Patella component revision with or without ORIF
1. Preoperative planning
The surgeon should prepare:
- A patella component which is compatible with the patient's knee replacement system.
- For ORIF of the patellar fracture.
- For a patellar salvage procedure.
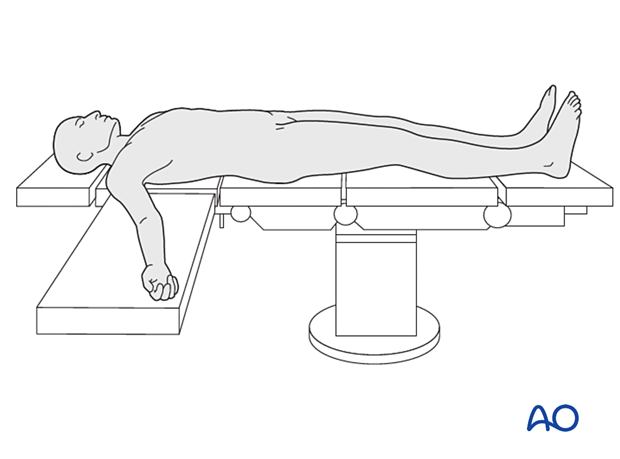
2. Patient preparation
The patient is placed in the supine position. A radiolucent table may facilitate intraoperative fluoroscopy if required.
3. Surgical approach
The surgeon can use the previous surgical skin incision followed by a medial parapatellar arthrotomy.
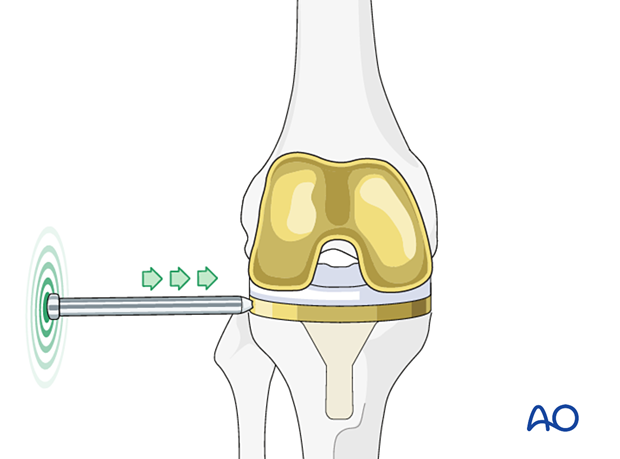
4. Verification of component stability
Femoral and tibial component
After exposure of the knee joint, the surgeon must assess the fixation stability and the rotational alignment of the tibial and femoral components. The polyethylene insert should be assessed for wear.
5. Patella component revision
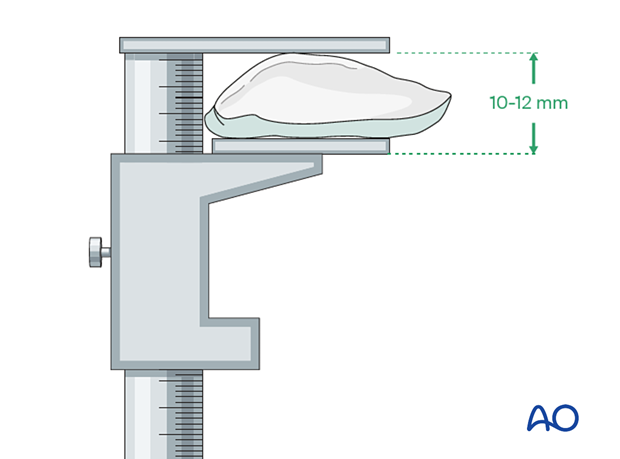
Evaluation of bone stock
The loose patella component is removed, and the remaining bone stock is examined.
If the thickness of the patella measured with a caliper is less than 10-12 mm, there is not enough bone stock to accept a new patella component.
If the bone quality is not ideal for cement fixation, the surgeon may choose against the insertion of a new component.
In these circumstances, a patelloplasty or patellectomy is considered.
If there is enough bone stock, a new patella component can be inserted following fixation of the patella fracture.
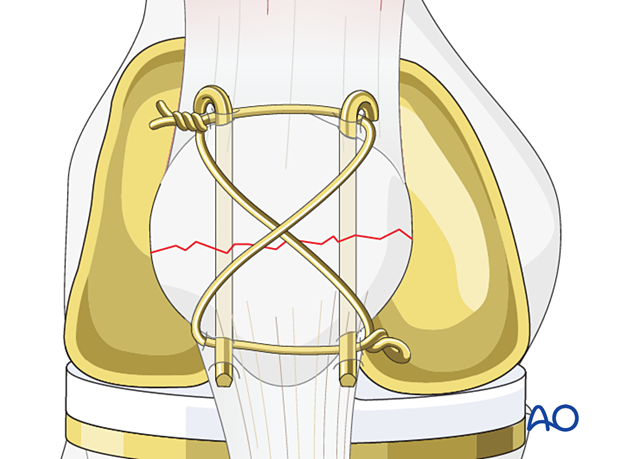
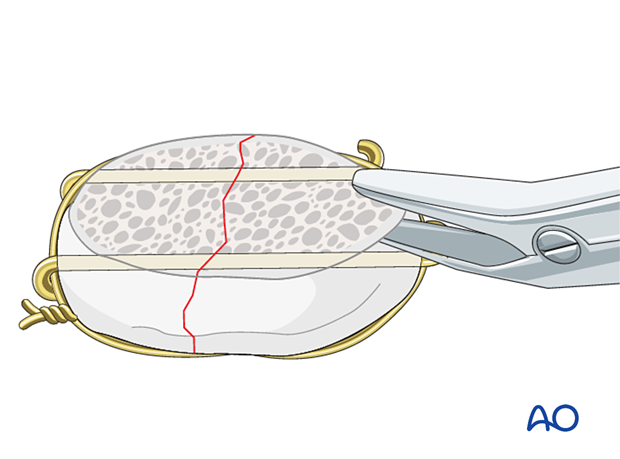
Fracture fixation
Any fracture will need to be reduced and fixed either with a cerclage wire, lag screws, or miniplates to restore the integrity of the extensor mechanism. Details for these procedures can be found in the patella section of the AO Surgery Reference.
Patelloplasty
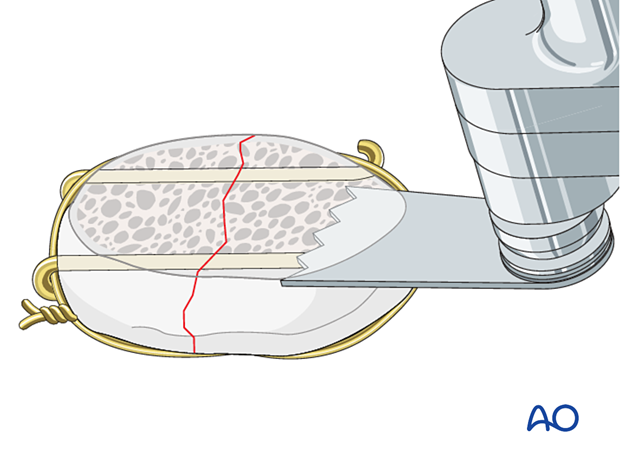
Patelloplasty is performed after fixation of the patella using small oscillating saws or bone rongeurs to reshape the remaining patella to achieve optimal tracking in the femoral trochlea.
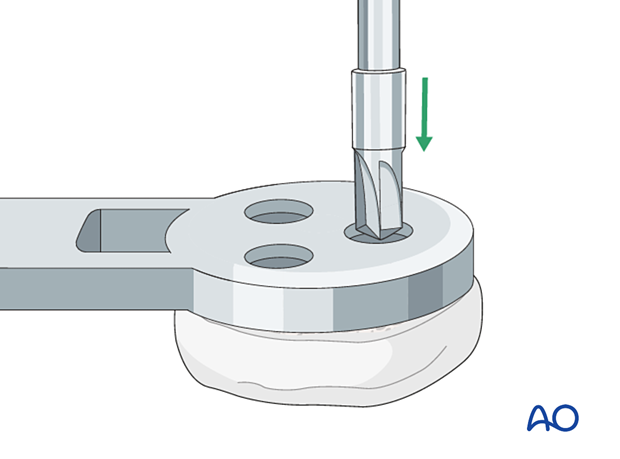
Patella preparation
A saw is used to recut the patella down to good cancellous bone surface.
The proper component size is selected using a template. Fixation holes are drilled into the patella using the patella jig.
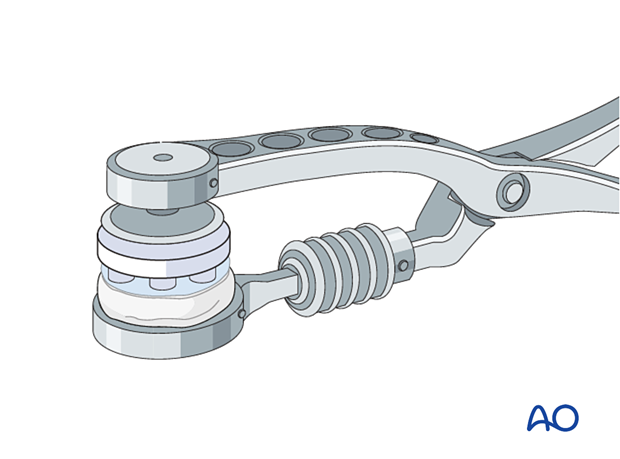
Cementing
The new component is cemented to the bone bed and held in place using the patella clamp until the cement has hardened.
If patellar tracking is not ideal, a lateral retinacular release and medial imbrication can be performed.

6. Aftercare
The patient can be mobilized with full weight-bearing and active range of motion immediately after surgery.













