Safe zones for pin placement
1. General considerations
For pin insertion, the condition of the soft-tissue envelope has to be considered. Areas of crush injuries or areas of extensive soft-tissue damage should be avoided, in order to minimize the risk of subsequent pin-track infection.
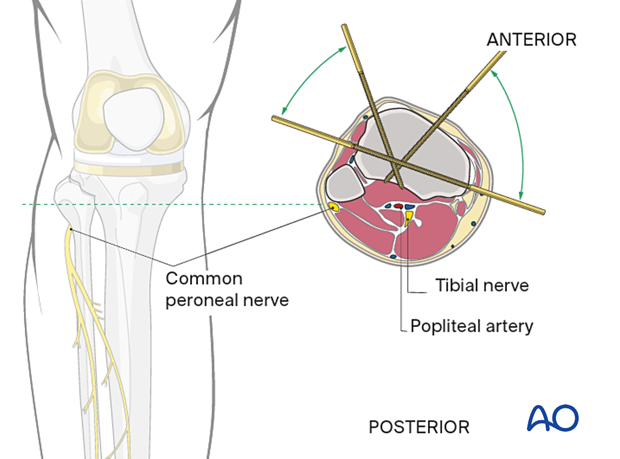
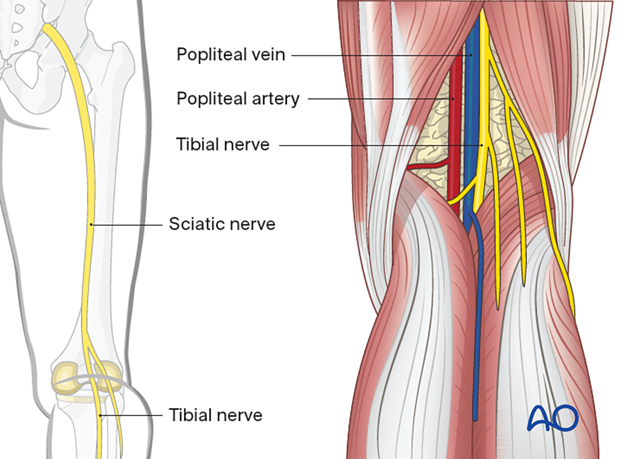
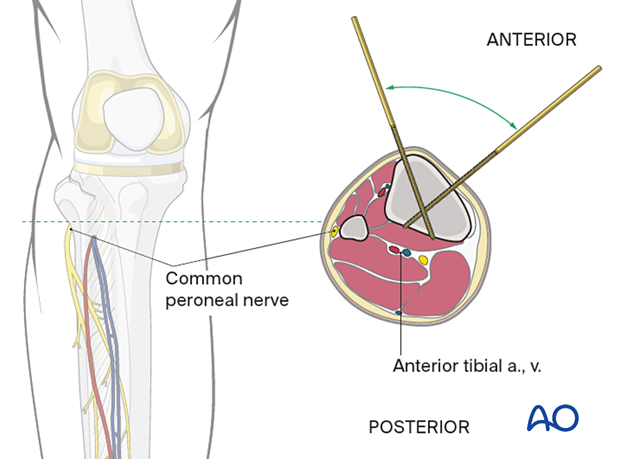
Make sure to avoid the neurovascular structures around the knee (common peroneal nerve, deep peroneal nerve, and popliteal artery).
The safest anatomical zones for pin insertion are from the anterolateral to direct medial regions of the tibia. See the anatomical location of muscle groups and neurovascular bundles in each respective region.
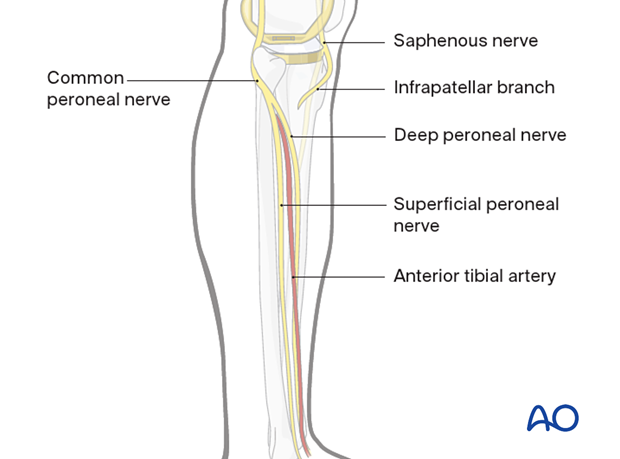
2. Lower leg
Common peroneal nerve
The common peroneal nerve begins posteriorly in the thigh and runs from the center of the popliteal fossa laterally and anteriorly together and below the tendon of the biceps femoris. It winds anteriorly around the neck of the fibula and then ramifies in the anterior compartment into superficial sensory and deep motor and sensory branches. Damage to this nerve results in a severe functional deficit.
Saphenous nerve
The saphenous nerve is purely sensory. It runs distally on the anteromedial side of the thigh and passes the knee joint on the medial side of the patella where it gives off the infrapatellar branch. At the ankle, it is anterior to the medial malleolus where it runs together with the long saphenous vein. Injury to this nerve will not result in functional deficit but results in a sensory loss and problems with neuroma formation.
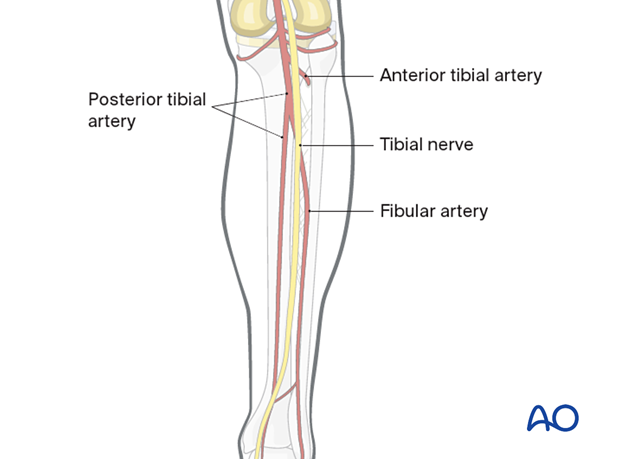
Popliteal artery
The popliteal artery traverses the center of the popliteal fossa. It trifurcates at the level of the proximal tibial shaft into the anterior tibial artery which enters the anterior compartment just above the interosseous membrane, the fibular or peroneal artery, and into the posterior tibial artery.
Tibial nerve
The tibial nerve passes through the popliteal fossa and courses deep to the arterial supply throughout the remainder of the leg.
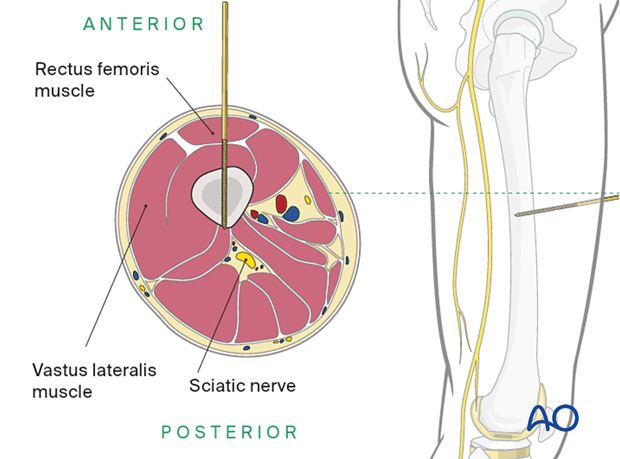
3. Upper leg
Safe zones
The safest anatomical zones for pin insertion are the anterolateral and direct lateral regions of the femur. See the anatomical location of muscle groups and neurovascular bundles in each respective region.
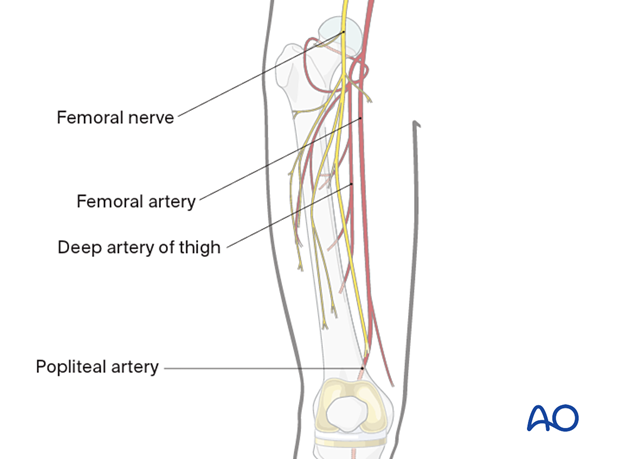
Anatomy
The diaphysis of the femur is surrounded by a thick muscular envelope. The major neurovascular structures are located medially and posteriorly and, therefore, the femur can safely be approached over the anterolateral region.
The femoral nerve passes out of the pelvis and courses down the medial aspect of the leg. The femoral nerve provides innervation to the vastus musculature with branches that typically course across the femur just distal to the lesser trochanter.
Vascular anatomy
The external iliac becomes the femoral artery when it leaves the pelvis and gives rise to the profunda in the proximal one-third of the femur. The arterial branches remain posteromedial to the femur for the large majority of the upper leg, allowing for safe exposure of the femur or up to 60% of the femoral diaphysis.
Sciatic nerve
The sciatic nerve passes out of the greater sciatic notch and courses down the femur posterolaterally within the posterior compartment through the popliteal fossa. The division of the sciatic nerve in the peroneal and tibial branches is variable, it can occur even as the nerve exits the pelvis. However, the divisions course through the upper leg together until they pass the popliteal fossa.
4. Pin insertion (external fixator)
Locations for pin insertion
The proper locations for pin insertion for external fixators have to be chosen according to the type of external fixator indicated. Total knee arthroplasty can significantly limit the safe zone for pin insertion. In general, the pin should be kept outside of the fracture hematoma and should be as far distant to the prosthesis as possible. Any possible introduction of bacteria into the intramedullary canal can lead to prosthetic infection.
Bridging external fixator
For bridging external fixators, the pins are placed anteriorly in the femoral and tibial shafts.
Nonbridging external fixator
For nonbridging external fixators, the pins are placed only in the tibia.
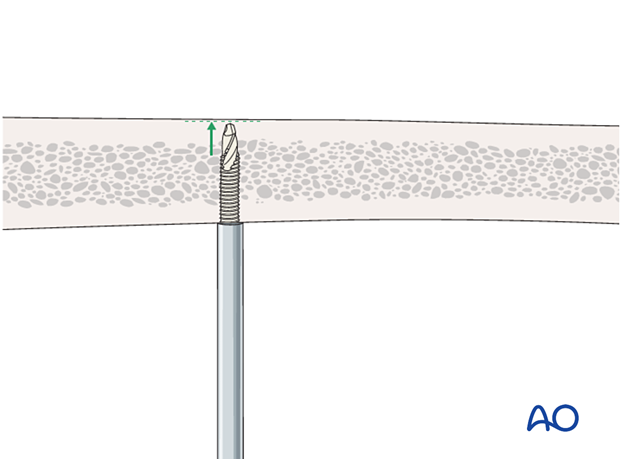
Depth of pin insertion
Pins must be inserted sufficiently deep to engage in the far cortex. In the far cortex, the pins must not protrude so as not to injure the neurovascular bundle or the soft tissues.
Self-drilling, self-tapping Schanz pins should not be inserted beyond the second cortex.
Threads in the far cortex can create thermal necrosis of the proximal cortex leading to pin loosening and the self-drilling tip can threaten neurovascular structures beyond the far cortex. Thus, self-drilling, self-tapping Schanz pins should not be inserted beyond the second cortex.
Predrilling should be considered in patients with dense bone.
5. Proximal tibia
Proximal tibial head
Neurovascular structures (NVS)In the depth of the popliteal fossa, we find the neurovascular structures in close proximity to the bone. The exact distance of the neurovascular structures to the bone and to the middle of the tibia is variable.
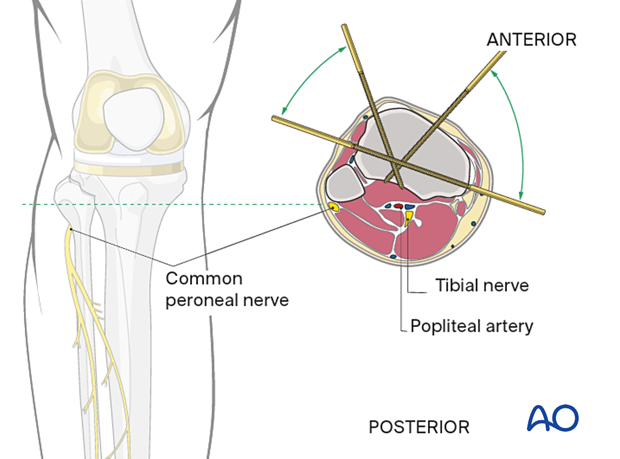
Pin placement should respect the knee joint capsule and therefore be below 2 cm of the tibial plateau. If a more proximal pin fixation is necessary for very high fractures pin placement should be as anterior as possible due to the shorter extension of the knee joint capsule in this area.
The utilization of fine wires is recommended as fixation closer to the joint becomes necessary.
Distal of the tibial tuberosity
To minimize the risk of infection it is best to insert the pins where soft-tissue coverage is minimal.
Therefore distal to the tibial tubercle the safe zones for pin insertion are the tibial crest and the medial face of the tibia.
One must be careful and avoid deep penetration beyond the far cortex.
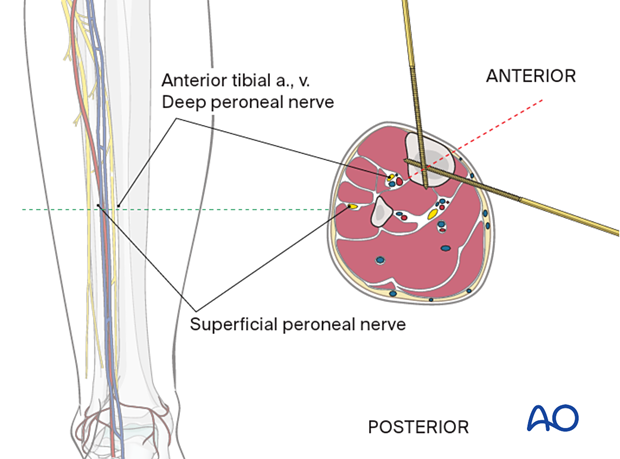
6. Tibial shaft
The neurovascular bundle (the anterior tibial artery and vein together with the deep peroneal nerve) runs anterior to the interosseous membrane close to the posterolateral border of the tibia.
They are at risk if the pin is inserted in the direction as indicated by the red dotted line approximately halfway between the anterior crest and the medial edge of the tibia.
7. Midshaft of the femur
The neurovascular structures in the midshaft of the femur are medial, and anterior placement of the pins will avoid them. The distal pin should avoid the suprapatellar pouch in order to be extraarticular. A general rule is to insert pins more than 8-10 cm from the superior pole of the patella.