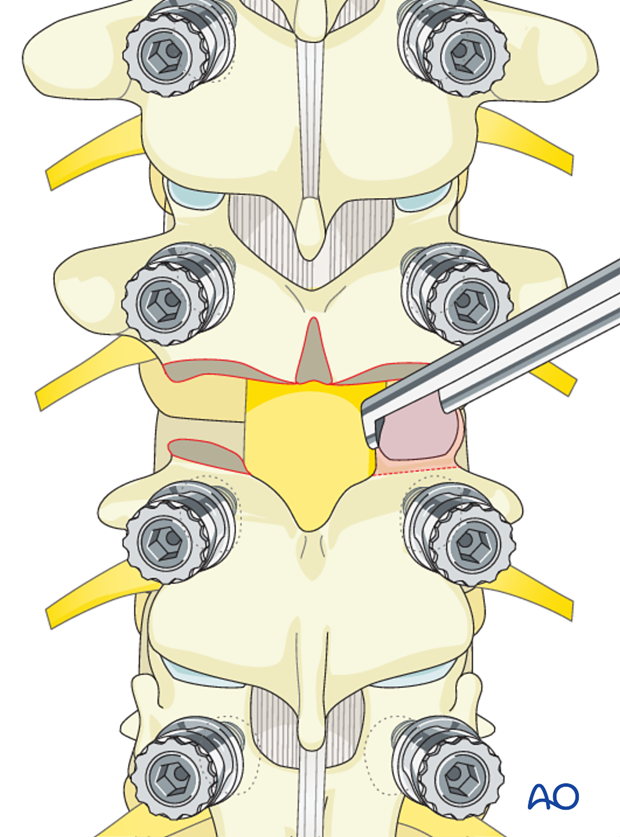
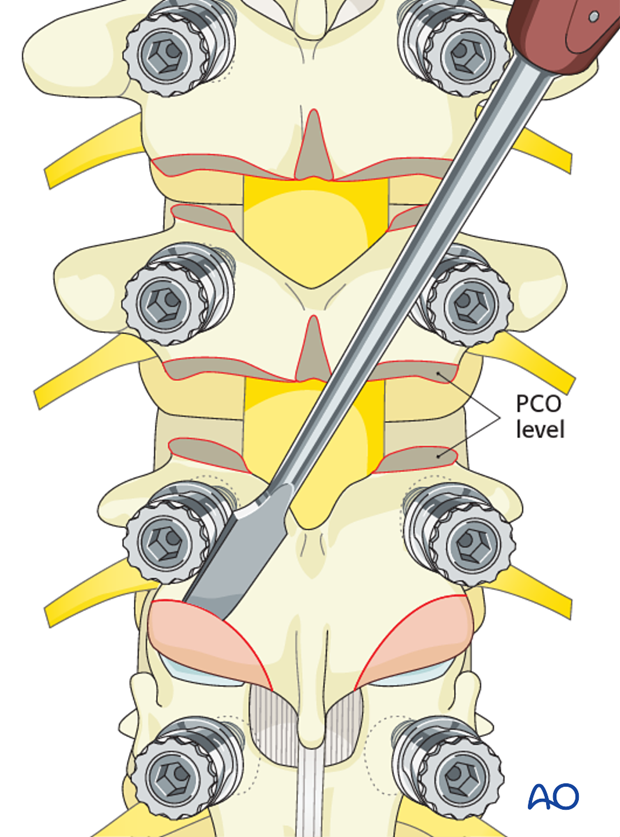
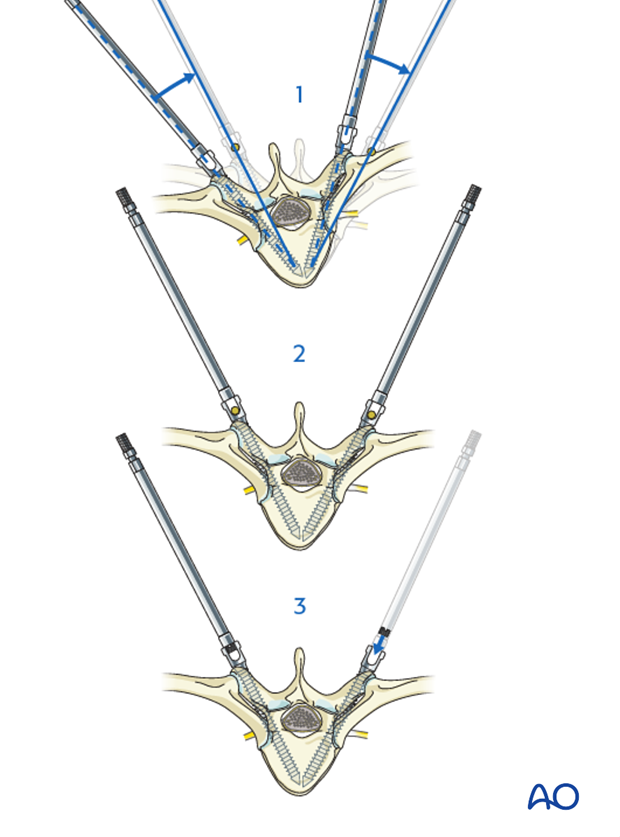
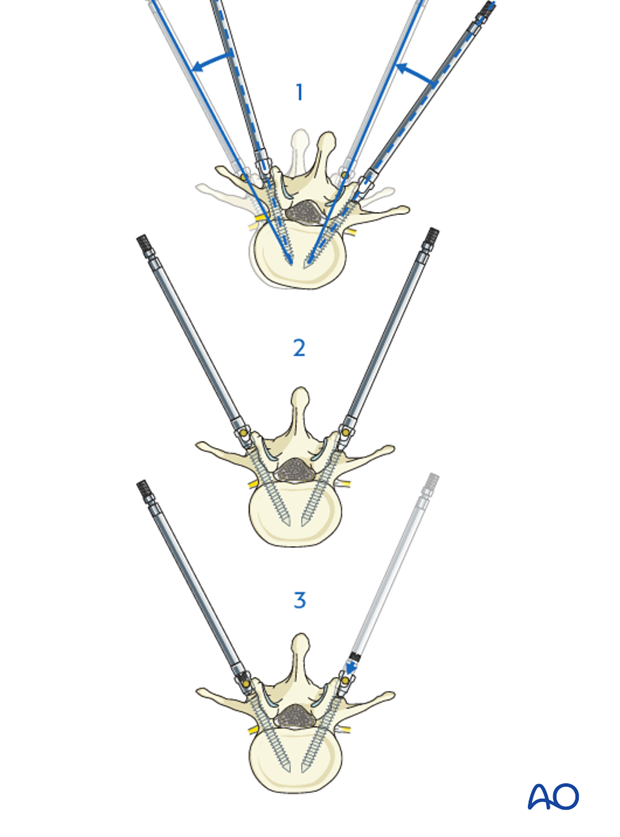
A soft tissue release can be performed by removal of the interspinous ligaments along with the midline ligamentum flavum of the apical regions of the deformity. If additional release is desired, then formal Posterior Column Osteotomy (PCO) can be performed at the same levels. PCO is also called SPO (Smith-Petersen osteotomy) or Ponte osteotomy. The shaded area to the left outlines the bony resection performed during a PCO.
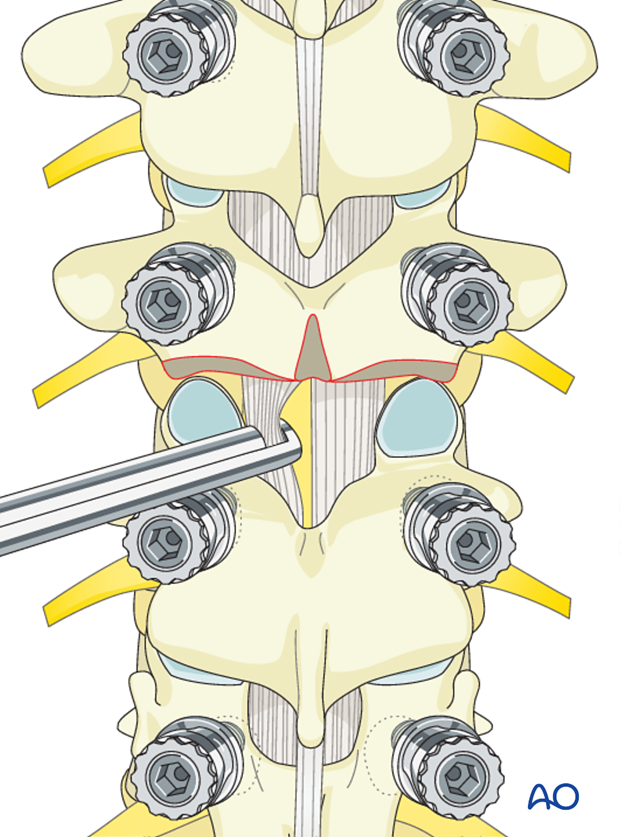
All posterior releases begin by resecting the inferior aspect of the spinous process, followed by removal of the interspinous ligament utilizing a standard rongeur.
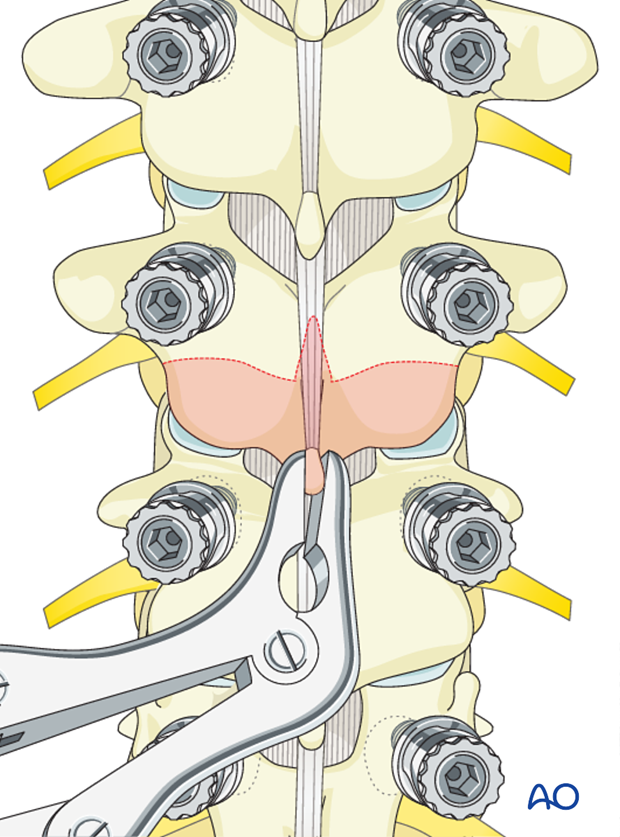
Removal of the 3-5 mm of the inferior aspect of the inferior facet joint is performed at each level of the planned fusion using an osteotome.
The ligamentum flavum is removed with a Kerrison rongeur beginning in the midline and exiting lateral until abutting against the medial aspect of the superior facet. It is important not to penetrate deeply against the dura.
Care should be taken not to tear the dura particularly on the concavity of the curve where the neuro tissues preferentially lie.
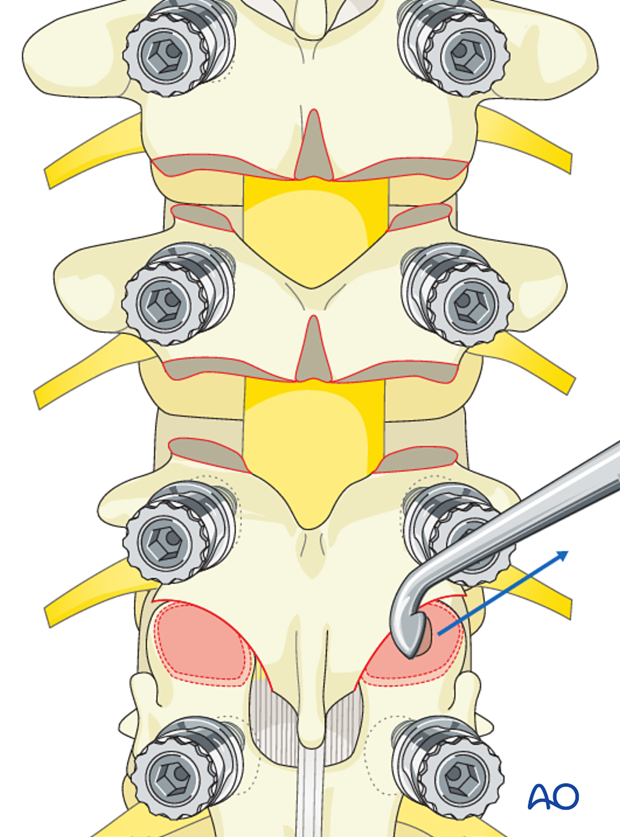
A Kerrison rongeur is utilized to remove the most cephalad portion of the superior articular facet exiting out lateral into the neuroforamen. This completes the PCO and is usually repeated at other levels.
Epidural bleeding within the neuroforamen is controlled with hemostatic agents and cottonoid packing.
5. Facet joint fusion
In cases where a PCO has been performed, the facet joint is already removed and this step ("Facet joint fusion") should be omitted.
The inferior articular facet is removed with an osteotome exposing the articular cartilage of the superior articular facet.
Remove the articular cartilage from the superior articular facet using a gouge or a curette.
Insert pieces of bone graft (autograft, allograft, or bone substitute) into the decorticated facet joint for arthrodesis.
These steps are repeated for all the levels on both sides.

6. Correction of the deformity
Left rod
The left rod is bent to the appropriate thoracic kyphosis as preoperatively planned and lumbar lordosis corresponding to the levels to be fused.
The amount of thoracic kyphosis bent into the left rod will be based on:
- curve size
- curve flexibility
- number and purchase of bone anchors
- size and material of the rod utilized
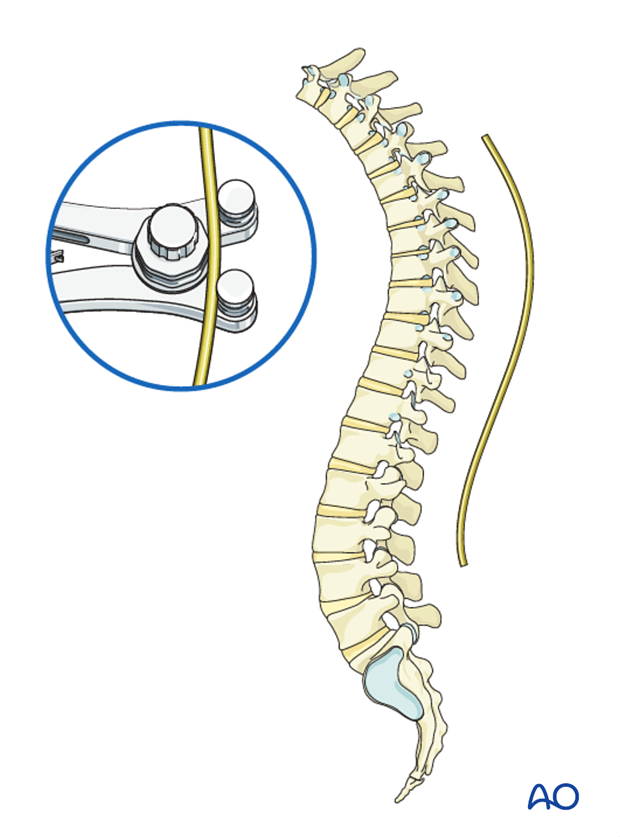
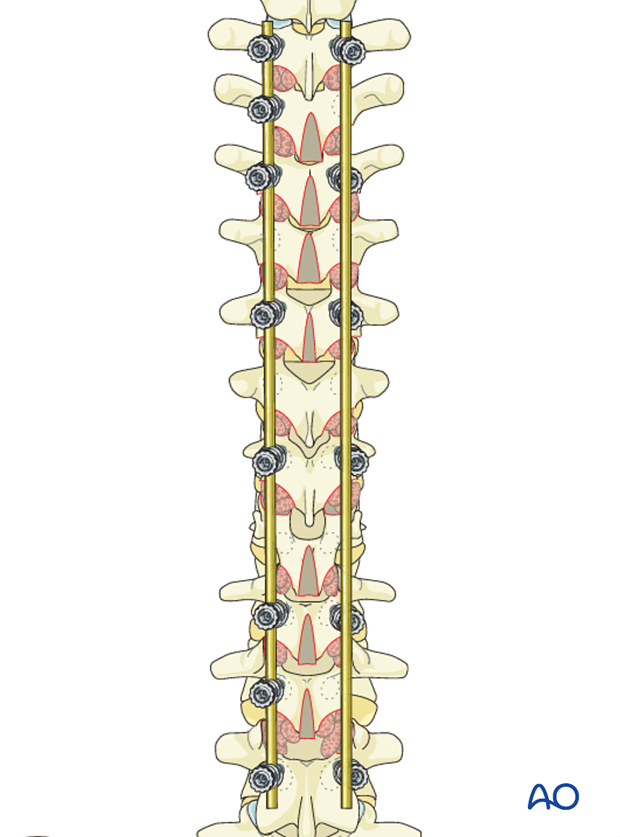
Starting with the most cranial screw the rod is inserted sequentially into the screws on the left side of the thoracic and right side of the lumbar curve conforming to the two deformities without being locked.
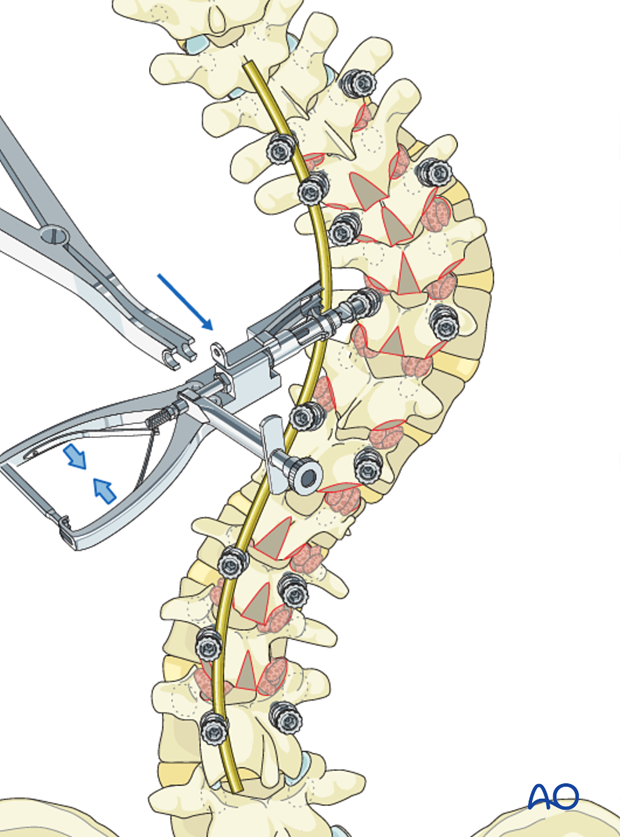
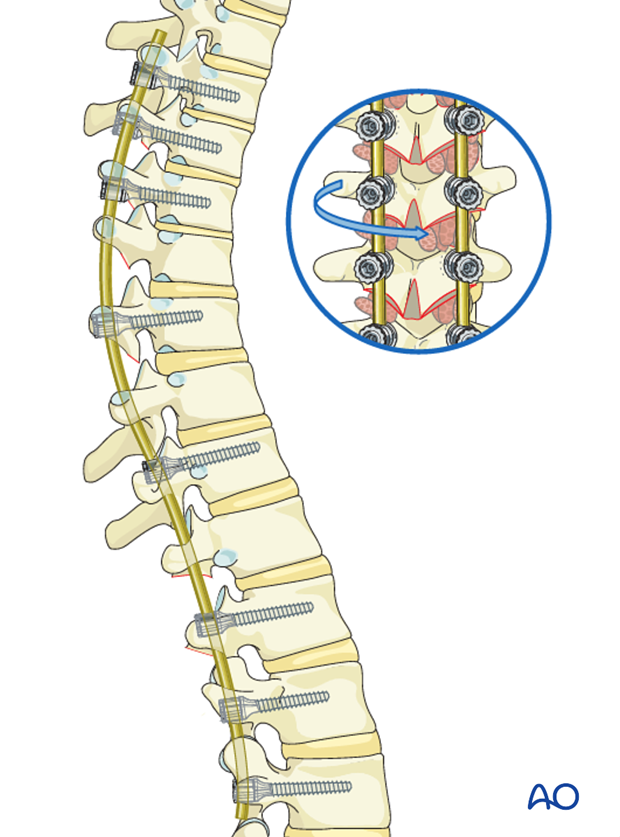
Rod holders are then applied onto the rod and the rod is rotated 90° around its axis correcting the scoliosis, and restoring the kyphosis in the thoracic spine and the lordosis in the lumbar spine.
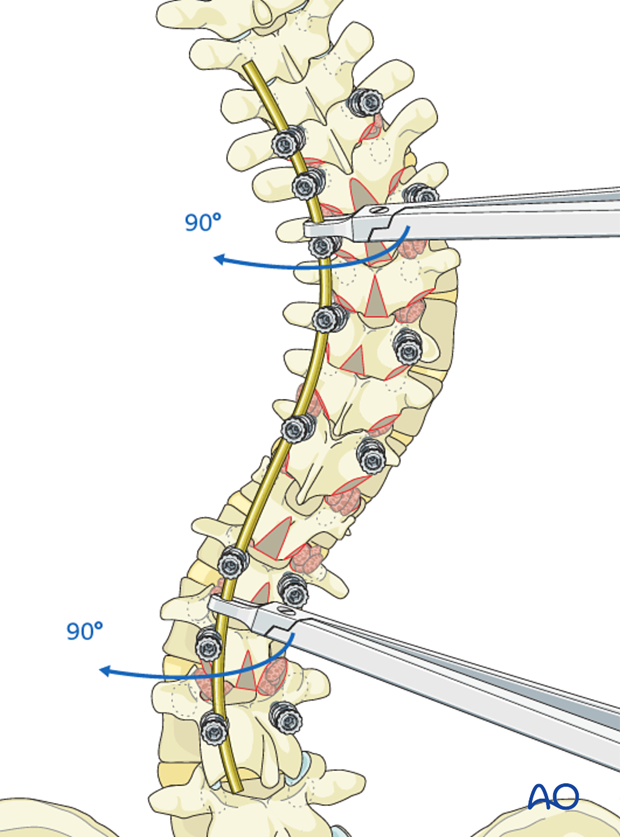
The rod is locked to the 2-3 most caudal screws to prevent the rod from rotating back. The other screw heads are kept unlocked.
Derotation of the spine
Vertebral screw derotation extenders are applied to the three periapical screw heads on the concavity and convexity.
An apical derotational maneuver is then performed on the thoracic curve to simultaneously translate the apical vertebrae dorsally and medially to meet the kyphotically contoured concave rod. The screws are then sequentially locked to this rod from the ends to the apex.
Secondary, an apical derotation maneuver is performed in the lumbar curve to simultaneously translate the lumbar apex medial and ventral to create increased lumbar lordosis while correcting the scoliosis.
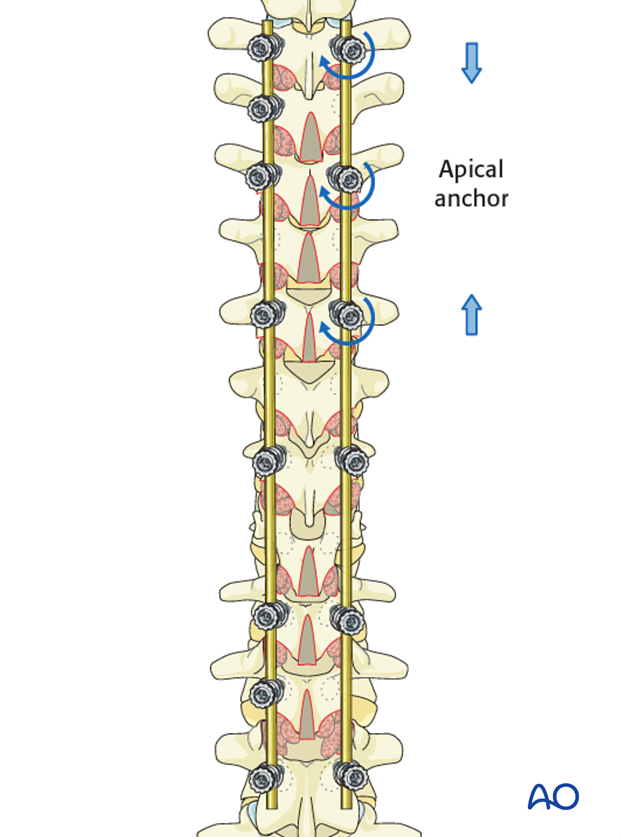
Concave distraction
Holding the spine in a derotated position, distraction is performed starting at the apex pushing caudal against the lower screws while pushing cranial against the upper screws. After the distraction is performed. Each set screw is locked down to hold the correction.
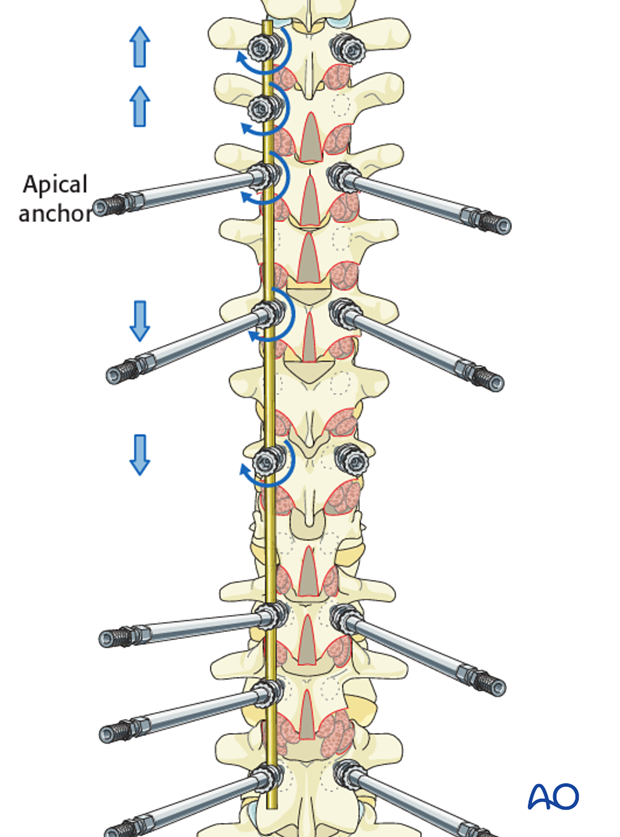
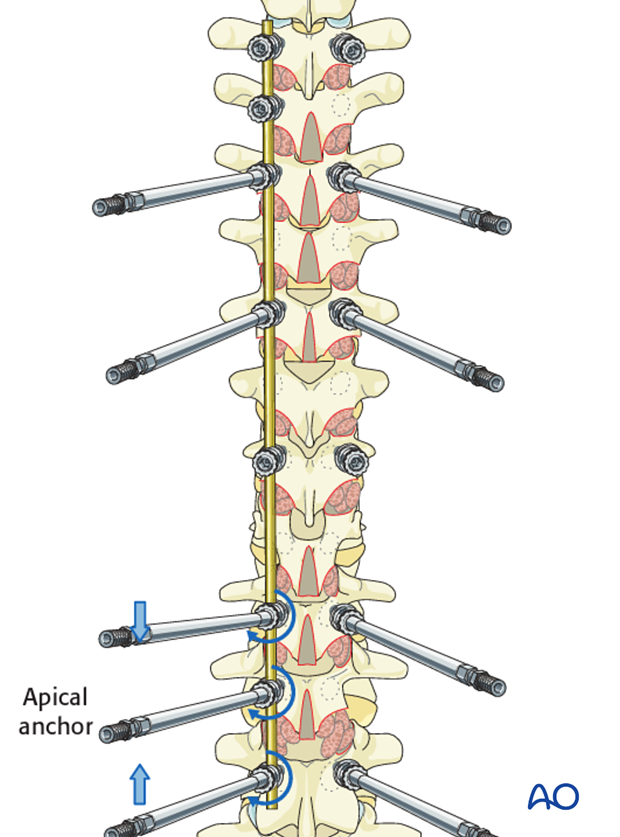
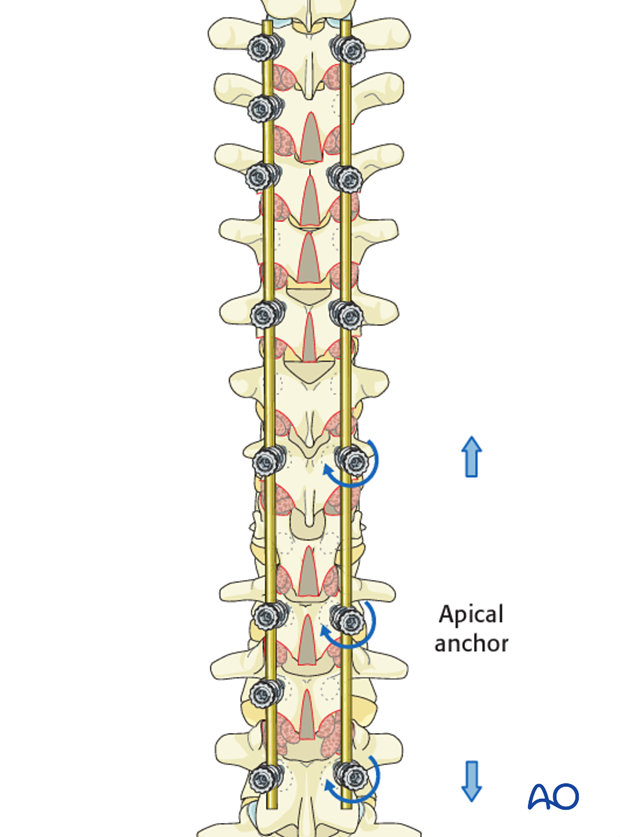
Convex compression
After locking the apical screw to the rod, the lumbar convex screws are compressed towards the apical anchor to horizontalize each vertebra and then locked in position.
Coronal benders applied for fine tuning the correction. Care is taken to apply only minimal stress in order to prevent bone-screw interface failure.
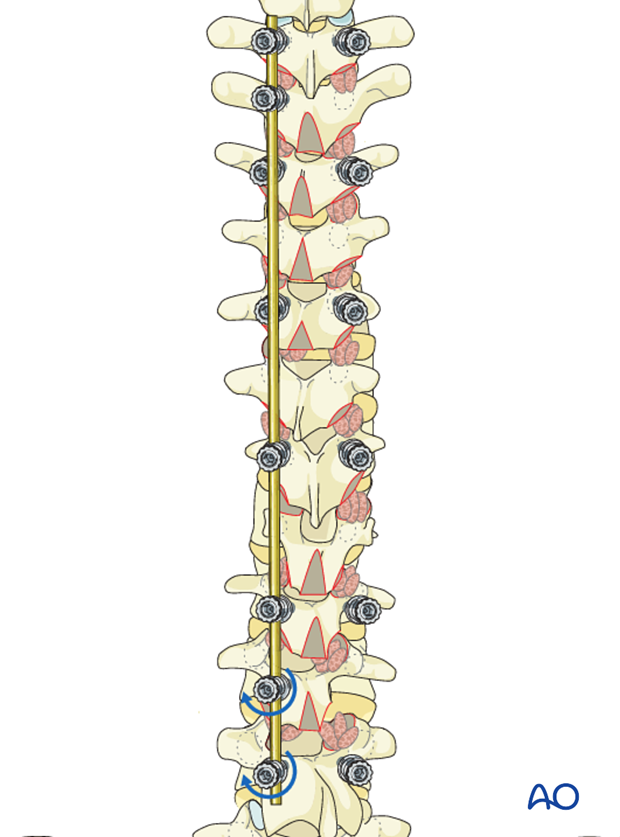
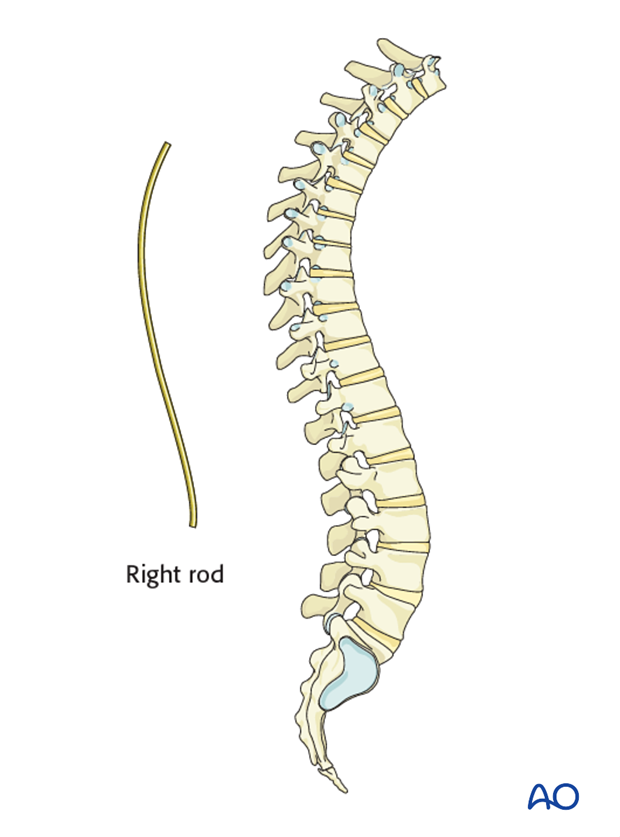
Right rod
The right rod is bent to the appropriate thoracic kyphosis with the appropriate transition into lordosis of the lumbar region as necessary.
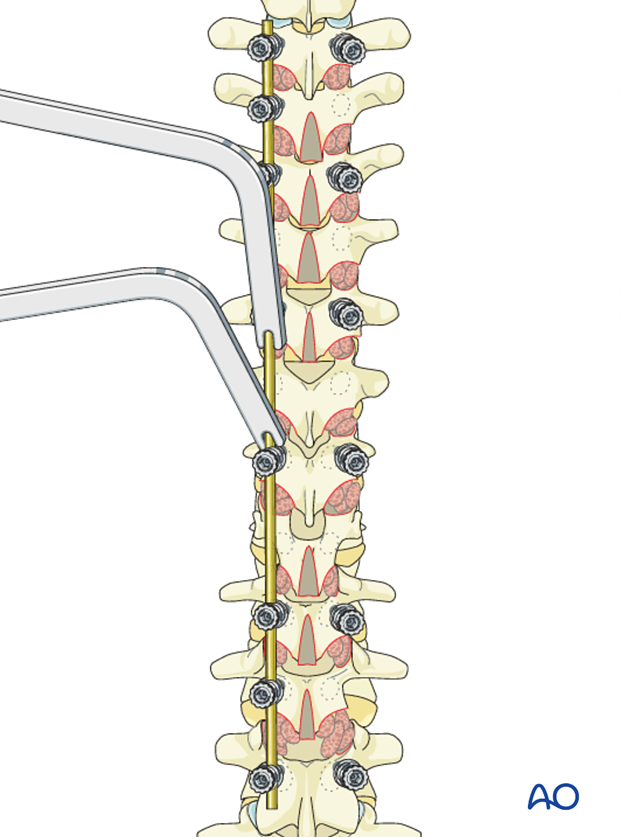
The rod is placed into the cranial thoracic screws on the right side and the set screws are applied loosely.
The distal end of the rod is then levered down using a rod holder while sequentially being attached to the distal screws.
This cantilever maneuver helps reduce the apical thoracic convex rotational deformity.
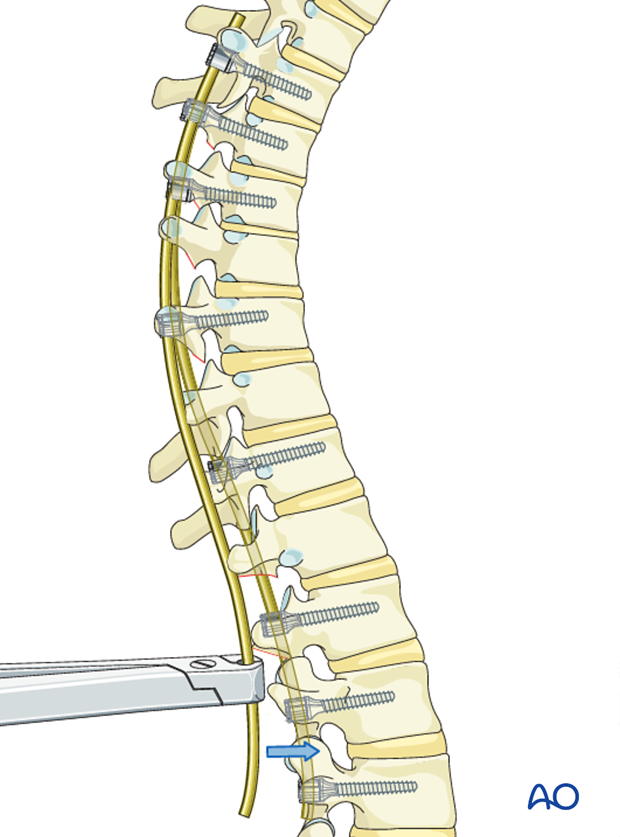
This maneuver will push the apical rib hump anteriorly, thereby achieving derotation of the apical segments.
Compression on convex side
After locking the apical screw to the rod, the convex thoracic screws are compressed towards the apical anchor to horizontalize each vertebra and then locked in position.
Concave distraction
Concave distraction is applied towards the locked apical anchor on the right sided rod.
It is recommended to obtain radiographic imaging in both planes to confirm optimal alignment at this point
Final fine tuning
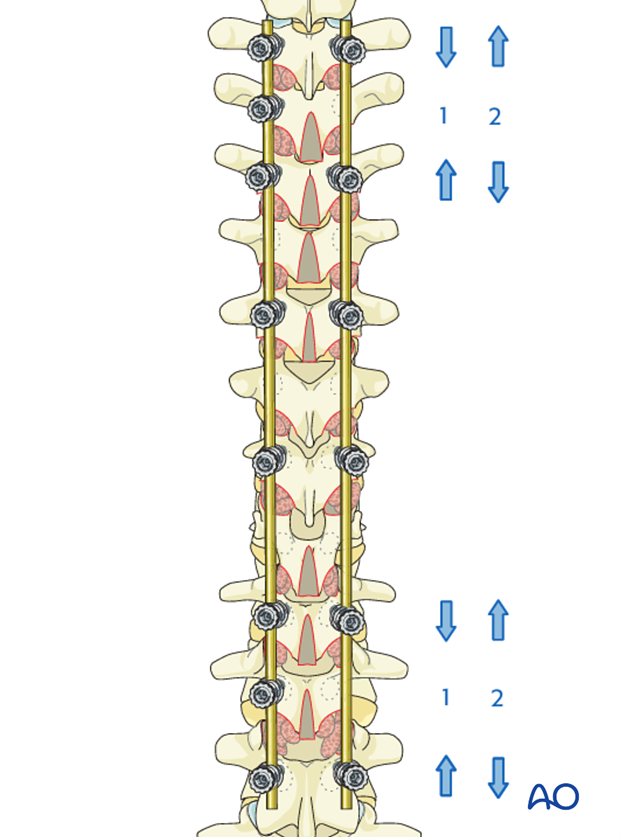
Compression (1) or distraction (2) is used at the cranial 2-3 levels in order to fine tune shoulder balance, and at the caudal 2-3 levels in order to optimize LIV position.
7. Spinal fusion
Decortication
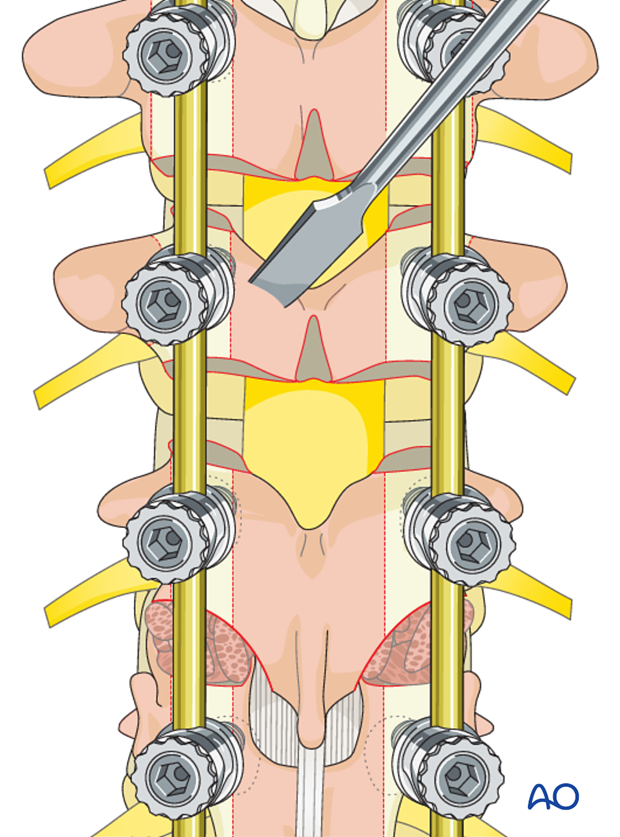
The laminae and the transverse processes are decorticated with an osteotome.
Care should be taken to always point the osteotome away from the spinal canal.
Alternatively, the decortication may be performed with a powered burr.
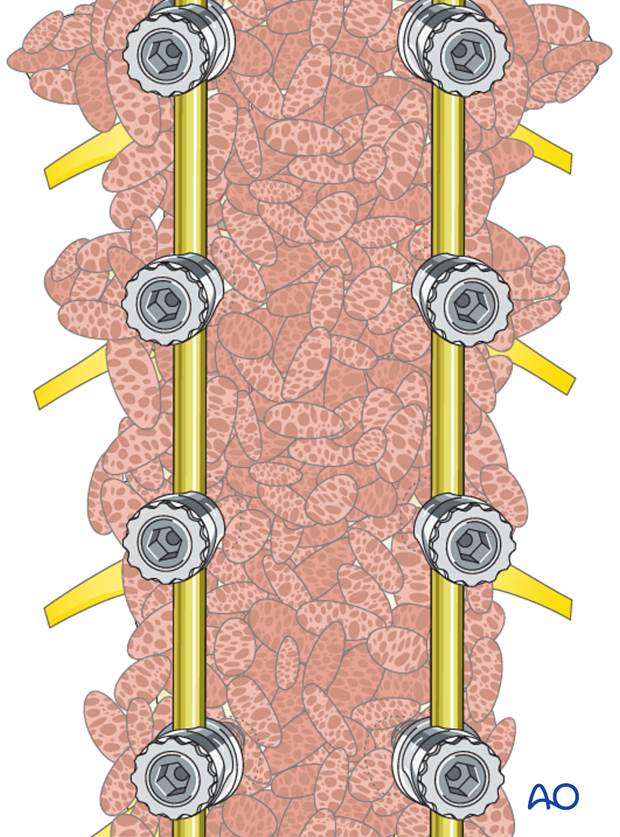
Bone grafting
Bone graft (allograft, autograft, or bone substitutes) is copiously placed over the entire decorticated area.
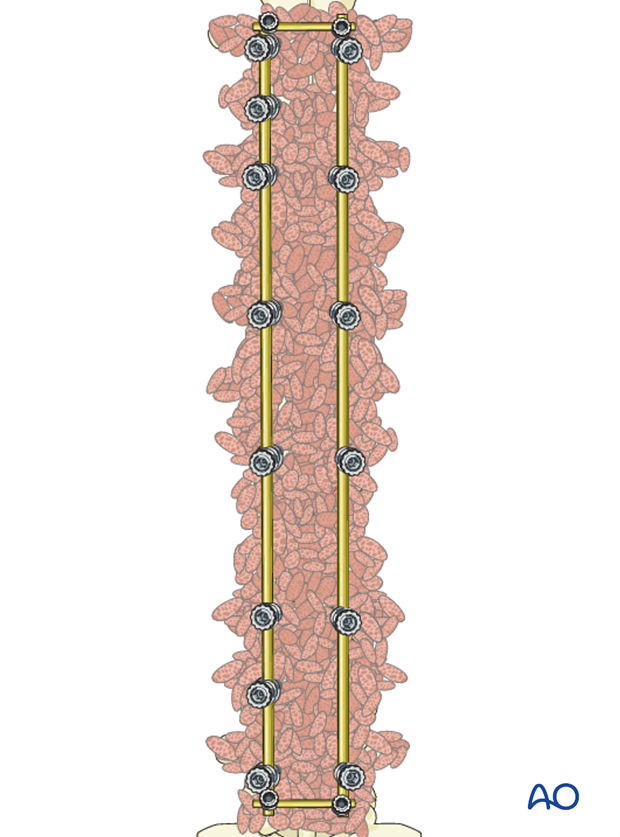
8. Transverse rod connectors (if desired)
Transverse connectors are optional in this technique based on overall construct stability.
9. Intraoperative imaging
At some point prior to wound closure intraoperative imaging should check:
- Fusion levels
- Screw position
- Overall coronal and sagittal correction and alignment
10. Aftercare following correction of spinal deformity
Immediate postoperative medication
Intravenous antibiotics are administrated for at least 24 hours, depending on hospital protocol. The use of an epidural pain catheter vs. intravenous patient controlled analgesia (PCA) are utilized for acute pain management.
Mobilization
Early mobilization out of bed, is preferably started the day after surgery. Generally a postoperative brace/orthosis is not required.
Postoperative imaging
It is appropriate to obtain upright PA and Lateral xrays of the patient at some point early postoperative either before the patient is discharged from the hospital or at the 1st postoperative visit as an outpatient
Restriction of activities
To allow the bone to heal and form a solid arthrodesis, some restriction of sports activities, especially contact sports, is usually advised for 6 months.
Postoperative complications
Early postoperative complications include:
- Postoperative wound infection
- Urinary tract infection
- Respiratory complications such as pneumonia
Late postoperative complications include:
- Pseudarthrosis with loss of correction
- Late deep wound infections
- "Adding on" which is progression of scoliotic deformity in the non-instrumented spine.
- Crankshaft phenomenon (progression of scoliotic deformity within the instrumented spine).
- Implant failure or other implant related complications
In the long term adjacent segment degenerations above and below the instrumented spine may occur.













