Plate
1. Principles
Introduction
Periprosthetic patella fractures occur typically through fall onto a bent knee. With this simple mechanism comes significant surgical care issues and potential complications. The difficulty in the treatment of a patella that has been resurfaced includes the diminutive size of the remnant patella and the disruption of the blood supply that occurs at the time of the knee arthroplasty. If the extensor mechanism is disrupted due to displacement of the fracture, then the patellar button is likely also unstable. This will therefore require open reduction and internal fixation in conjunction with the revision of the patellar component.
Preoperative planning is critical and can be complicated by the scatter produced by the metallic components during a CT scan. However, plain radiographs are often inadequate to understand the comminuted nature of these fractures.
A surgeon should be prepared for multiple modalities of fixation.
Debridement
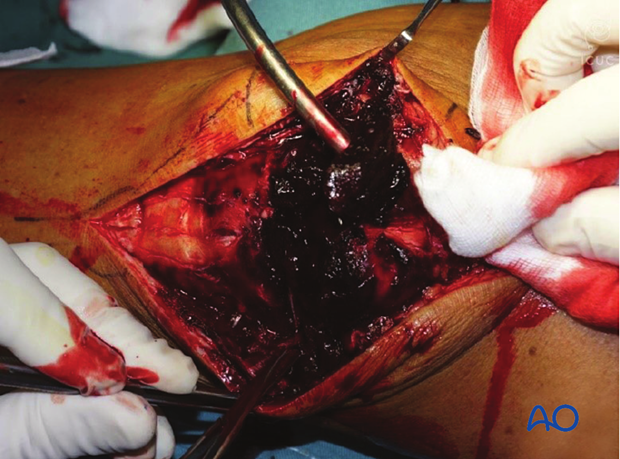
When exposure is complete, the surgeon will be able to evaluate the patellar button for stability. Occasionally the patient may have a peripheral fracture that may disrupt the extensor mechanism without disrupting the prosthetic patella. However, if the patella component is unstable, it should be removed with careful extraction of all cement.
The knee joint and fracture lines must be irrigated and cleared of the blood clot and small debris to allow exact reconstruction.
2. Patient preparation and approach
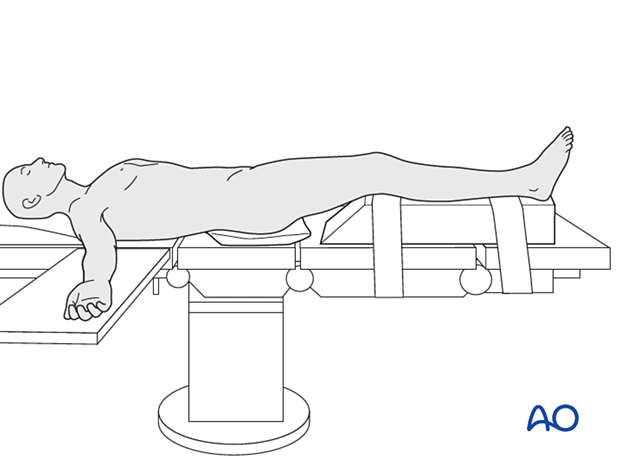
The patient should be positioned supine with the affected lower extremity on a ramp that will allow for full knee extension and ease of biplanar fluoroscopy.
The prior surgical incision should be utilized over the mid patella. The deep dissection should be carried out with an arthrotomy that will allow for exposure of the undersurface of the patella. Utilization of a proximal thigh tourniquet can be helpful during reconstruction. The surgeon may also choose to have appropriate polyethylene implants available for revision, particularly in knee replacements that have been in place for many years.
3. Reduction and fixation
Verification of reduction
A precise reconstruction of the articular surface is not possible or necessary when the patella has been previously resurfaced. However, restoration of the extensor mechanism and a recipient bed for a new patellar button are the ultimate goals.
The surgical exposure allows for the required visual confirmation of the reduction of both the ventral and dorsal surfaces of the patella.

Reduction and temporary fixation
The reduction of this fracture requires careful planning.
The largest fragments are reduced and temporarily fixed with K-wires.
In frontal/coronal (transverse) fractures, the reduction is easier with the knee extended.
Sagittal fractures are more easily reduced with the knee flexed.

Frequently, the use of several K-wires is required to hold smaller fragments to the larger fragments.

Plate application
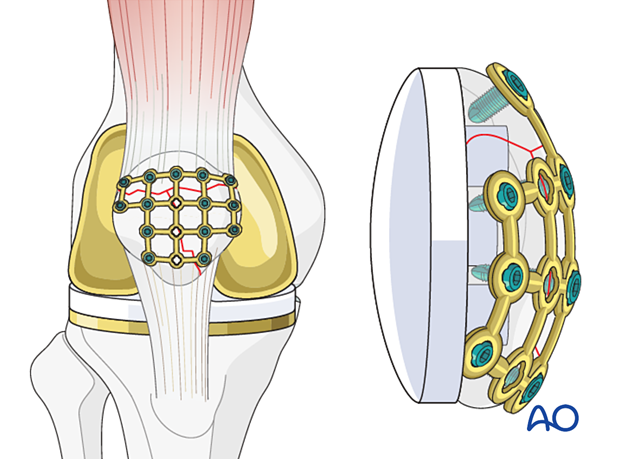
Plate selection on the subcutaneous cortex of the patella can be very challenging. It should be reserved for multifragmentary fractures that require multiplanar fixation.
Commonly a small fragment mesh plate is selected. This can be cut and contoured to precisely outline the fracture fragments of the patella. Locking fixation in these plates is helpful considering the significant forces across the patella fracture and the need for unicortical fixation.
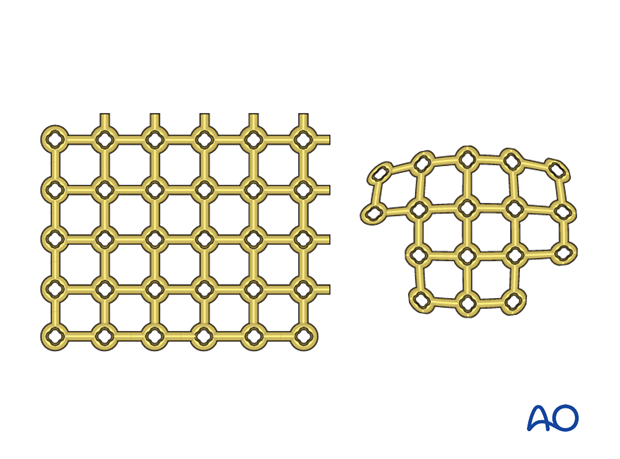
The plate is placed on the cortex in close apposition and a single limb of the plate can be bent around the inferior pole of the patella to allow for lag screw fixation of the plate.
Screws placed from the anterior cortex will typically be locking screws to allow for unicortical placement.
Placement of the revision patellar button must be carefully planned to avoid screw peg interference.
Patella component revision
After the successful reconstruction of the patellar anatomy, the patellar button can be revised. Please refer to the dedicated section of the AO Surgery Reference.
4. Aftercare
The patient can typically be full weight-bearing in extension until wound healing. Gentle range of motion exercises can be continued until bony consolidation.













