Compression plate
1. Principles
In the setting of a two-part metaphyseal or diaphyseal fracture that occurs in a non-osteoporotic patient, take care to achieve anatomical reduction of the single plane fracture and achieve interfragmentary compression, giving absolute stability.
2. Implant selection
Plate selection
Compression of simple metaphyseal fractures can be achieved with compression plate technique, interfragmentary screw fixation with neutralization plate.
Depending on which technique is employed, a plate can be selected from the following options:
- Standard locking compression plate
- Precontoured locking compression plate, including variable angle systems
Options for additional stability
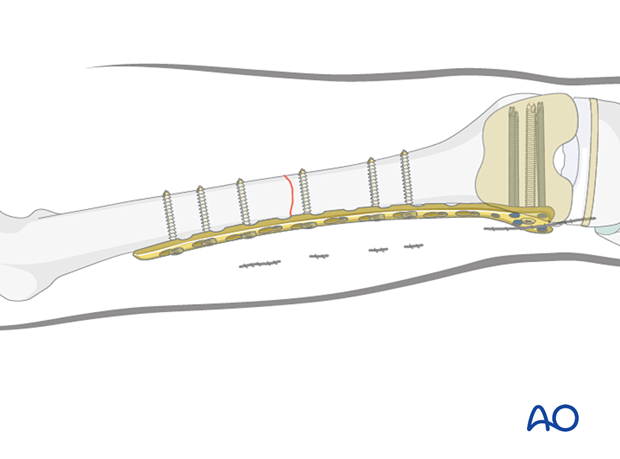
Additional stabilization can be achieved with locking and nonlocking screw fixation above and below the fracture site.
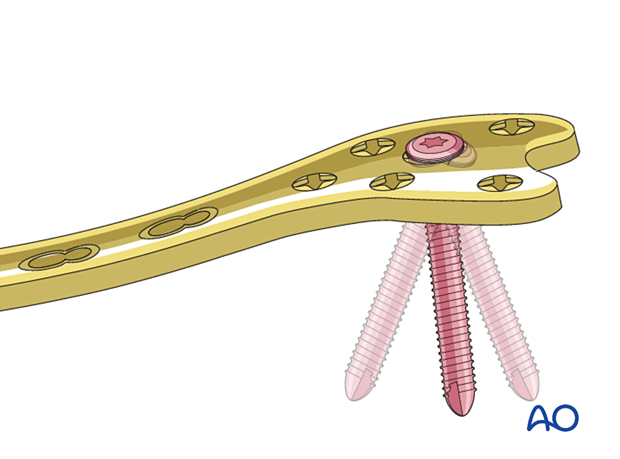
If there is no room for bicortical screw fixation, different options may be used around the component stem to secure the plate:
- Unicortical locking screw fixation
- Cerclage cables integrated into the plate
- Locking attachment plate
For additional details on these implants please refer to adjunct plate options.
3. Preparation and approach
This procedure is usually performed through an anterolateral or lateral approach.
4. Reduction
Direct reduction techniques are used to achieve anatomical reduction under direct vision. Indirect maneuvers may be required to overcome commonly encountered deforming forces.
Main deformities
Three major deformities are managed:
- Varus/valgus: frontal plane alignment is checked by assessing the quality of direct reduction and evaluating limb alignment in comparison with the uninjured site. This is facilitated by prepping and draping both legs.
- Rotation: rotational alignment is checked by assessing the quality of direct reduction and evaluating torsional profile in comparison with the uninjured site. This is facilitated by prepping and draping both legs.
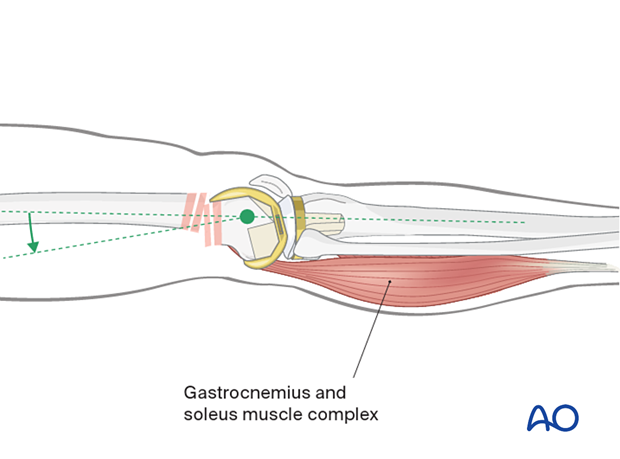
- Flexion/extension (sagittal plane alignment): take care to overcome the deforming force from the pull of the gastrocnemius insertion of the muscle in the distal fragment.
Flexion of the knee over a padded bump is of assistance.
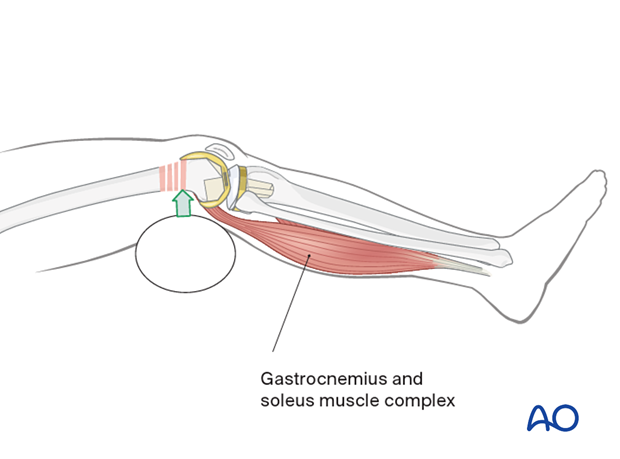
If the fracture pattern allows, a sagittal pin can be used as a joystick in the condylar block to correct flexion/extension before interfragmentary compression is achieved.
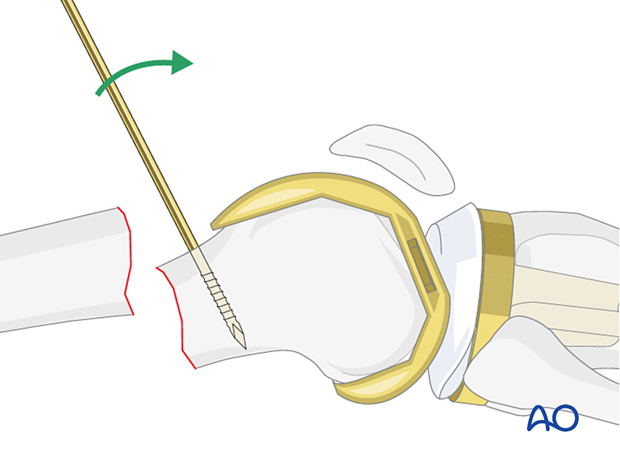
5. Plate fixation
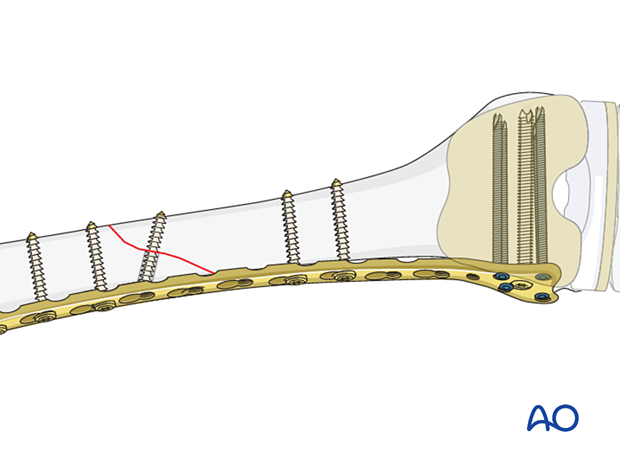
Compression plate
It is recommended to apply controlled compression to the metaphyseal fracture component using the articulated tension device when there is direct contact between the proximal and distal main fragments in simple transverse fractures.
Severely comminuted or osteoporotic metaphyseal fractures should not be compressed.
Distal fixation is achieved with screws into the metaphysis and then a Verbrugge clamp is loosely applied to the proximal segment. The articulated tension device is engaged in the proximal hole of the plate and fixed to the bone with a bicortical screw. An articulating wrench is then used to compress the fracture zone. When this occurs the strain gauge on the device goes from the green zone to the yellow zone and finally to the red zone. During the use of this wrench, the fracture complex must be monitored to ensure that no undesirable displacement occurs.
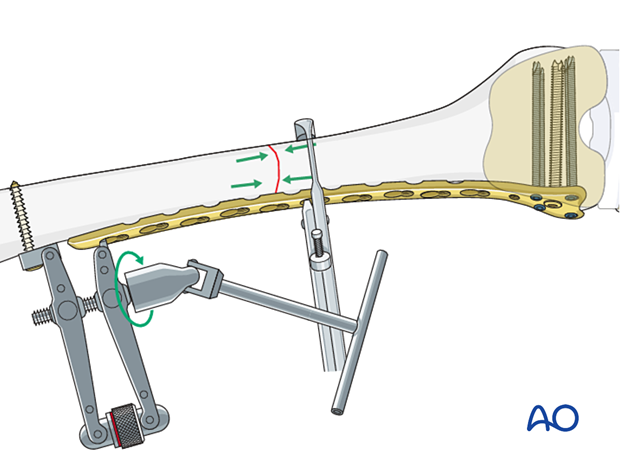
After the appropriate tension is applied, a screw is inserted into the proximal segment in the eccentric position for additional compression of the fracture site.
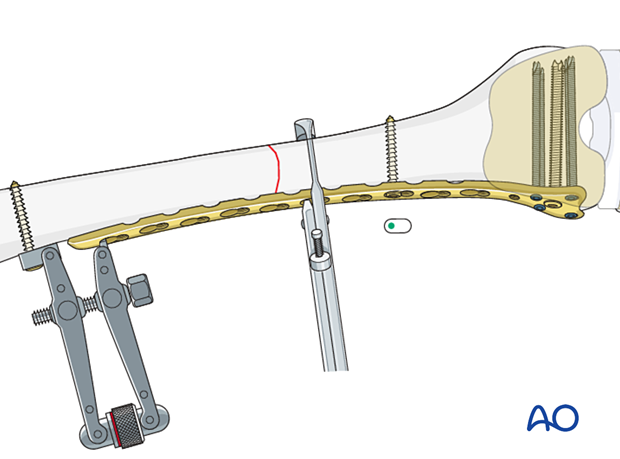
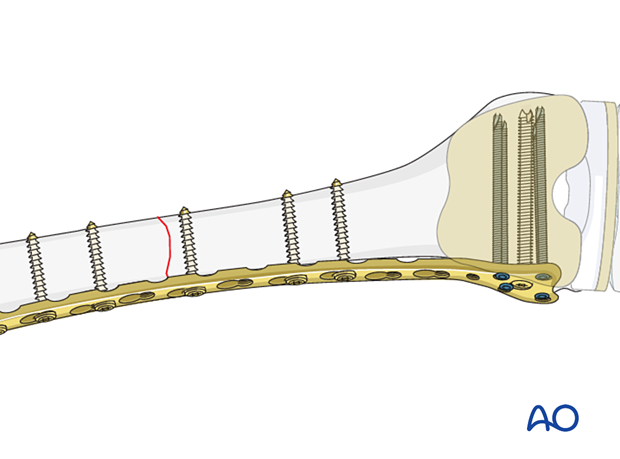
2 to 3 additional cortical screws should be inserted to the proximal fragment.
Oblique single-plane fractures
In oblique, single-plane fractures, an interfragmentary lag screw should be inserted through the plate. Alternatively, the lag screw may be inserted outside the plate prior to plate application.
Final check of fracture reduction and fixation
Gently move the knee through a full range of motion. Carry out a clinical assessment of the rotational profile. Finally, perform a radiographic assessment of the frontal-plane alignment (varus/valgus) and sagittal-plane alignment (extension/flexion).
Examine the knee for any ligamentous instability.
6. Aftercare
These fixation techniques will allow early full weight bearing immediately postoperatively.
Knee bracing is not essential and should be considered optional for patient comfort.













