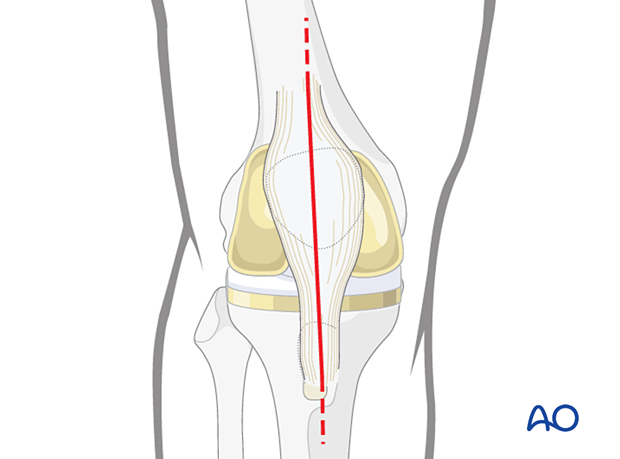
Midline longitudinal approach
1. Introduction
This universal approach is used for primary and revision total knee replacement. In periprosthetic fractures, variations of the approach can be used for fractures requiring medial and lateral arthrotomy as well as patellar fractures and antegrade tibial nailing.
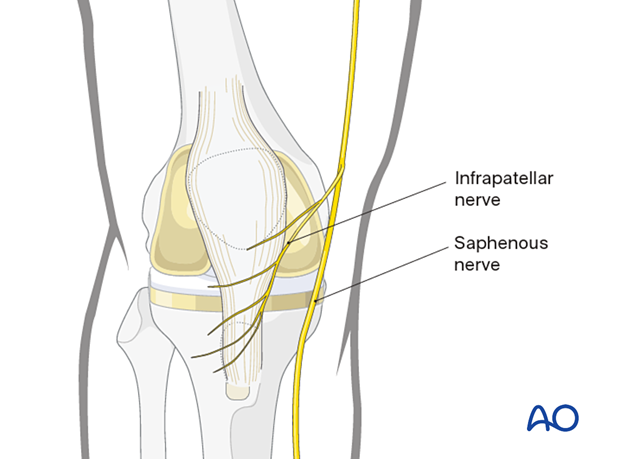
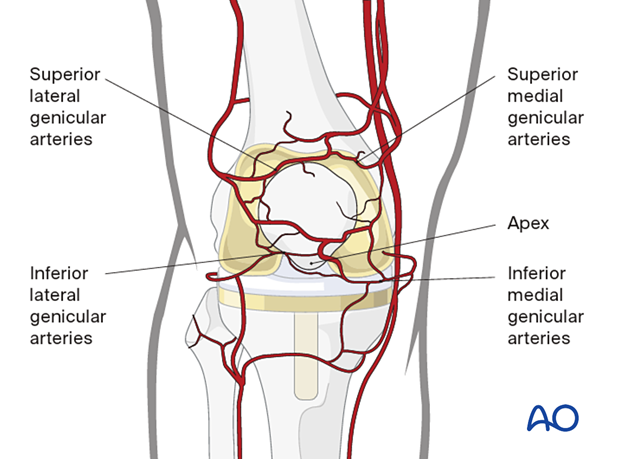
2. Surgical anatomy
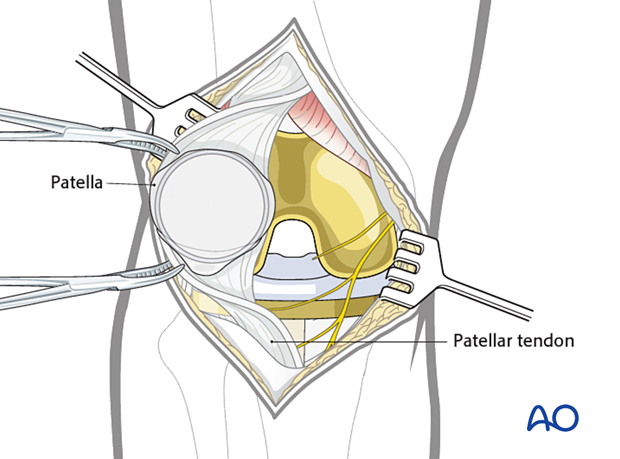
The saphenous nerve runs along the medial aspect of the distal femur. The infrapatellar branches of the saphenous nerve lie on the medial and inferior aspects of the patella and run across to the lateral side. Postoperatively, there is usually minor sensory loss to the lateral side of the scar, but significant saphenous nerve damage is avoidable. Occasionally, there may be postsurgical saphenous nerve neuroma formation which is rarely a significant problem.
The anterior surface is surrounded by an extraosseous arterial ring, which receives inflow from branches of the genicular arteries. This anastomotic ring supplies the patella through mid-patellar vessels, which penetrate the middle third of the anterior surface, and the polar vessels, which enter the apex.
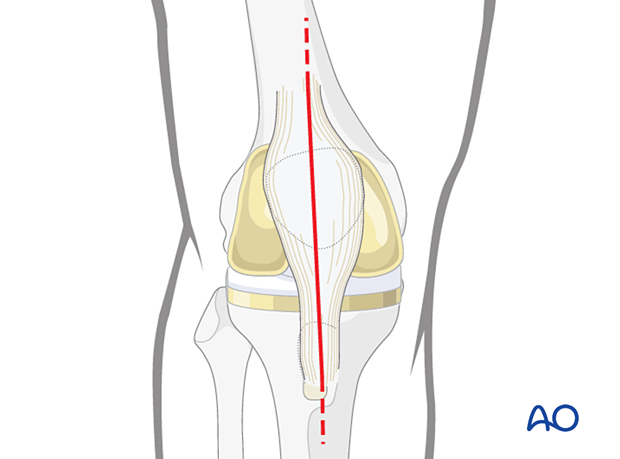
3. Longitudinal approach
The majority of the total knee arthroplasties are performed using a longitudinal midline incision. Thus, the same incision can be reused and extended proximally or distally as needed.
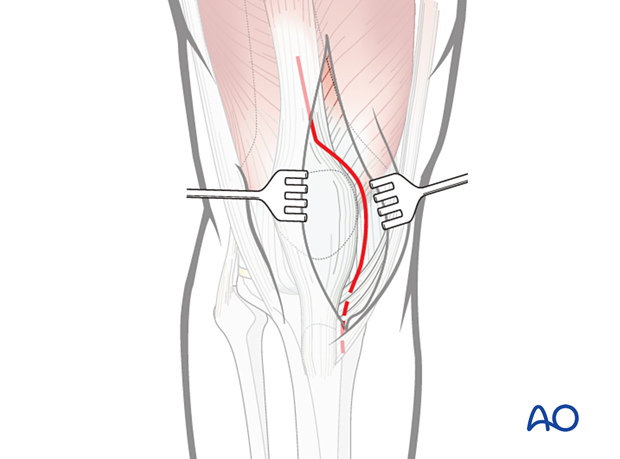
Full-thickness flaps should be developed to avoid damage to the skin blood supply.
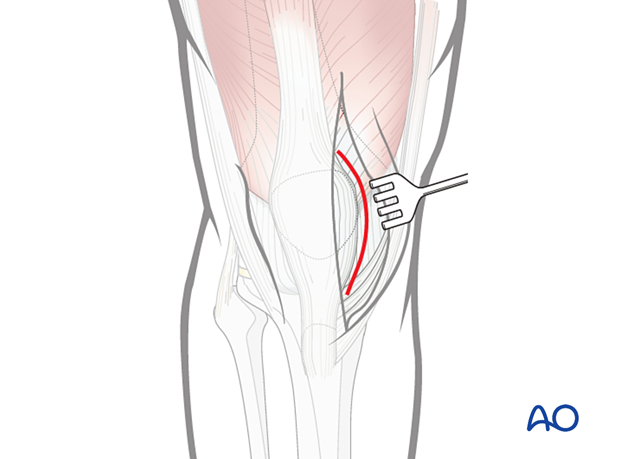
4. Arthrotomy
A medial parapatellar arthrotomy is routinely performed for knee arthroplasty surgery.
A lateral parapatellar arthrotomy is rare.
Incise the medial patellar retinaculum and open the joint capsule.
5. Proximal and distal extensions
Depending on the fracture configuration, the incision can be extended proximally to increase the exposure.
The incision can be extended more distally towards the tibial tubercle to increase the exposure.
The distal extension can be used in isolation for tibial intramedullary nailing.
Eversion of the patella is only necessary when dealing with patellar fractures and revision of the patellar component. Additional releases at the quadriceps, lateral retinaculum, or tibial tubercle may be needed to achieve safe exposure.
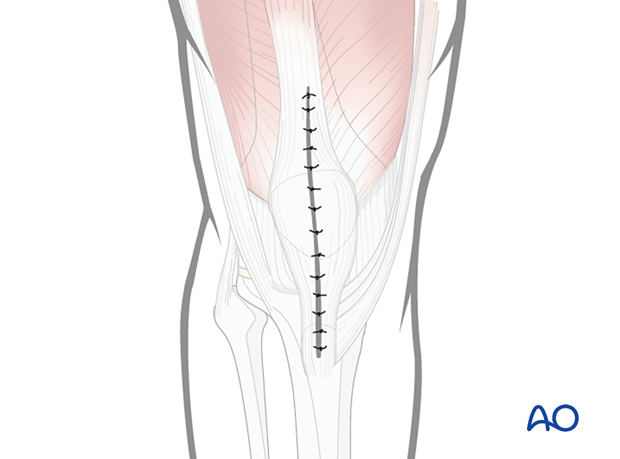
6. Wound closure
Before closure, irrigate the knee joint to remove any debris. Standard layered closure is performed. The use of a suction drain may be considered. Close the skin with staples or nonabsorbable sutures.