Compression plate
1. Introduction
Nonoperative treatment of periprosthetic fractures of the proximal tibia often leads to nonunion or malunion. However, operative stabilization can be challenging because of the limited available bone stock for fixation.
2. Implant selection
Fracture fixation is largely dependent on the anatomy of the fracture and the selected approach. The proximal tibia requires the use of low-profile plating constructs due to poor soft tissue coverage. Medial, lateral, and posteromedial options are possible.
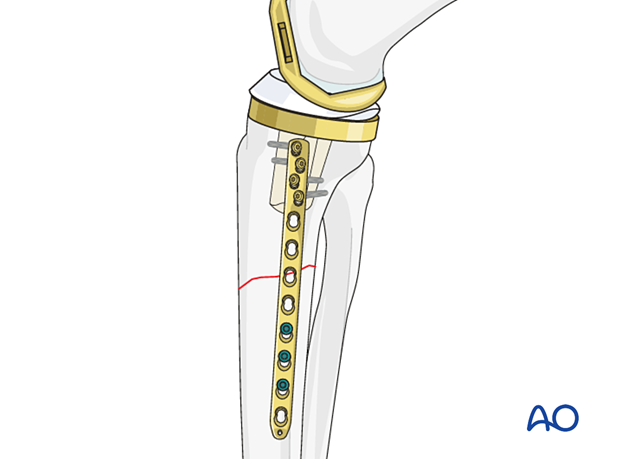
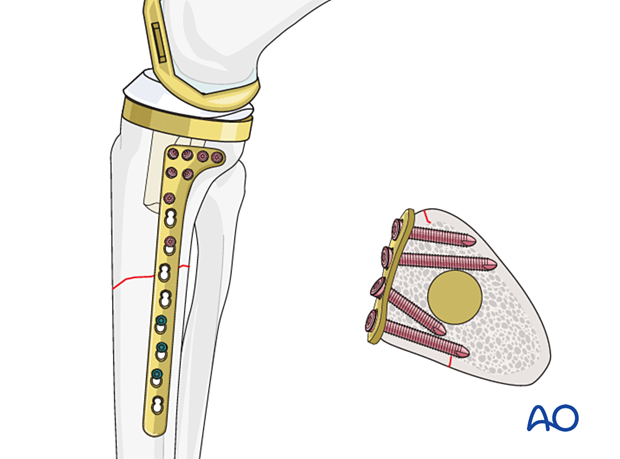
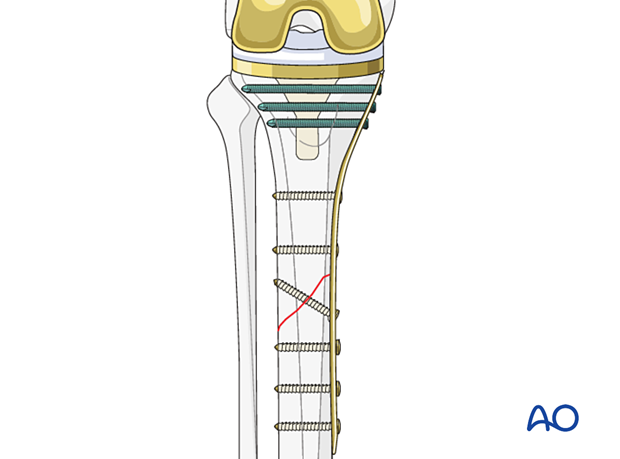
Variable angle locking options are advantageous in the proximal tibia when screw placement is limited by the prosthesis and the cement mantle.
Some plates offer small fragment and large fragment options at opposite ends of the plate, which allows for a low-profile option on the proximal tibia (metaphyseal plate).

Options for additional stability
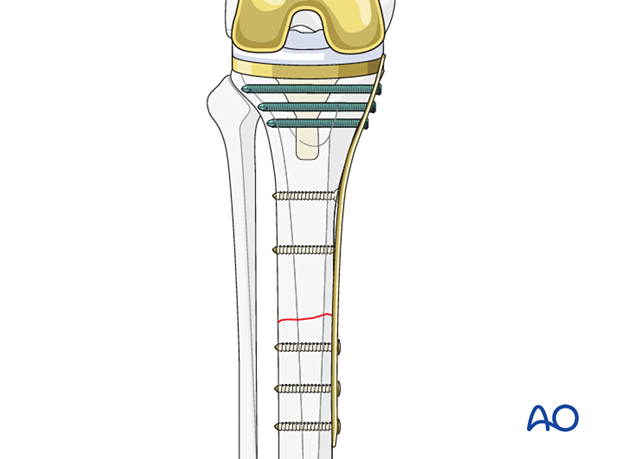
Additional stabilization can be achieved with locking and nonlocking screw fixation above and below the fracture site.
If there is no room for bicortical screw fixation, different options may be used around the component stem to secure the plate:
- Unicortical locking screw fixation
- Cerclage cables integrated into the plate
- Locking attachment plate
For additional details on these implants please refer to adjunct plate options.
3. Patient preparation and approach
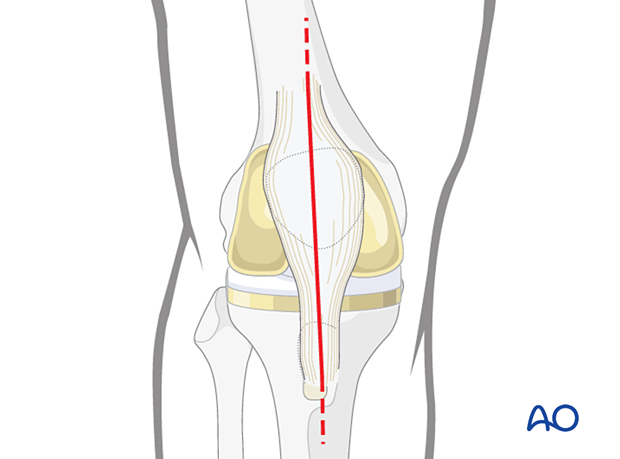
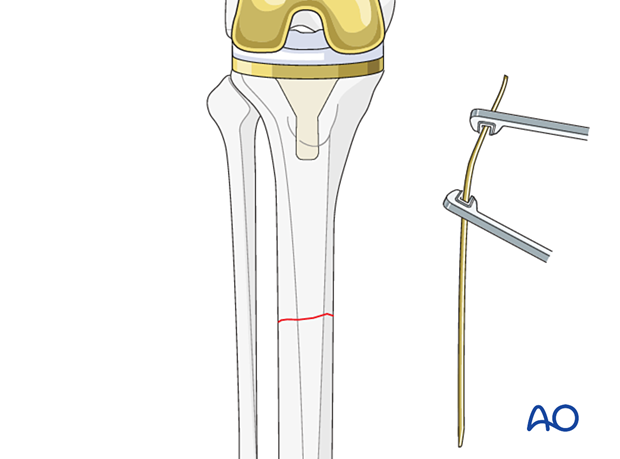
In some cases, the midline approach to the knee that was used for the knee arthroplasty will be extended in order to adequately expose the fracture.
When compression plating of a short oblique fracture is performed, the surgical approach should be selected to allow for the creation of appropriate axilla.
Small incisions may be made over the distal aspect of the plate utilizing fluoroscopy as a guide, in order to minimize larger surgical approaches.
Supine positioning with a bump under the ipsilateral greater trochanter helps face the patella forward.
Flexion of the knee can aid in fracture reduction and careful evaluation of preoperative radiographs will predict the need for flexion. A radiolucent triangle or a ramp for the extremity can be utilized based on the surgeon's preference. The following patient preparations can be used:
4. Reduction
The fracture site should be exposed, cleared of hematoma and debris, and reduced utilizing appropriate direct reduction maneuvers.
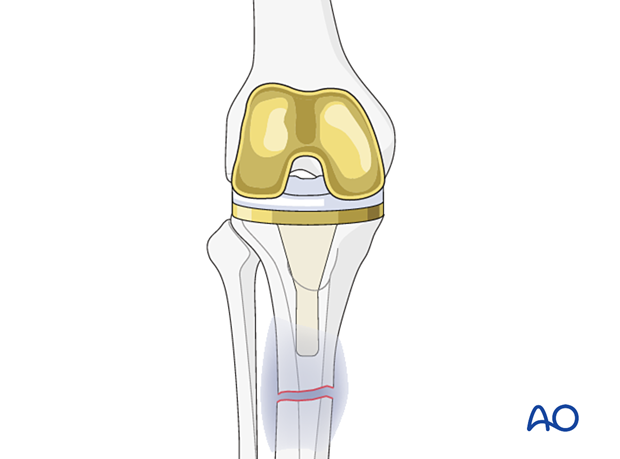
Plate contouring
The medial aspect of the tibia requires careful contouring of the plate. Small fragment plates are easier to contour.
Transverse fractures require under contouring at the fracture site according to standard techniques as described in the proximal tibia section of the AO Surgery Reference.
5. Fixation
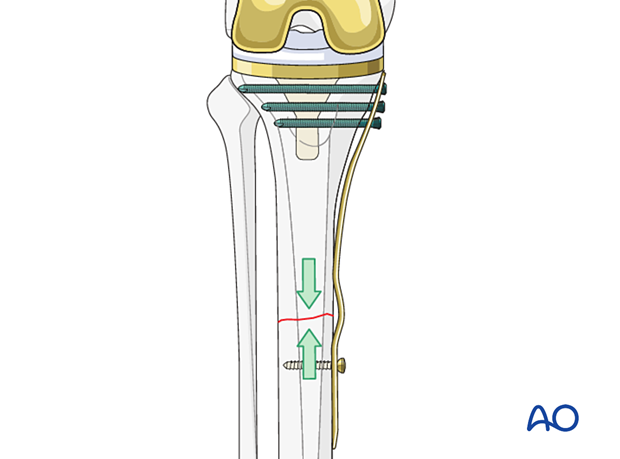
For transverse fractures, the plate should first be secured to the proximal tibia using either locking or non-locking screw fixation depending on bone quality. Often proximal screw fixation can be achieved both anterior and posterior to the fin of the knee arthroplasty. Insertion of screws through the cement mantle may be required to achieve adequate fixation.
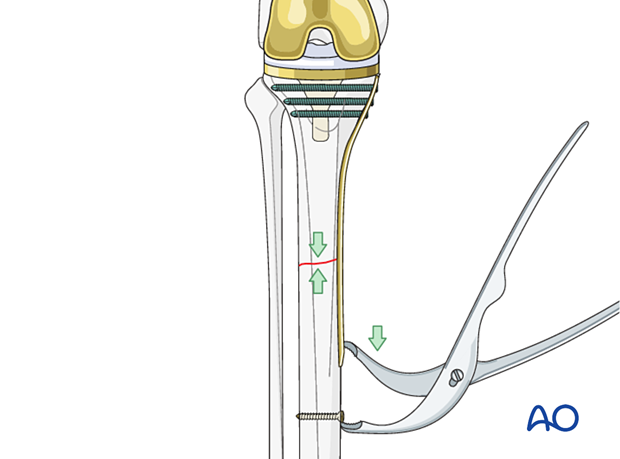
In short oblique fractures, the plate will be secured to the bone creating axilla.
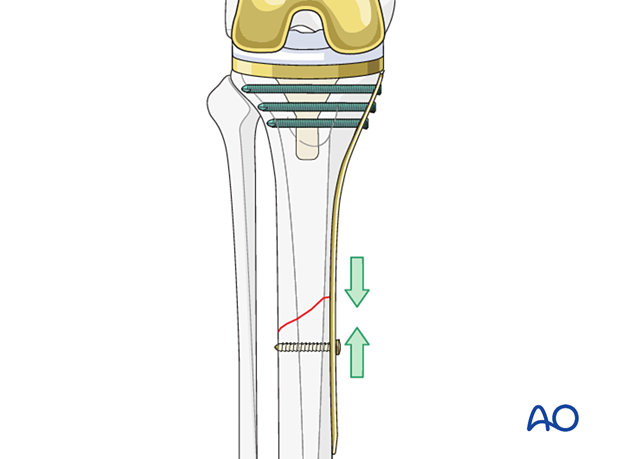
Initial compression can be achieved utilizing a Verbrugge clamp, after insertion of a push-pull screw distal to the plate.
Alternatively, an articulated tensioning device can be used if a large fragment plate is selected.
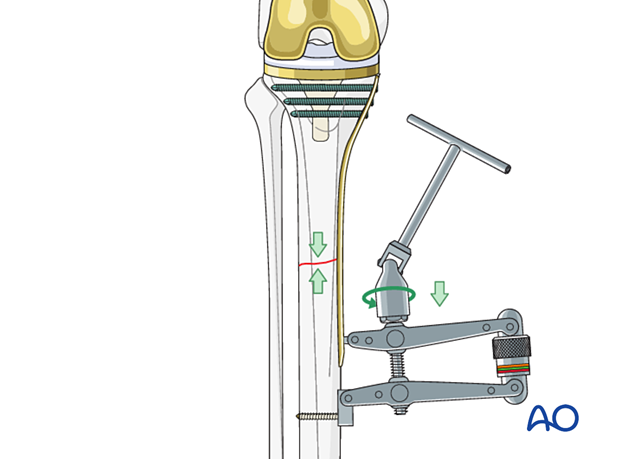
Compression can be secured through the insertion of screws in compression mode.
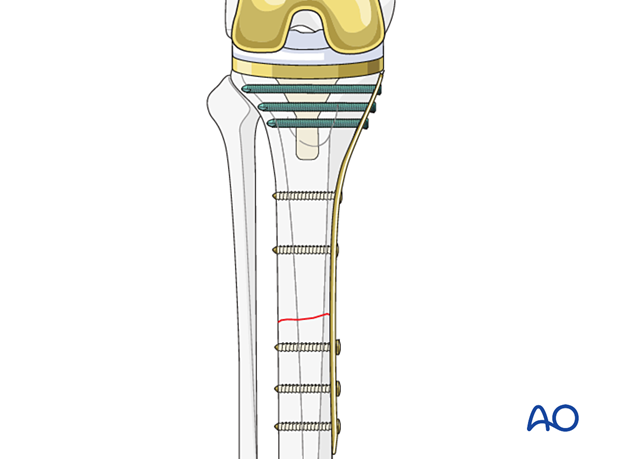
In oblique fractures, far cortical gapping can be minimized by inserting a lag screw perpendicular to the fracture plane.
6. Radiographic verification
Anteroposterior, mediolateral, and oblique radiographs of both the fracture site and the arthroplasty are obtained at the end of the procedure, to ensure that:
- There is no displacement
- The joint articulation is preserved
7. Aftercare
These fixation techniques will often allow early full weight-bearing postoperatively. Because of limited bone stock sometimes protective weight bearing will be needed until fracture consolidation is visible.
Knee bracing is not essential and should be considered optional for patient comfort.













