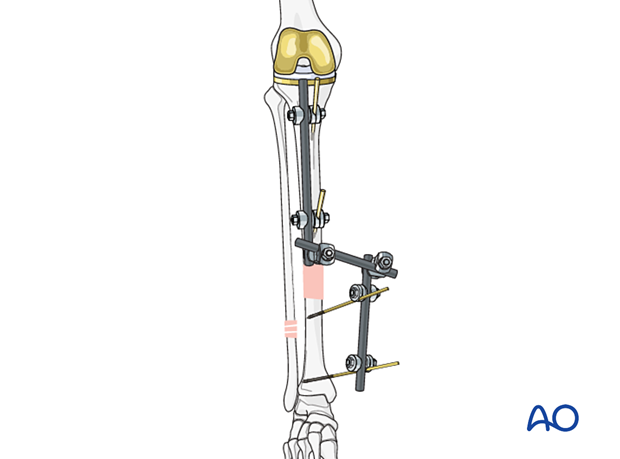
Temporary external fixator
1. Introduction
An external fixator can be considered for periprosthetic fractures. However, there is an increased risk of introducing an infection to knee arthroplasty. Keeping pins as far away from the arthroplasty as possible will decrease this risk. Consideration of spanning knee external fixation instead of isolated tibial external fixation may also enable the surgeon to protect the knee arthroplasty more effectively.
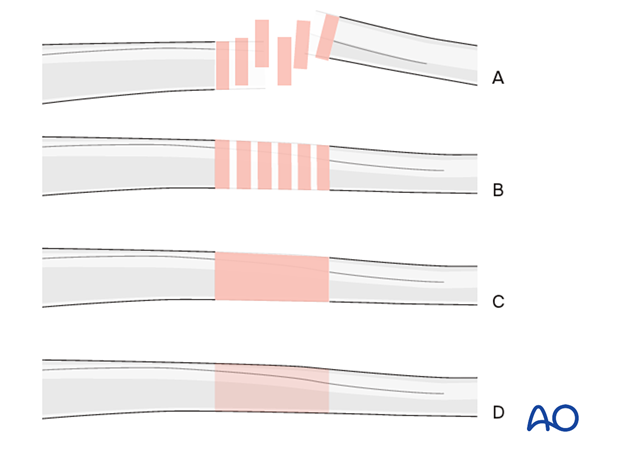
2. Note on illustrations
Throughout this treatment option, illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fracture
B) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
3. Principles of modular external fixation
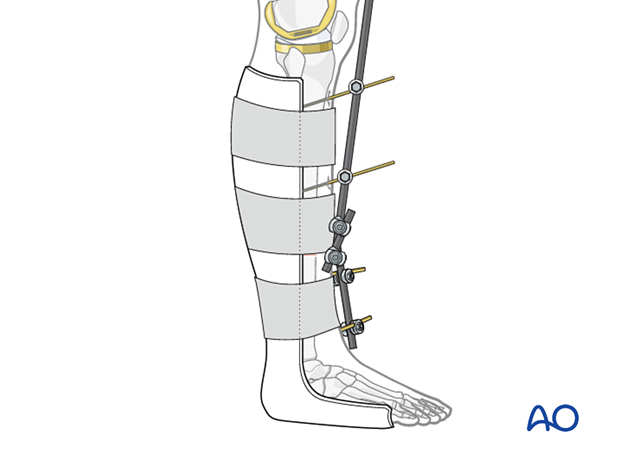
The modular external fixator is optimal for temporary use. It is rapidly applied without the need for intraoperative x-rays and can be adjusted later.
Details of external fixation are described in the basic technique for the application of a modular external fixator.
Specific considerations for the tibial shaft are given below.
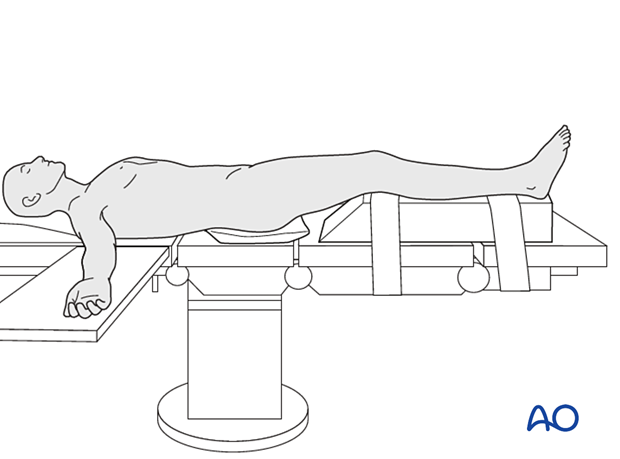
4. Patient preparation
This procedure is typically performed with the patient in a supine position.
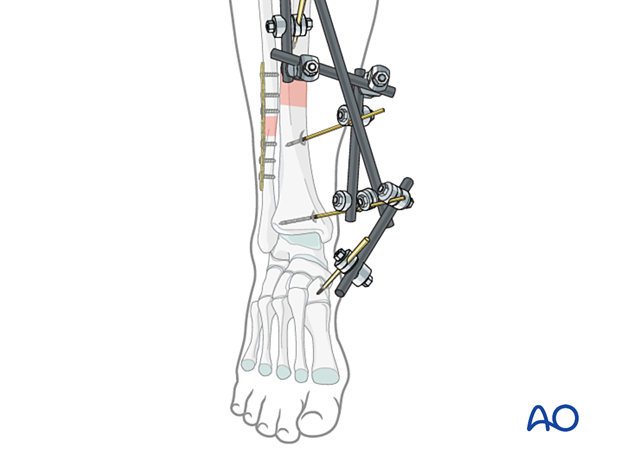
5. Safe zones for pin placement
For safe pin placement, make use of the safe zones and be familiar with the lower leg's anatomy.
Care should be taken to avoid contact with the cement mantle surrounding the tibial component, as a Schanz pin would be likely to disrupt the integrity of that cement.
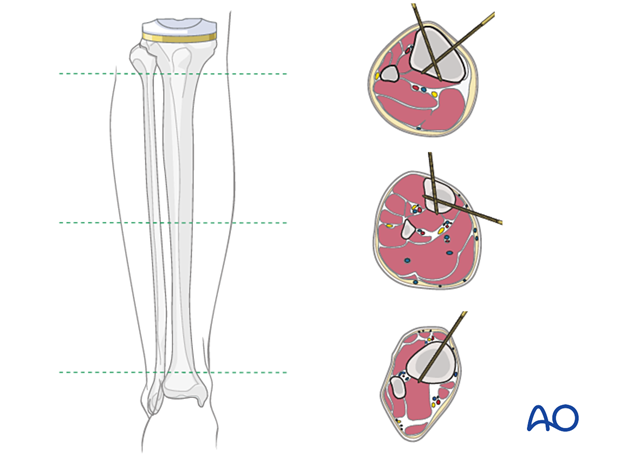
6. Pin insertion (tibial shaft)
In definitive external fixation, self-drilling pins should be avoided due to excessive heat generation leading to infection and pin loosening. Similarly, drilling a hole in the thick tibial crest is also associated with excessive heat generation. As the anteromedial tibial wall provides adequate thickness for the placement of pins, this trajectory is preferable. A trajectory angle (relative to the sagittal plane) of 20-60° for the proximal fragment and 30-90° for the distal fragment is recommended.
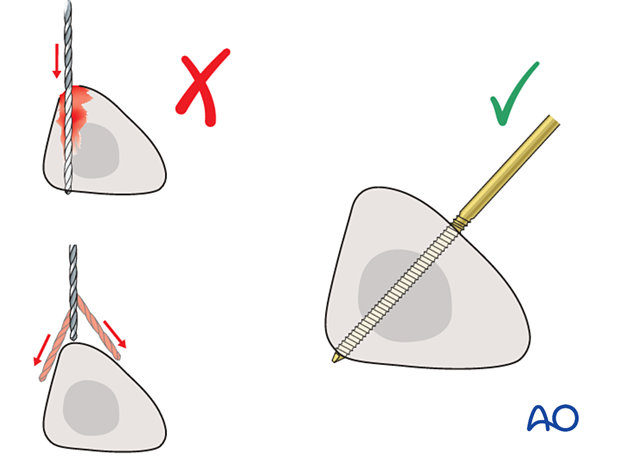
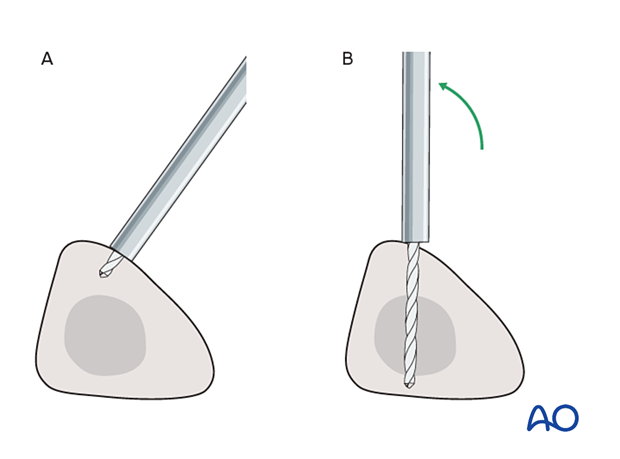
The pins may be placed more anteriorly to avoid the frame catching on the opposite leg. The drill bit is started with the tip just medial to the anterior crest and with the drill bit perpendicular to the anteromedial surface (A). As the drill bit starts to penetrate the surface, the drill is gradually moved more anteriorly until the drill bit is in the desired plane (B). This should prevent the tip from sliding down the medial or lateral surface.
7. Frame construction / reduction and fixation (tibial shaft)
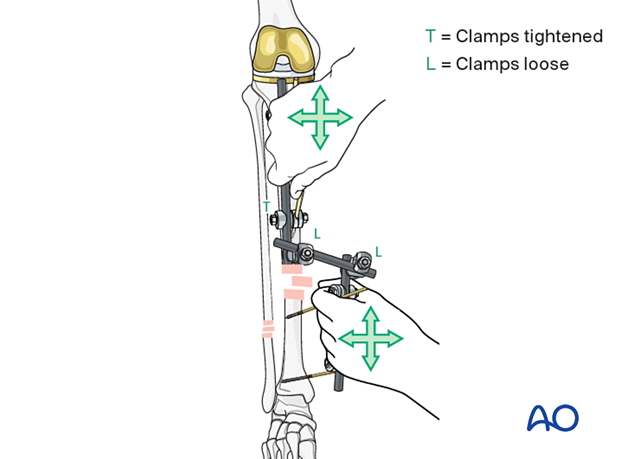
Reduction and fixation
Restore length with a bolster behind the knee to give slight flexion.
Plating of the fibula
A fractured fibula may be plated to add further stability to the reduction.
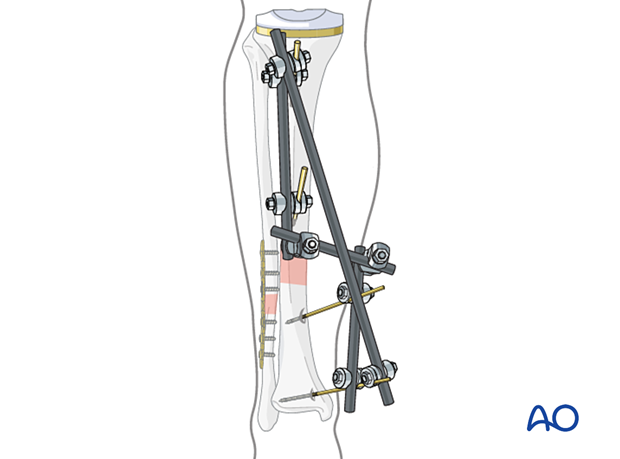
Pearl: Prevent plantar flexion contracture
In patients with severe soft-tissue involvement, it may be helpful to add a pin in the foot (one of the tarsal or metatarsal bones) to maintain the ankle at a 90° angle and prevent a plantar flexion contracture.
The pin may be inserted in either the navicular bone, in one of the cuneiforms, in the first metatarsal base, or in the first and fifth metatarsal base, and connected with a rod to the tibial external fixator. The medial cuneiform and the first metatarsal are large enough to accommodate a more stable 5 mm pin. Care should be taken to insert the pin bicortically and to avoid the intra-articular spaces.
Alternatively, a splint may be fashioned to prevent equinus position of the foot.
8. Aftercare following external fixation
Thromboembolic prophylaxis
Thrombo-prophylaxis should be given according to local treatment guidelines.
Pin-site care
Proper pin insertionThe pin-insertion technique is important to prevent postoperative complications. Pin care protocol includes:
- Correct placement of pins (see safe zones) avoiding ligaments and tendons, e.g., tibia anterior
- Correct insertion of pins (e.g., trajectory, depth) avoiding heat necrosis
- Extending skin incisions to release soft-tissue tension around the pin insertion (see inspection and treatment of skin incisions)
Local aftercare protocols to prevent pin tract infection are generally in place. The following points are recommended:
- The pin-insertion sites should be kept clean. Any crusts or exudates should be removed. The pins should be cleaned using regular water and soap (by taking a normal shower). The cleaning frequency depends on the circumstances and varies from daily to weekly but should be done in moderation.
- No ointments or antibiotic solutions are recommended for routine pin-site care.
- Dressings are not usually necessary once wound drainage has ceased.
In the case of pin loosening or pin tract infection, the following steps need to be taken:
- Remove all involved pins and place new pins in a healthy location.
- Debride the pin sites in the operating theater, using curettage and irrigation.
- Take specimens for a microbiological study to guide appropriate antibiotic treatment if necessary.
Before changing to a definitive internal fixation, an infected pin tract needs to heal. Otherwise, infection will result.
Follow up
See patient 7-10 days after surgery for a wound check. X-rays are taken to check the reduction.
Implant removal
The external fixator is usually removed before the definitive internal fixation. Occasionally, it may be maintained to aid in reducing the fracture during plate fixation, but in these cases, there must be no sign of any infection before going to the operating room.













