ORIF - Plate fixation
1. Principles
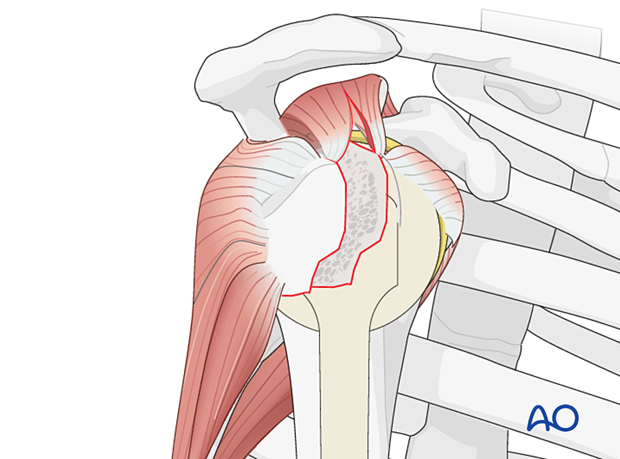
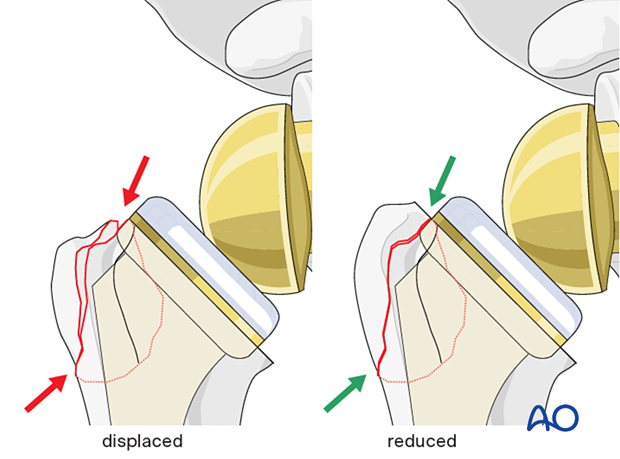
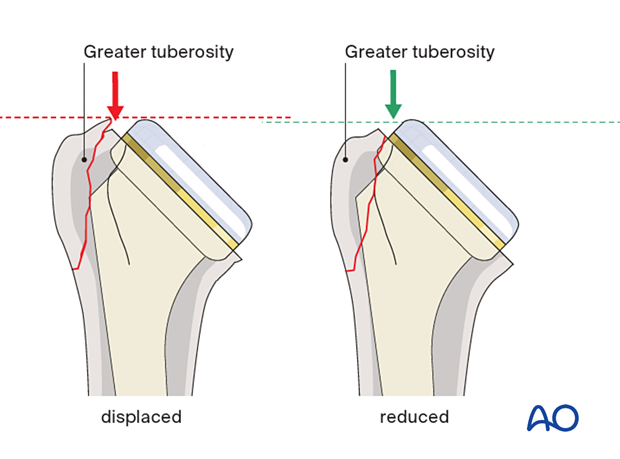
The greater tuberosity is typically displaced posterosuperiorly due to the pull of the rotator cuff.
The displaced greater tuberosity must be reduced and fixed stably.
More information about fixation of this fracture type can be found in the AO Surgery Reference Proximal humerus module.
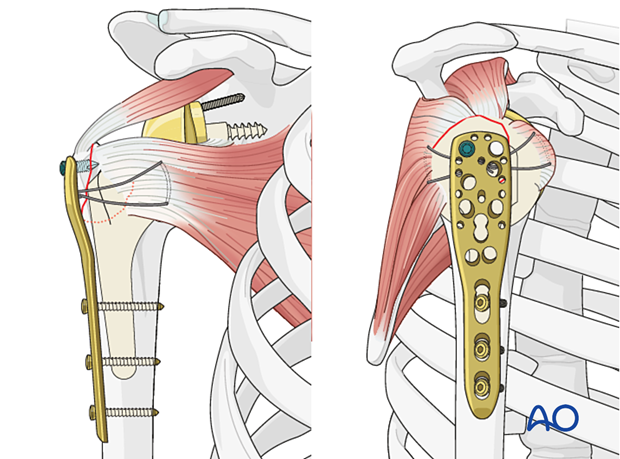
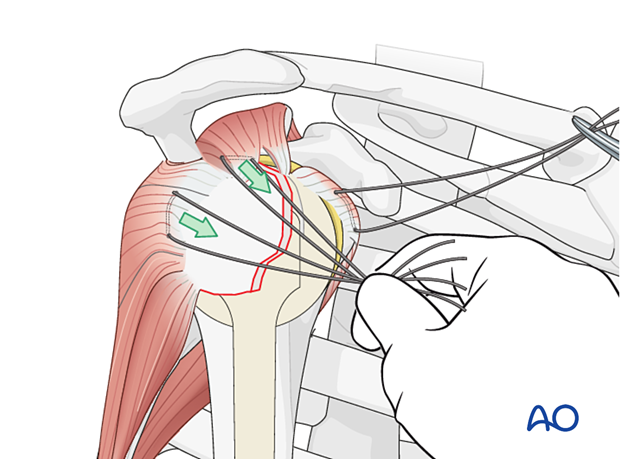
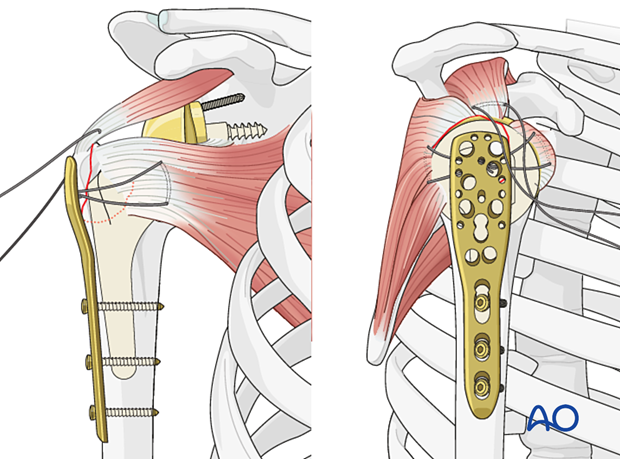
A plate can be used to buttress a greater tuberosity fragment to increase the stability of a suture fixation. This can be an anatomically pre-shaped plate or a one-third tubular plate.
An example of a completed construct is shown in this illustration.
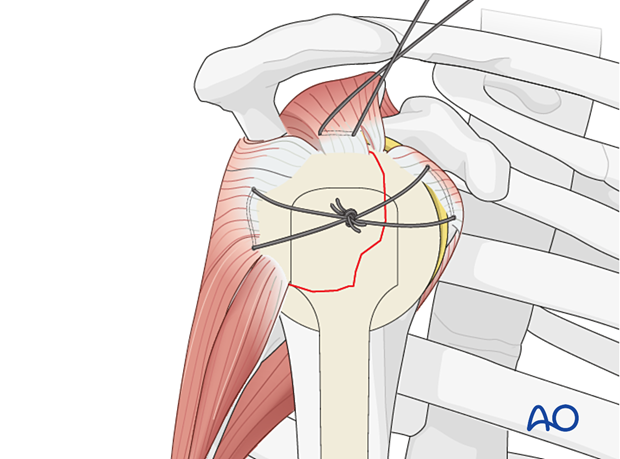
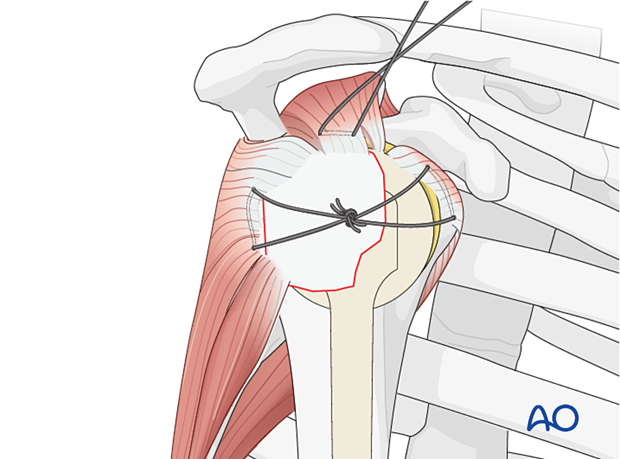
Suture reduction and fixation of the greater tuberosity
Sutures in the rotator cuff tendon insertions aid manipulation, reduction, and temporary fixation of a proximal humerus fracture.
Traction on the sutures helps achieve reduction. When tied, they bring the fragments together and stabilize them.
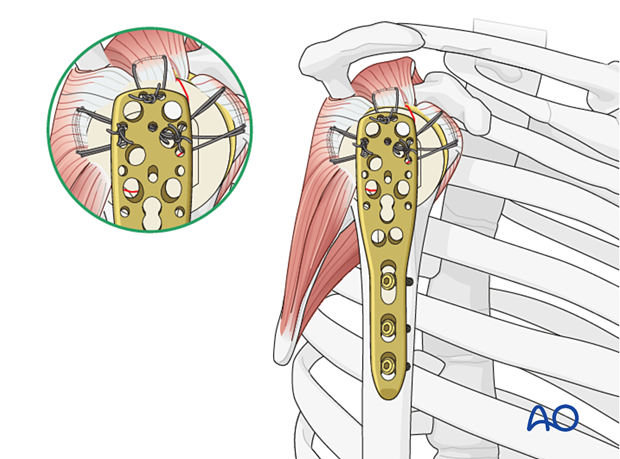
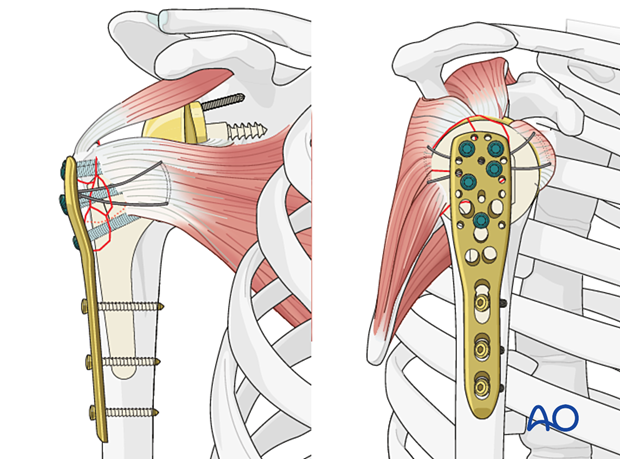
Neutralizing sutures in addition to plate and screws
Sutures placed through the insertions of each rotator cuff tendon increase stability, and should be used as well as the plate and screws, particularly for more comminuted and/or osteoporotic fractures. With osteoporotic bone, the tendon insertion is often stronger than the bone itself, so that sutures placed through the insertional fibers of the tendon may hold better than screws or sutures placed through bone.
This form of fixation was referred to as a “Tension band suture fixation”. We now prefer the term “Neutralizing suture” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
2. Patient preparation and approaches
Patient preparation
It is recommended that this procedure is performed with the patient in a beach chair position.
Patient positioning should be discussed with the anesthetist.

Approach
The approach of choice is the deltopectoral approach.

3. Reduction and preliminary fixation
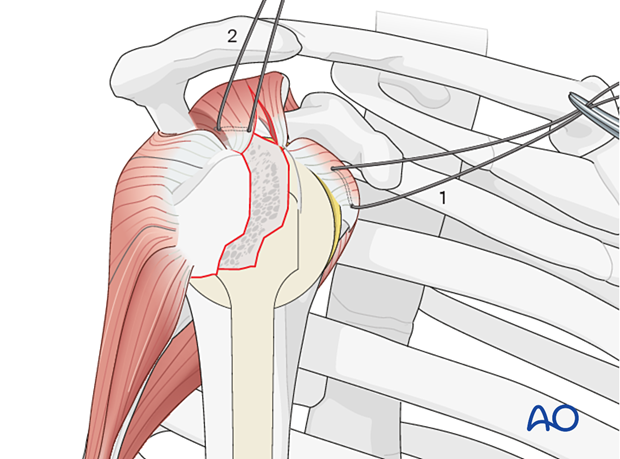
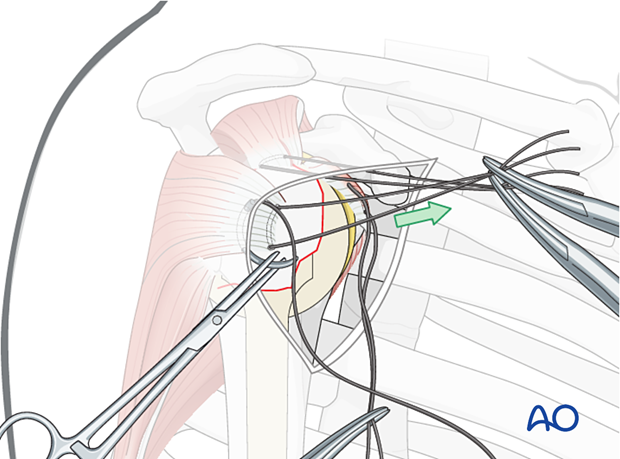
Place rotator cuff sutures
Subscapularis and supraspinatus tendonsSutures are inserted into the subscapularis tendon (1) and the supraspinatus tendon (2). The sutures are placed medial to the osteotendinous junction. These provide guides for reduction and temporary fixation of the greater and lesser tuberosities.
A suture is passed through the infraspinatus tendon insertion (3). This can be difficult. Traction on the previously placed sutures will aid visualization of the infraspinatus tendon.
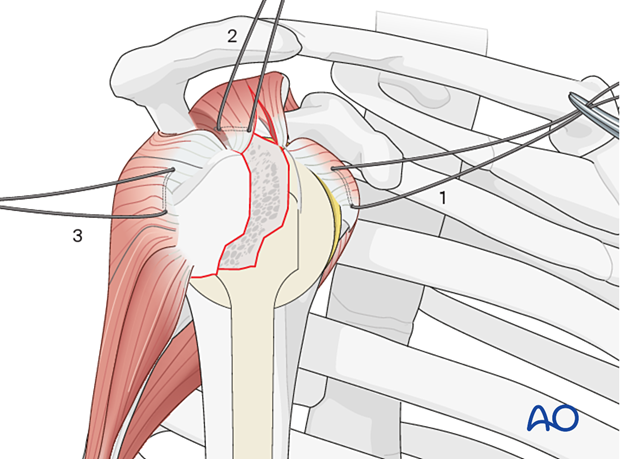
Anterior traction on the supraspinatus tendon helps to expose the greater tuberosity and infraspinatus tendon.
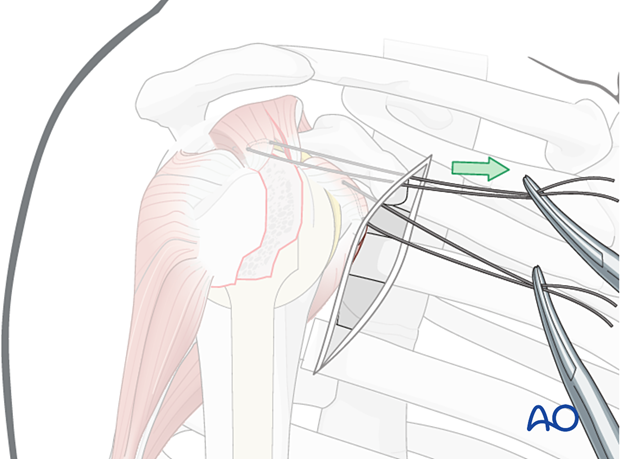
A preliminary traction suture is inserted into the visible part of the posterior rotator cuff.
Traction on the suture exposes the proper location for a suture in the infraspinatus tendon insertion. The initial traction suture may then be removed.
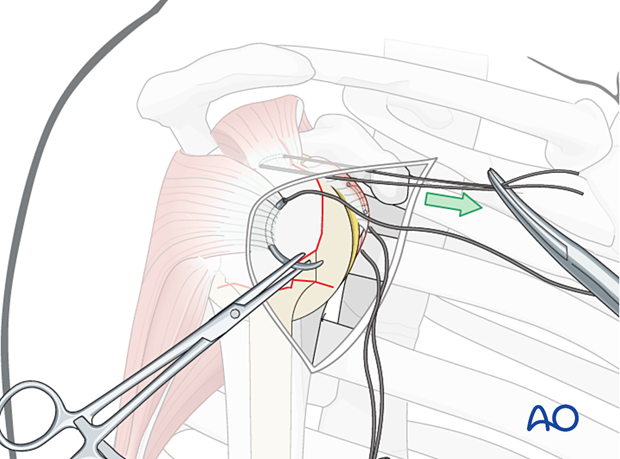
Reduce the greater tuberosity
The sutures in the supraspinatus and infraspinatus tendons are used to reduce the greater tuberosity.
Preliminary fixation of the greater tuberosity
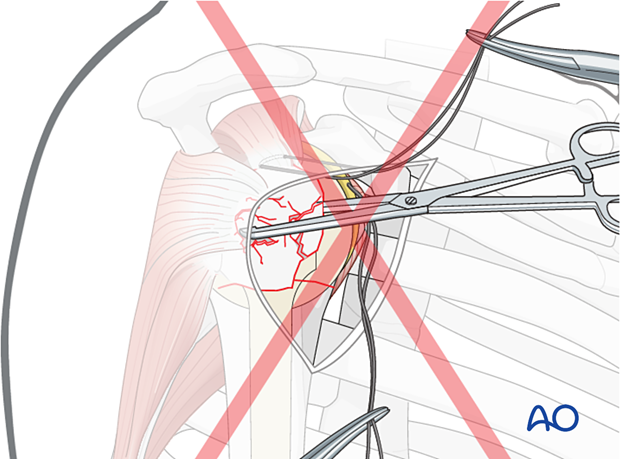
The transverse sutures are tightened and tied to achieve preliminary fixation of the greater tuberosity fragment.
Confirm reduction
After preliminary fixation the reduction is checked visually and with image intensification.
All fracture lines should remain closed without steps or gaps between the greater and lesser tuberosities during rotation of the arm. This should be further assessed by image intensification.
The AP x-ray should show the correct relationship between the prosthetic head and the tuberosities.
Specifically, the greater tuberosity should not project superiorly to the prosthetic head.
4. Plate fixation
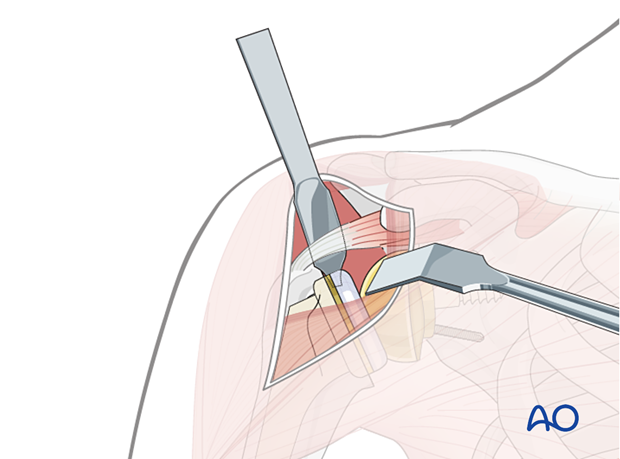
Attach the plate to the humeral shaft
The plate is fixed to the humeral shaft with a bicortical 3.5 mm cortical screw inserted through the elongated hole. More detail on this technique can be found in the AO Surgery Reference Proximal humerus module.
Preliminary plate position is confirmed with image intensification.
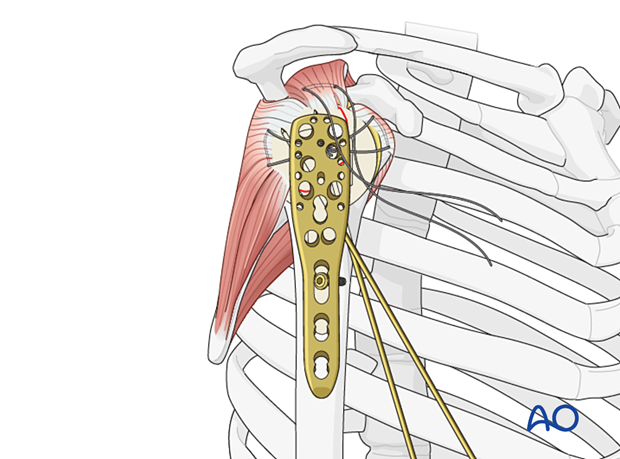
Insert additional screws into the humeral shaft
Insert one or two additional bicortical screws into the humeral shaft. As the stem needs to be avoided, drill obliquely anterior and/or posterior to the stem. It is preferable to position screws both anterior and posterior to the stem.
5. Supplementary rotator cuff tendon sutures
Secure the tendons of the rotator cuff (subscapularis, supraspinatus, infraspinatus) with additional neutralizing sutures through the small holes in the plate.
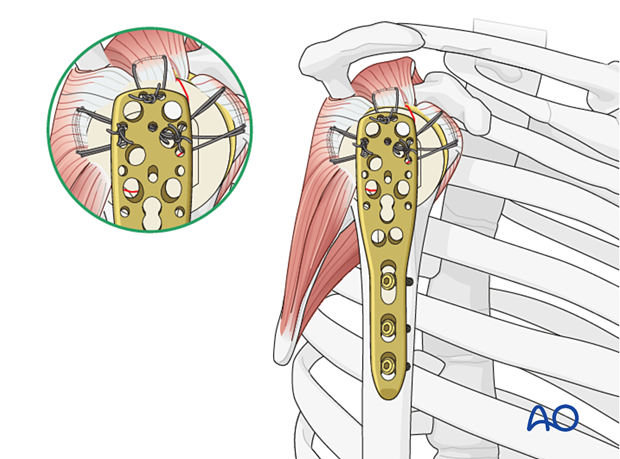
Proximal screw placement
If the greater tuberosity fragment is sufficiently large, proximal angle stable screws can be inserted to increase fixation stability.
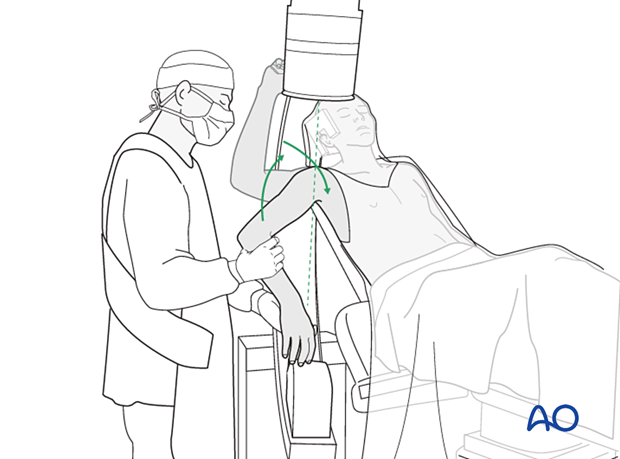
6. Final check of osteosynthesis
The C-arm must be directed to allow orthogonal views. Position the arm as necessary to confirm that reduction is satisfactory, fixation is stable, and the screws are of appropriate length.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.













