ORIF - Plate fixation
1. Principles
Introduction
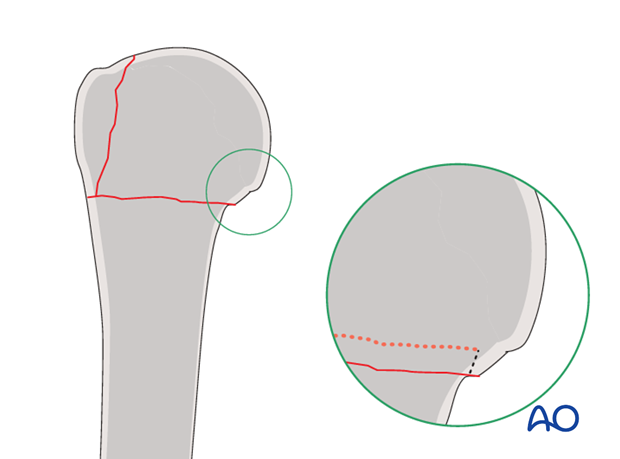
The displaced greater tuberosity must be reduced and fixed stably. The metaphyseal fracture may be left impacted, unless severe deformity must be corrected. This disimpacts the metaphyseal fracture, which will be fixed with the plate.
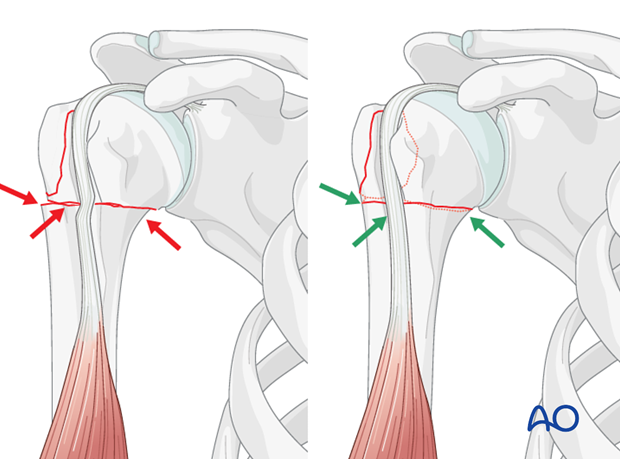
Proper reduction
The greater tuberosity is typically displaced posterosuperiorly due to the pull of the rotator cuff. The humeral head is typically rotated posteriorly due to the pull of the subscapularis tendon on the intact lesser tuberosity. Both aspects of deformity have to be corrected precisely. If there is a valgus/varus malposition of the humeral head this has to be corrected to allow a proper reduction of the greater tuberosity.
Suture reduction and fixation of the greater tuberosity
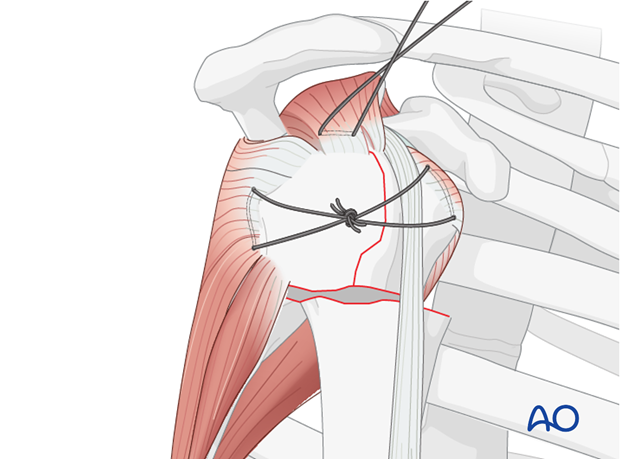
Sutures in the rotator cuff tendon insertions aid manipulation, reduction, and temporary fixation of a proximal humerus fracture.
Traction on the sutures helps achieve reduction. When tied, they bring the fragments together and stabilize them.
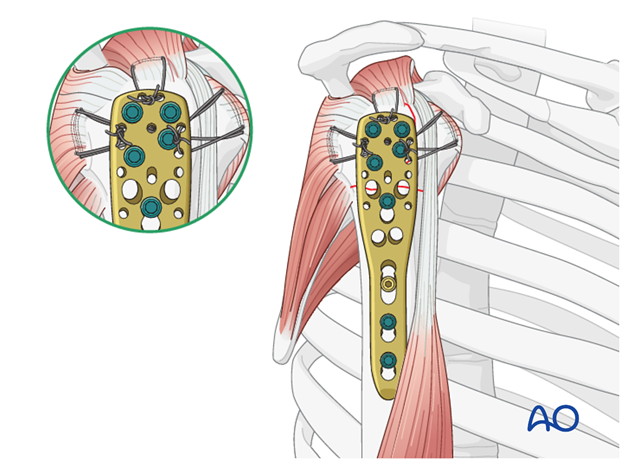
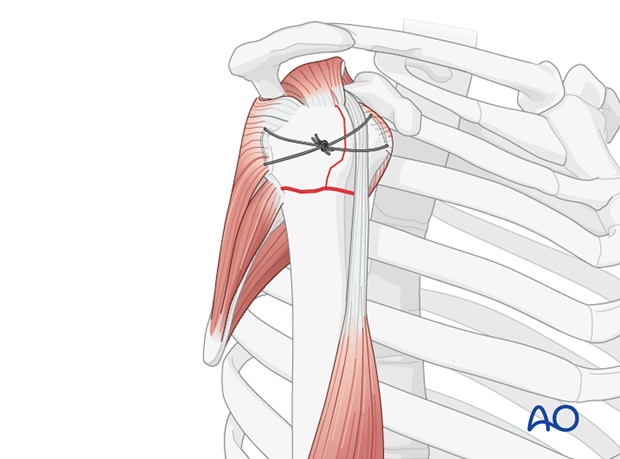
Neutralization sutures in addition to plate and screws
Sutures placed through the insertions of each rotator cuff tendon increase stability, and should be used as well as the plate and screws, particularly for more comminuted and/or osteoporotic fractures. With osteoporotic bone, the tendon insertion is often stronger than the bone itself, so that sutures placed through the insertional fibers of the tendon may hold better than screws or sutures placed through bone.
These additional sutures are typically the last step of fixation.
This form of fixation was referred to as a “Tension band suture fixation”. We now prefer the term “Neutralization sutures” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
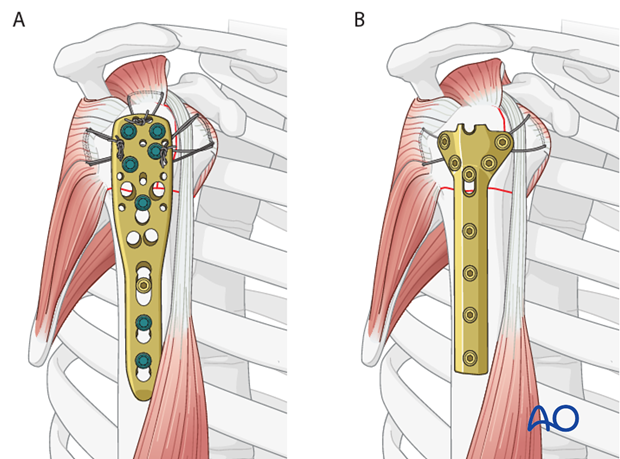
Angular stable versus standard plates
This procedure describes proximal humeral fracture fixation with an angular stable plate (A). Sometimes, these implants are not available. Standard plates provide an alternative option, for example the modified cloverleaf plate (B). Presently, the specific indications, advantages, and disadvantages of angular stable and standard plates are being clarified. There is some evidence that angular stable plate provide better outcomes. In addition to type and technique of fixation, the quality of reduction, the soft-tissue handling, and the characteristics of the injury and patient significantly influence the results. There is no evidence that the use of angular stable plates will overcome these other factors.
2. Patient preparation and approaches
Patient preparation
It is recommended to perform this procedure with the patient in a supine position (with the beach chair position as alternative).
Approaches
For longer plates consider a deltopectoral incision.
Otherwise, choose anterolateral or transdeltoid approach according to which is closest to the patient’s tuberosity fracture.
3. Reduction and preliminary fixation
Reduction
Sequence of repair:
- Reduce and fix the greater tuberosity to the humeral head (thereby converting the 3-part fracture into a 2-part situation)
- Reduce the proximal humeral fragment to the shaft and fix it.
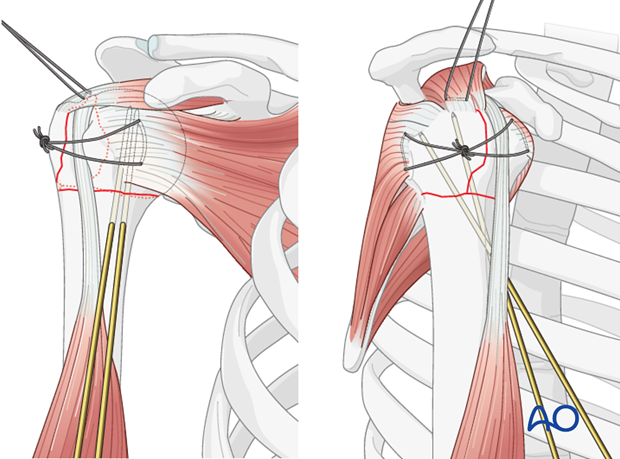
Place rotator cuff sutures
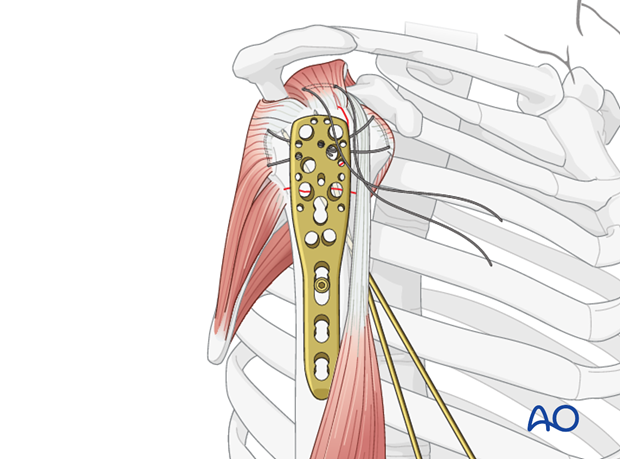
Subscapularis and supraspinatus tendon
Begin by inserting sutures into the subscapularis tendon (1) and the supraspinatus tendon (2). Place these sutures just superficial to the tendon’s bony insertions. These provide anchors for reduction, and temporary fixation of the greater and lesser tuberosities.
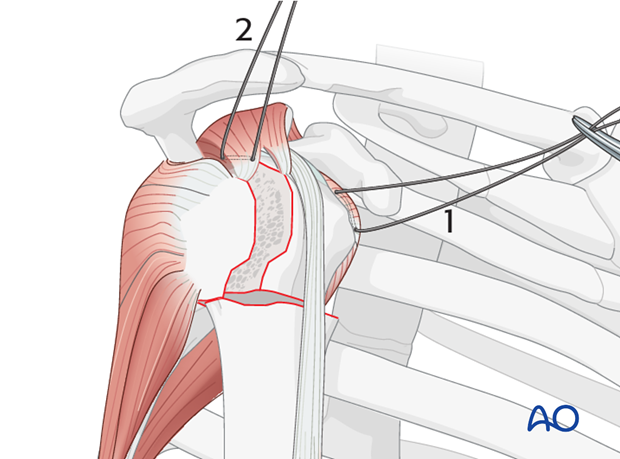
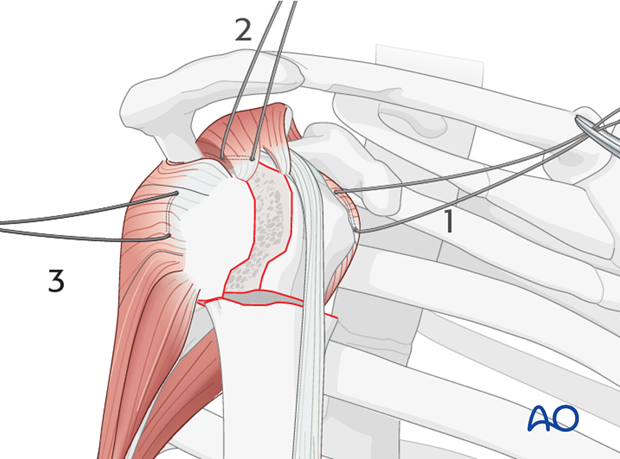
Infraspinatus tendon
Next, place a suture into the infraspinatus tendon insertion (3). This can be demanding, and may be easier with traction on the previously placed sutures, or with properly placed retractors.
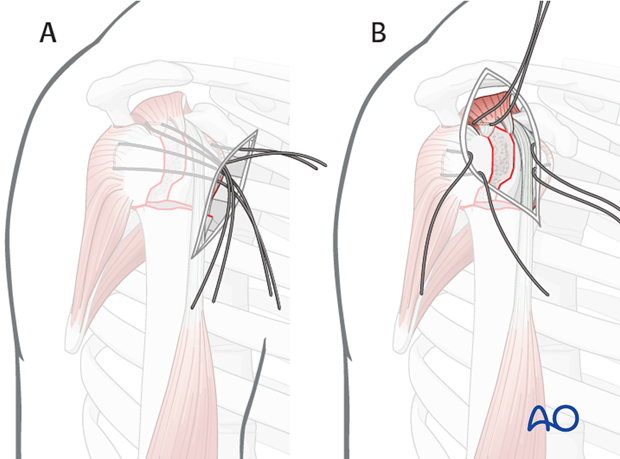
Variations depending on the approach chosen
Inserting sutures into the infraspinatus tendon is easier with a lateral approach. A) shows a deltopectoral approach and B) an anterolateral (transdeltoid) approach.
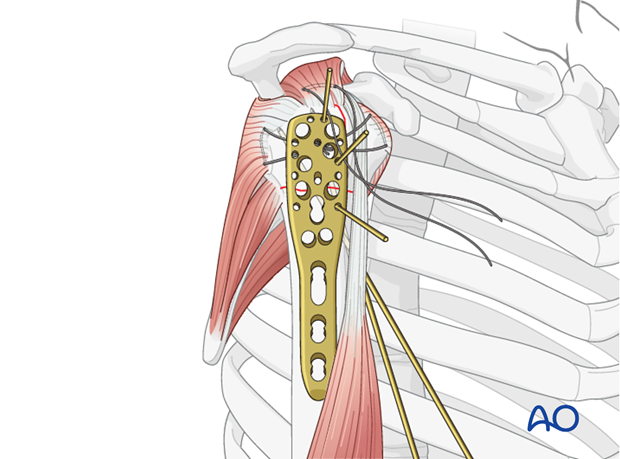
Use of stay sutures
Anterior traction on the supraspinatus tendon helps expose the greater tuberosity and infraspinatus tendon.

Insert a preliminary traction suture into the visible part of the posterior rotator cuff …
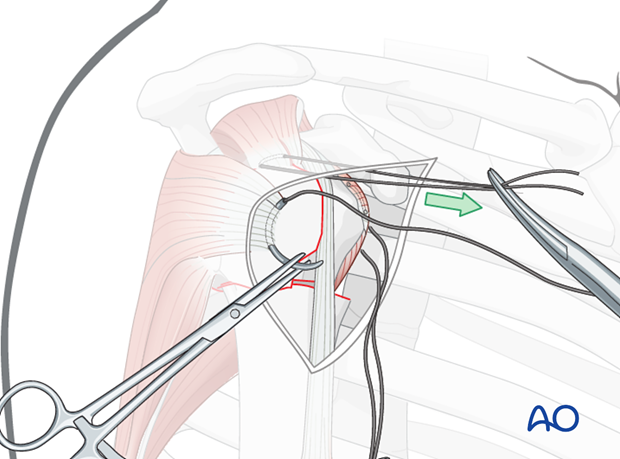
… and pull it anteriorly. This will expose the proper location for a suture in the infraspinatus tendon insertion. Then the initial traction suture is removed.
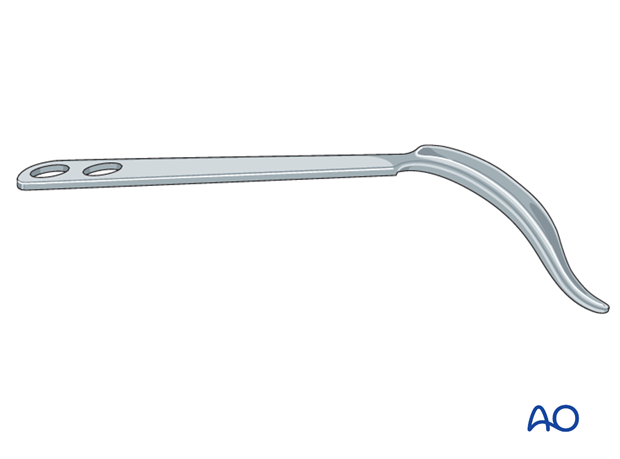
Pearl: larger needles
A stout sharp needle facilitates placing a suture through the tendon insertion.
Pearl: use of retractors
Use of blunt, curved Hohmann retractors underneath the deltoid muscle can be helpful to expose the humeral head.
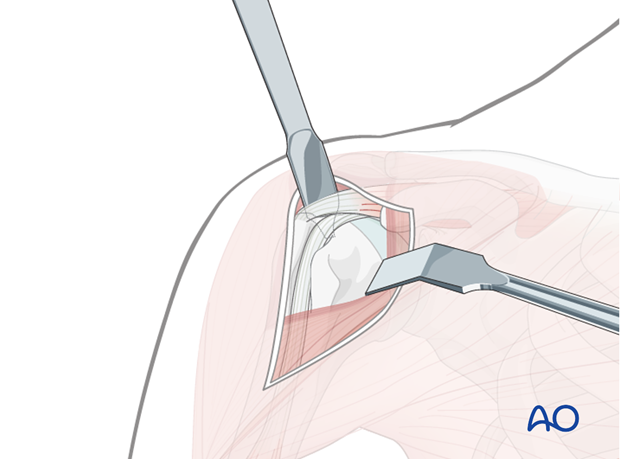
Similarly, a so-called delta retractor may improve deltoid retraction.
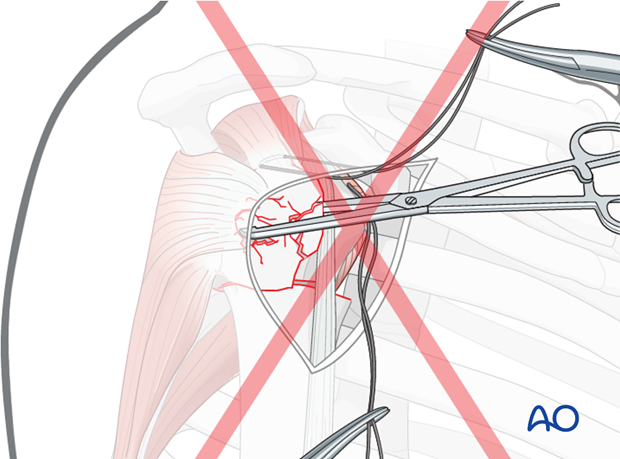
Pitfall: use of forceps or clamps in osteoporotic bone
Grabbing bone fragments with a forceps or clamp will typically increase comminution of osteoporotic bone. This should be avoided by using sutures as “handles” for manipulation and reduction.
Reduce the humeral head
Correct the valgus impaction by elevating the displaced proximal humeral segment. The required force may vary according to the degree of impaction.
Various techniques can be used to lift the humeral head such as:
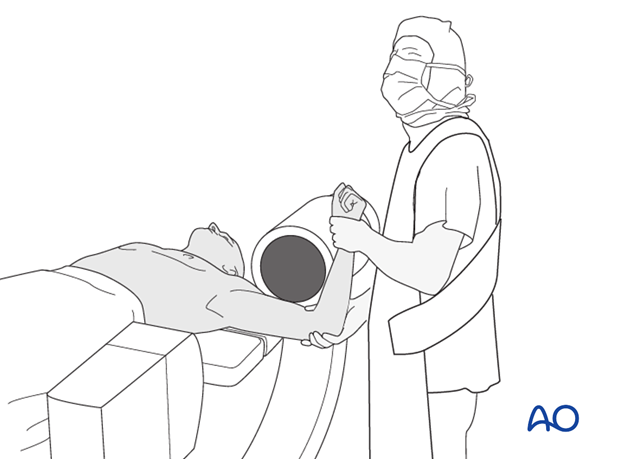
A) Digital pressure
B) Use of a blunt periosteal elevator (as illustrated)
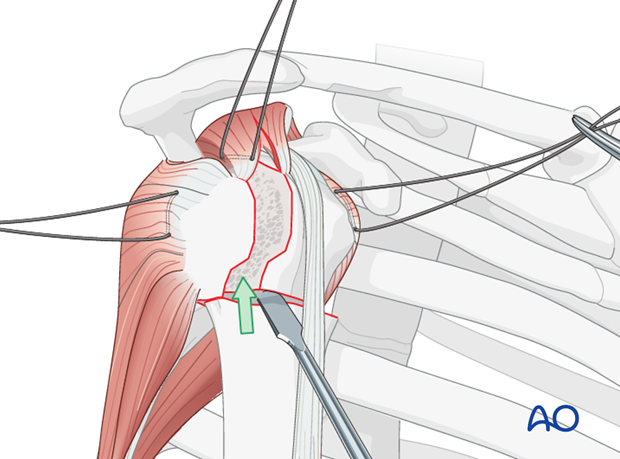
C) Leverage. A varus force can be applied to the humeral shaft. This can be achieved by using a fulcrum (eg, the surgeons fist, as shown, or a roll of towels) in the axilla.
D) Combination of direct manipulation and leverage.

E) If the fragments are jammed together, disimpaction with a bone punch may be required.
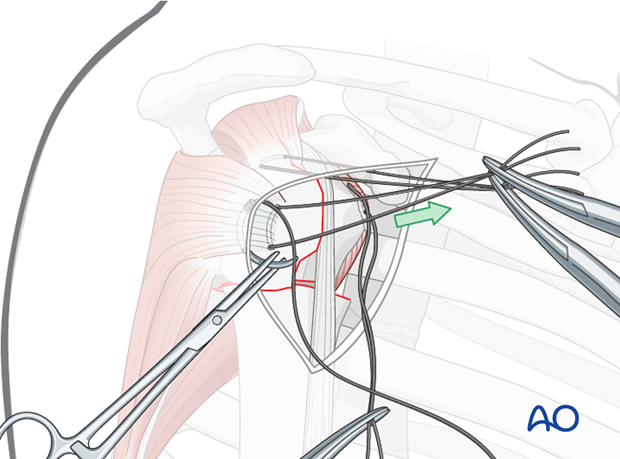
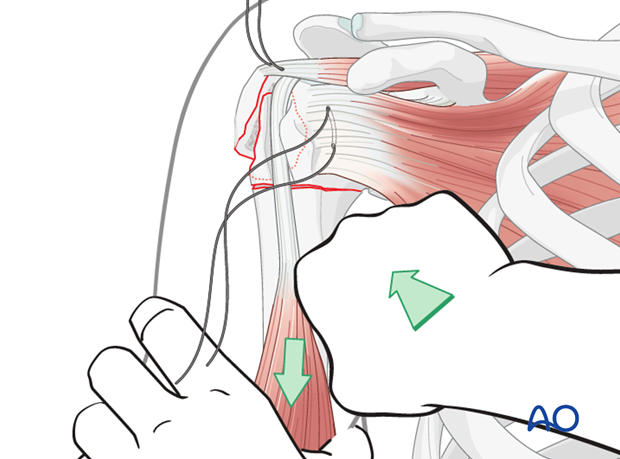
Reduce the greater tuberosity
Pull the sutures in the supra- and infraspinatus tendons in order to reduce the greater tuberosity.
Pearl: a periosteal elevator might be helpful in order to manipulate the greater tuberosity.
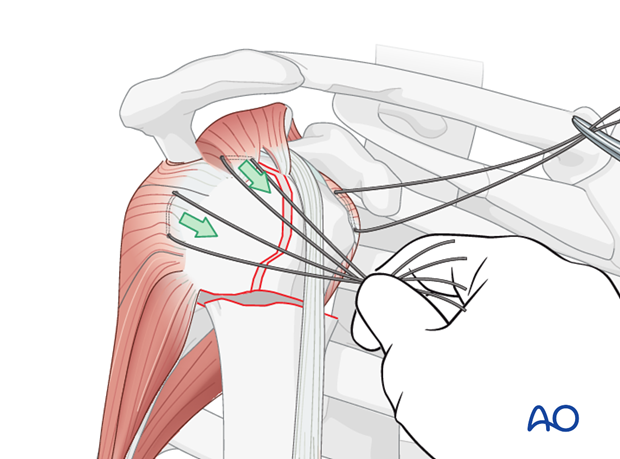
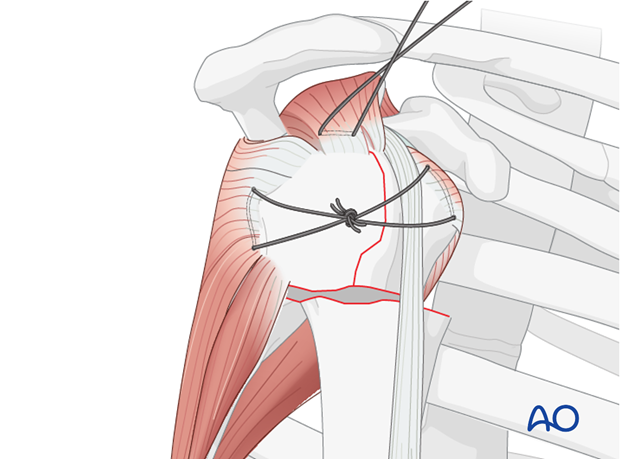
Preliminary fix the greater tuberosity
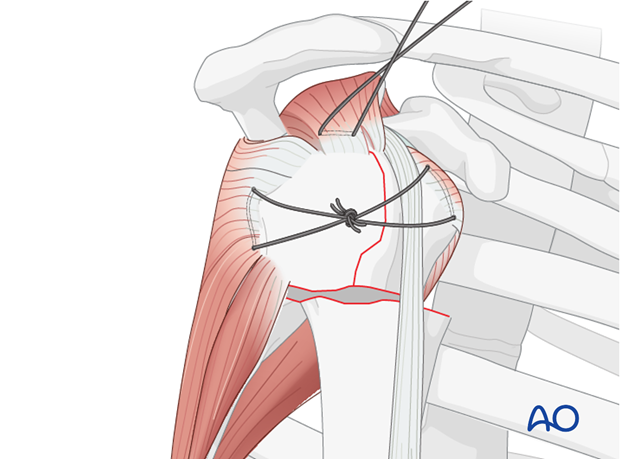
Tighten and tie the transverse sutures in order to preliminarily fix the greater tuberosity fragment. Thereby, the 3-part fracture is converted into a 2-part situation.
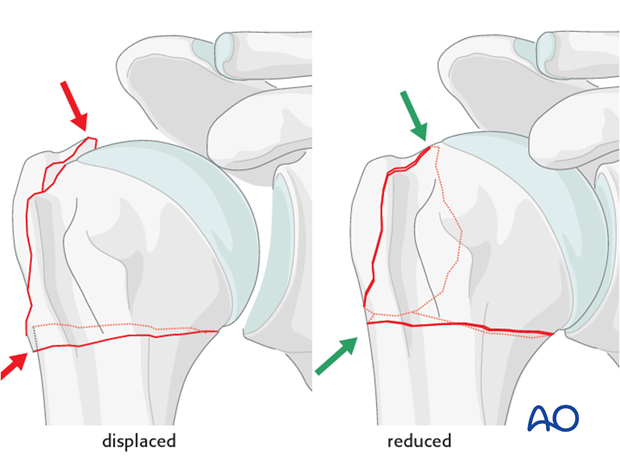
Confirm reduction
After preliminary fixation check the reduction visually and by image intensification.
Visual control
All fracture lines should be closed without any step or gap especially between the greater and lesser tuberosities.
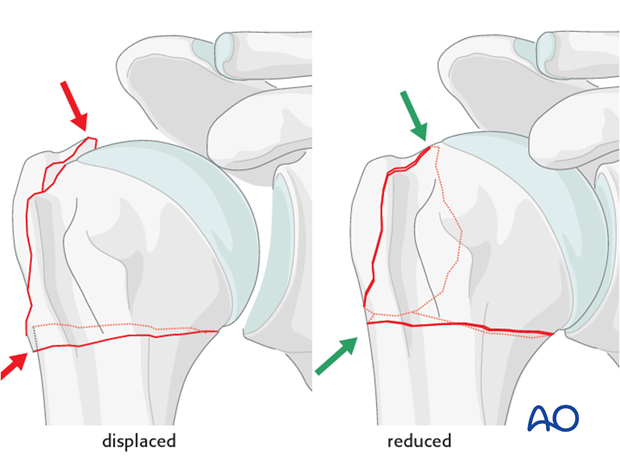
Radiographic confirmation
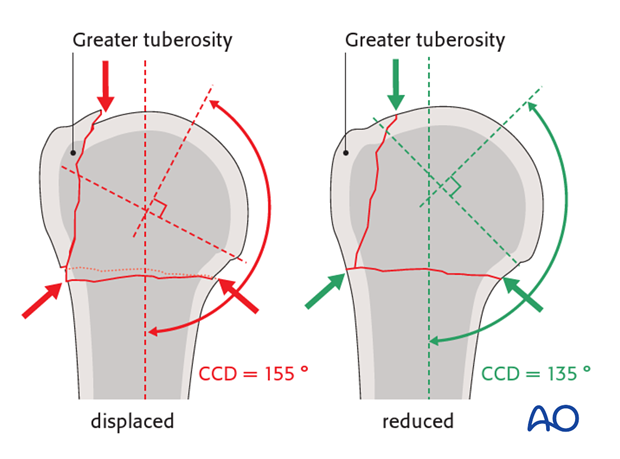
The AP x-ray should show the correct relationship between the humeral head and the tuberosities.
Superolaterally, the humeral head and the greater tuberosity should be flush without a step-off or gap. In particular, make sure that the greater tuberosity is not above the humeral head.
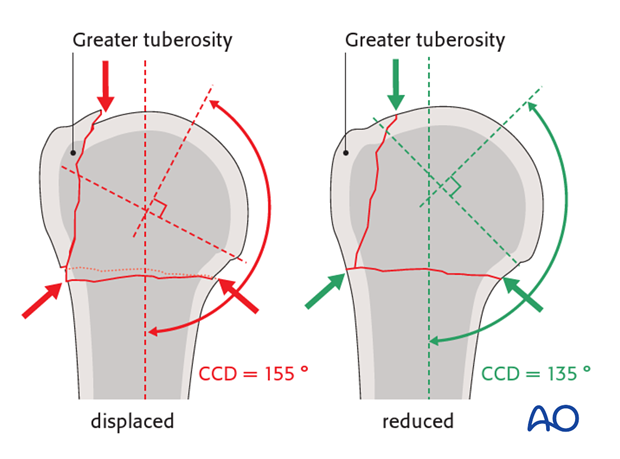
Confirm the inclination of the humeral head. The centrum collum diaphyseal angle (CCD) is illustrated. It is the angle between the axis of the humeral diaphysis, and the axis of the humeral neck, best identified as a perpendicular to the base of the humeral head. The CCD should be approximately 135°.
Valgus displacement of the humeral head must be corrected so there is enough room laterally for the tuberosities to be reduced.
Note: In fractures with apex anterior angular deformity, the axial alignment has to be checked with a lateral image, rather than the AP view.
Confirm proper rotational alignment
Correct rotational alignment must be confirmed. This can be done by matching the fracture configurations on both sides of the fracture. This would be useful in the more transverse fracture configuration as shown in the illustration.
Pearl: check retroversion
The bicipital groove might be a good indicator for correct rotation. In case of correct rotation, no gap/angulation is visible at the level of the fracture.
Remember that the humeral head is normally retroverted, facing approximately 25° posteriorly (mean range: 18°-30°) relative to the distal humeral epicondylar axis. This axis is perpendicular to the forearm with the elbow flexed to 90°.
Preliminary fixation
Quite often, the situation after reduction of the humeral head is stable and does not require additional preliminary fixation with K-wires. Nevertheless, in some cases it might be advantageous to use additional K-wires to secure the position of the humeral head. Therefore, use 2 or 3 K-wires. Make sure to place them from anterior in order to avoid interference with the foreseen plate position.
If the greater tuberosity is multifragmentary it might become necessary to use additional small K-wires in order to fix separate fragments.
Confirmation of reduction
The correct reduction must be confirmed in both AP and lateral views using image intensifier control.
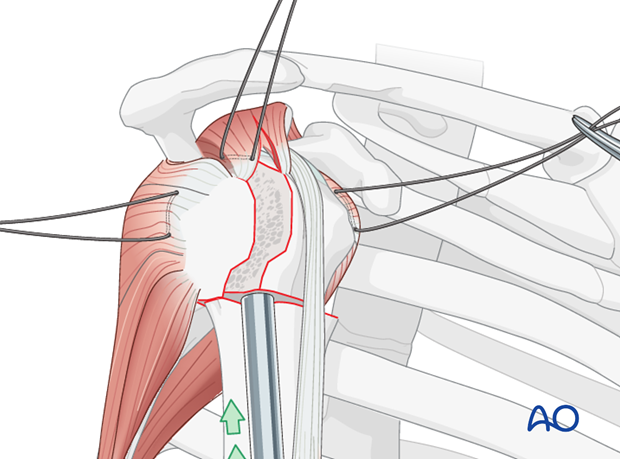
Pearl: reduction of tuberosities under humeral head
Anatomical reduction requires proper approximation of the greater tuberosity underneath the humeral head. Secure this by tightening the horizontal sutures between the subscapularis and infraspinatus tendons (lesser and greater tuberosities).
Pitfall: insufficient reduction of humeral head
A common mistake in reduction of the humeral head is insufficient elevation of the humeral head laterally, in relation to the humeral shaft. This keeps the greater tuberosity from fitting properly under the humeral head. As shown, the humeral head may remain below the top of the tuberosities.
Pearl: osteoporotic bone
In osteoporotic bone, stability may be increased by accepting some medial impaction of the humeral head.
4. Plate position
Correct plate position
The correct plate position is:
- about 5-8 mm distal to the top of the greater tuberosity
- aligned properly along the axis of the humeral shaft
- slightly posterior to the bicipital groove (2-4 mm)
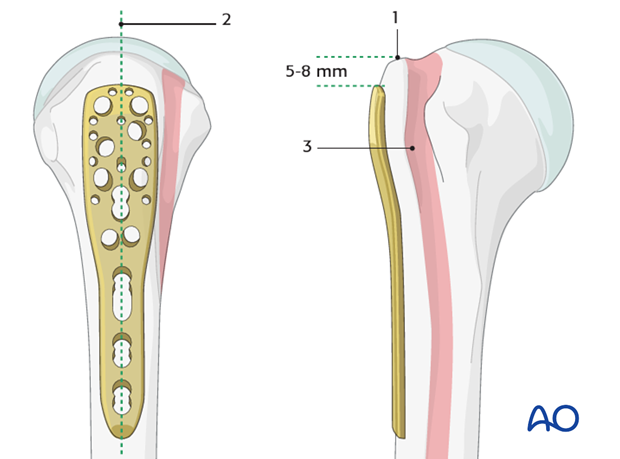
Confirmation of correct plate position
The correct plate position can be checked by palpation of its relationship to the bony structures and also confirmed by image intensification.
To confirm a correct axial plate position insert a K-wire through the proximal hole of the insertion guide. The K-wire should rest on the top of the humeral head.

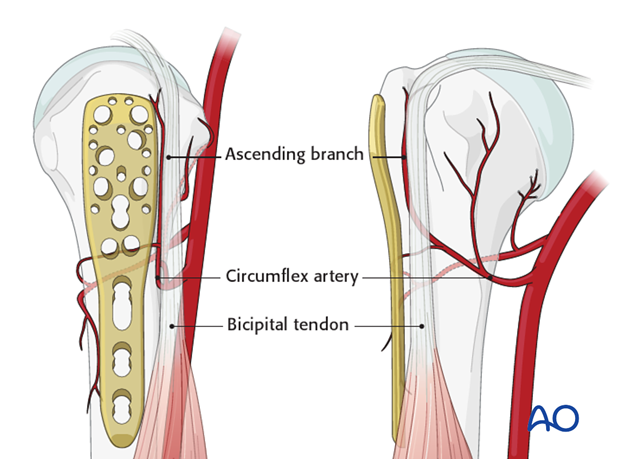
Pitfall 1: plate too close to the bicipital groove
The bicipital tendon and the ascending branch of the anterior humeral circumflex artery are at risk if the plate is positioned too close to the bicipital groove. (The illustration shows the plate in correct position, posterior to the bicipital groove).
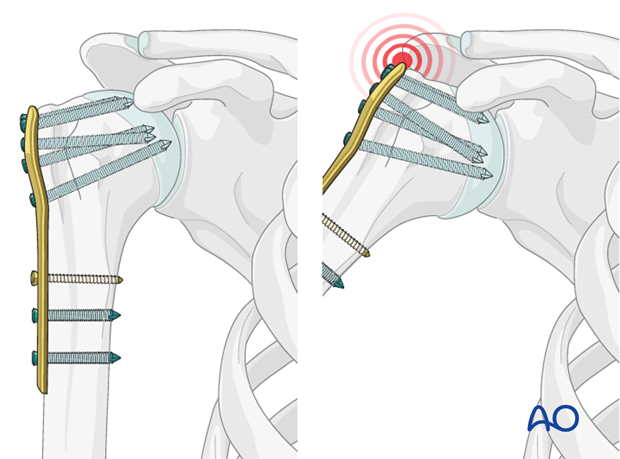
Pitfall 2: plate too proximal
A plate positioned too proximal carries two risks:
- The plate can impinge the acromion
- The most proximal screws might penetrate or fail to securely engage the humeral head
5. Plate fixation
Attach plate to humeral shaft
Attach the plate to the humeral shaft with a bicortical small fragment 3.5 mm screw inserted through the elongated hole.
Pearl 1: fine tuning of plate position
If the first screw is inserted only loosely in the center of the elongated hole, fine-tuning of the plate position is still possible. With the plate in proper position, tighten this screw securely.
Pearl 2: preliminary plate fixation with K-wires
For x-ray confirmation of plate position, one can fix the plate preliminarily to the bone with several 1.4 mm K-wires inserted through the small plate holes, before placing any screws.
Pearl 3: insert K-wires through appropriate guiding sleeves.
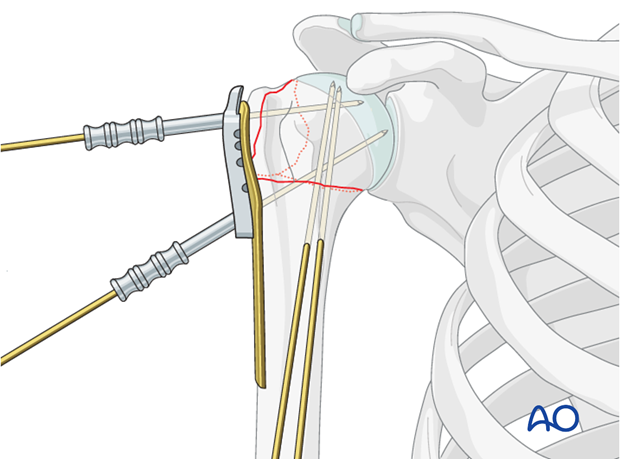
Fix plate to the humeral head
Drill holes
Use an appropriate sleeve to drill holes for the humeral head screws. Do not drill through the subchondral bone and into the shoulder joint.
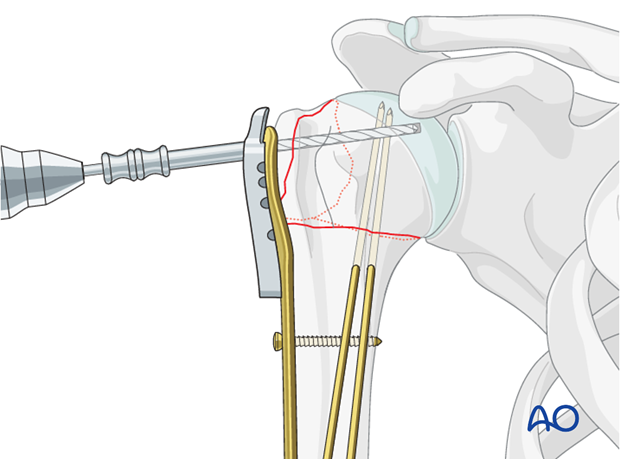
Avoiding intraarticular screw placement
Screws that penetrate the humeral head may significantly damage the glenoid cartilage. Primary penetration occurs when the screws are initially placed. Secondary penetration is the result of subsequent fracture collapse. Drilling into the joint increases the risk of screws becoming intraarticular.
Two drilling techniques help to avoid drilling into the joint.
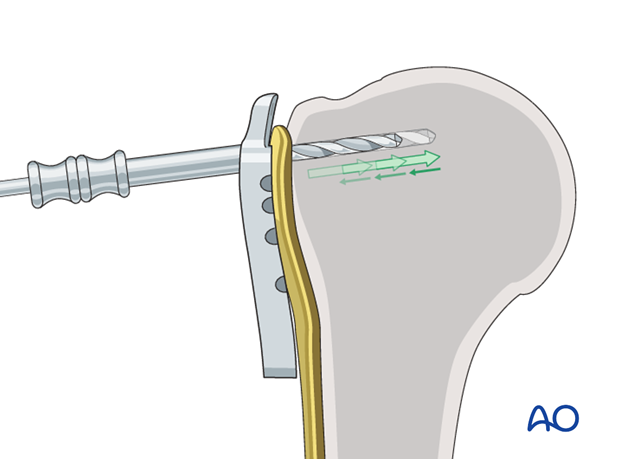
Pearl 1: “Woodpecker”-drilling technique (as illustrated)
In the woodpecker-drilling technique, advance the drill bit only for a short distance, then pull the drill back before advancing again. Keep repeating this procedure until subchondral bone contact can be felt. Take great care to avoid penetration of the humeral head.
Pearl 2: Drilling near cortex only
Particular in osteoporotic bone, one can drill only through the near cortex. Push the depth gauge through the remaining bone until subchondral resistance is felt.
Determine screw length
The intact subchondral bone should be felt with a depth gauge or blunt pin to ensure that the screw stays within the humeral head. The integrity of the subchondral bone can be confirmed by palpation or the sound of the instrument tapping against it. Typically, choose a screw slightly shorter than the measured length.
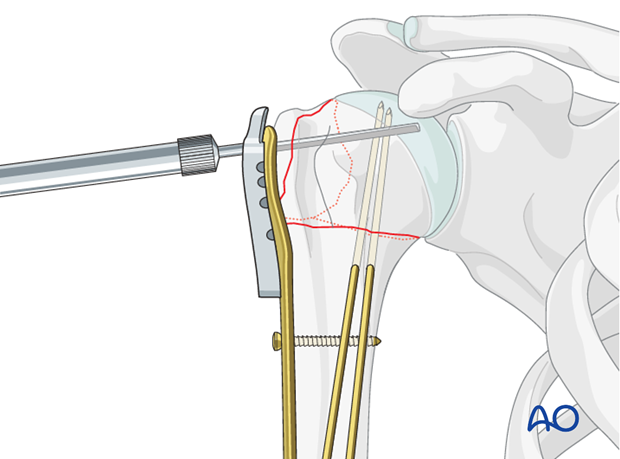
Insert screw
Insert a locking-head screw through the screw sleeve into the humeral head. The sleeve aims the screw correctly. Particularly in osteoporotic bone, a screw may not follow the hole that has been drilled.
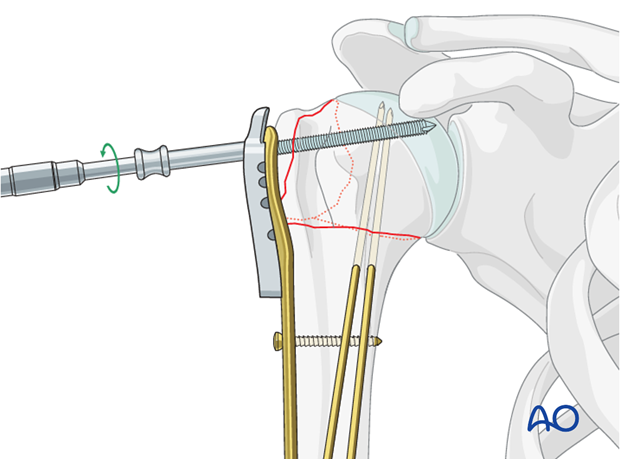
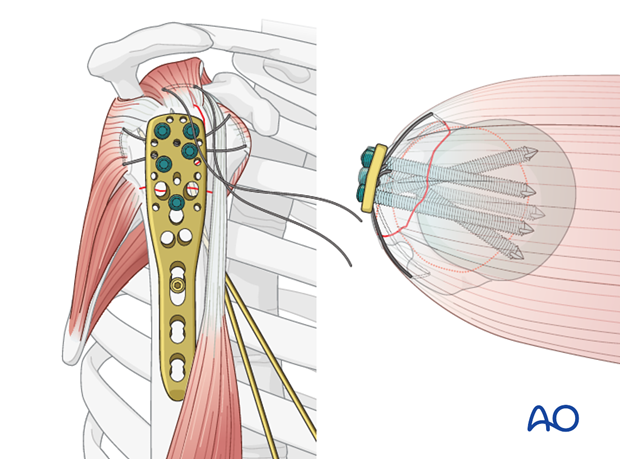
Number of screws and location
Place a sufficient number of screws (often 5) into the humeral head. The optimal number and location of screws has not been determined. Bone quality and fracture morphology should be considered. In osteoporotic bone a higher number of screws may be required.
Insert additional screws into the humeral shaft
Insert one or two additional bicortical screws into the humeral shaft.
Any K-wires placed during the procedure may now be removed.
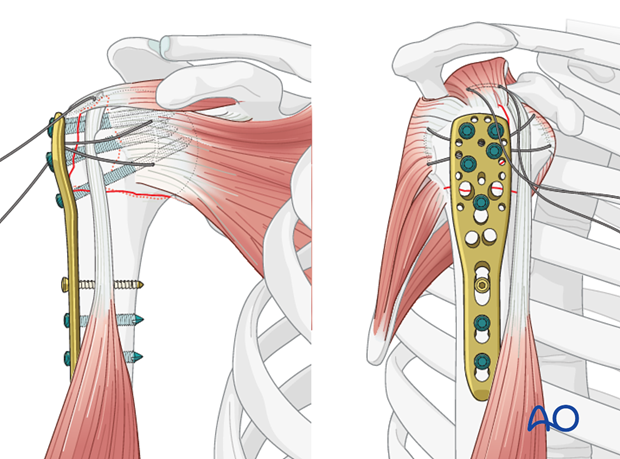
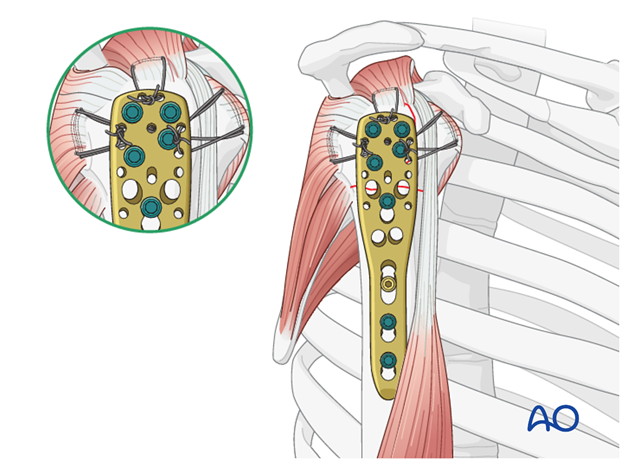
6. Supplementary rotator cuff tendon sutures
Secure the tendons of the rotator cuff (subscapularis, supraspinatus, infraspinatus) with additional neutralization sutures through the small holes in the plate.
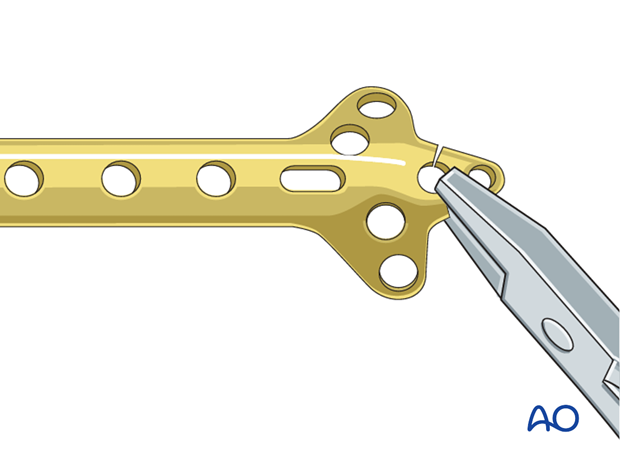
7. Use of standard plates
If no angular stable plate is available, a standard plate provides an alternative. The described procedure (reduction, preliminary fixation, and rotator cuff sutures) is essentially the same for standard plates, except for the screws. A good choice from the standard plates is the small fragment cloverleaf plate, with its tip cut off, and contoured as necessary. This plate allows multiple small fragment screws for the humeral head.
Be aware that angular stable implants provide better fixation, especially in osteoporotic bone. On the other hand, even angular stable plates are not a substitute for good surgical technique and judgment. Advances in fracture classification, understanding of the blood supply, use of rotator cuff tendon sutures, anatomical fracture reduction, and provisional fixation, represent improvements in care. When combined with optimal implants, these contributions offer the best chance of a good outcome.
8. Final check of osteosynthesis
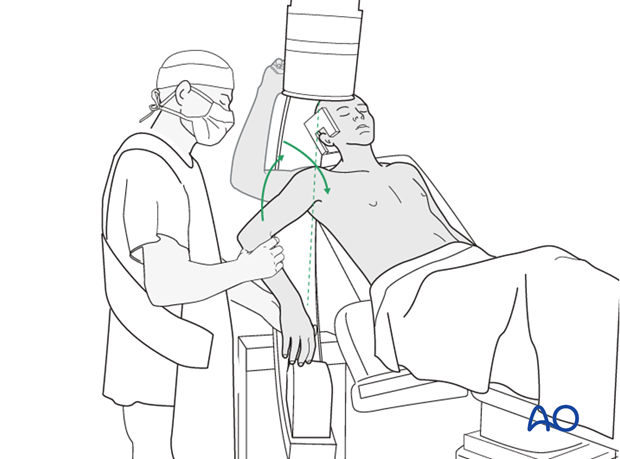
Using image intensification, carefully check for correct reduction and fixation (including proper implant position and length) at various arm positions. Ensure that screw tips are not intraarticular.
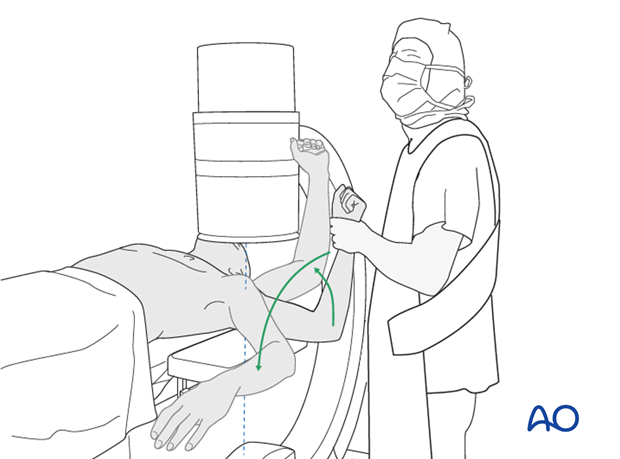
Also obtain an axial view.
In the beach chair position, the C-arm must be directed appropriately for orthogonal views. Position arm as necessary to confirm that reduction is satisfactory, fixation is stable, and no screw is in the joint.
9. Overview of rehabilitation
The shoulder is perhaps the most challenging joint to rehabilitate both postoperatively and after conservative treatment. Early passive motion according to pain tolerance can usually be started after the first postoperative day - even following major reconstruction or prosthetic replacement. The program of rehabilitation has to be adjusted to the ability and expectations of the patient and the quality and stability of the repair. Poor purchase of screws in osteoporotic bone, concern about soft-tissue healing (eg tendons or ligaments) or other special conditions (eg percutaneous cannulated screw fixation without tension-absorbing sutures) may enforce delay in beginning passive motion, often performed by a physiotherapist.
The full exercise program progresses to protected active and then self-assisted exercises. The stretching and strengthening phases follow. The ultimate goal is to regain strength and full function.
Postoperative physiotherapy must be carefully supervised. Some surgeons choose to manage their patient’s rehabilitation without a separate therapist, but still recognize the importance of carefully instructing and monitoring their patient’s recovery.
Activities of daily living can generally be resumed while avoiding certain stresses on the shoulder. Mild pain and some restriction of movement should not interfere with this. The more severe the initial displacement of a fracture, and the older the patient, the greater will be the likelihood of some residual loss of motion.
Progress of physiotherapy and callus formation should be monitored regularly. If weakness is greater than expected or fails to improve, the possibility of a nerve injury or a rotator cuff tear must be considered.
With regard to loss of motion, closed manipulation of the joint under anesthesia, may be indicated, once healing is sufficiently advanced. However, the danger of fixation loosening, or of a new fracture, especially in elderly patients, should be kept in mind. Arthroscopic lysis of adhesions or even open release and manipulation may be considered under certain circumstances, especially in younger individuals.
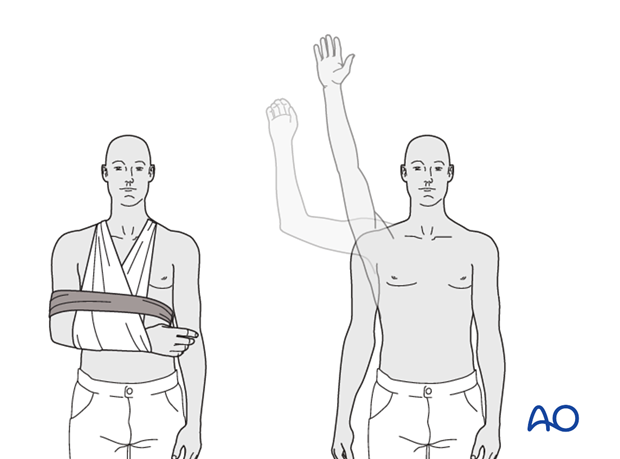
Progressive exercises
Mechanical support should be provided until the patient is sufficiently comfortable to begin shoulder use, and/or the fracture is sufficiently consolidated that displacement is unlikely.
Once these goals have been achieved, rehabilitative exercises can begin to restore range of motion, strength, and function.
The three phases of nonoperative treatment are thus:
- Immobilization
- Passive/assisted range of motion
- Progressive resistance exercises
Immobilization should be maintained as short as possible and as long as necessary. Usually, immobilization is recommended for 2-3 weeks, followed by gentle range of motion exercises. Resistance exercises can generally be started at 6 weeks. Isometric exercises may begin earlier, depending upon the injury and its repair. If greater or lesser tuberosity fractures have been repaired, it is important not to stress the rotator cuff muscles until the tendon insertions are securely healed.
Special considerations
Glenohumeral dislocation: Use of a sling or sling-and-swath device, at least intermittently, is more comfortable for patients who have had an associated glenohumeral dislocation. Particularly during sleep, this may help avoid a redislocation.
Weight bearing: Neither weight bearing nor heavy lifting are recommended for the injured limb until healing is secure.
Implant removal: Implant removal is generally not necessary unless loosening or impingement occurs. Implant removal can be combined with a shoulder arthrolysis, if necessary.
Shoulder rehabilitation protocol
Generally, shoulder rehabilitation protocols can be divided into three phases. Gentle range of motion can often begin early without stressing fixation or soft-tissue repair. Gentle assisted motion can frequently begin within a few weeks, the exact time and restriction depends on the injury and the patient. Resistance exercises to build strength and endurance should be delayed until bone and soft-tissue healing is secure. The schedule may need to be adjusted for each patient.
Phase 1 (approximately first 3 weeks)
- Immobilization and/or support for 2-3 weeks
- Pendulum exercises
- Gently assisted motion
- Avoid external rotation for first 6 weeks
Phase 2 (approximately weeks 3-9)
If there is clinical evidence of healing and fragments move as a unit, and no displacement is visible on the x-ray, then:
- Active-assisted forward flexion and abduction
- Gentle functional use week 3-6 (no abduction against resistance)
- Gradually reduce assistance during motion from week 6 on
Phase 3 (approximately after week 9)
- Add isotonic, concentric, and eccentric strengthening exercises
- If there is bone healing but joint stiffness, then add passive stretching by physiotherapist













