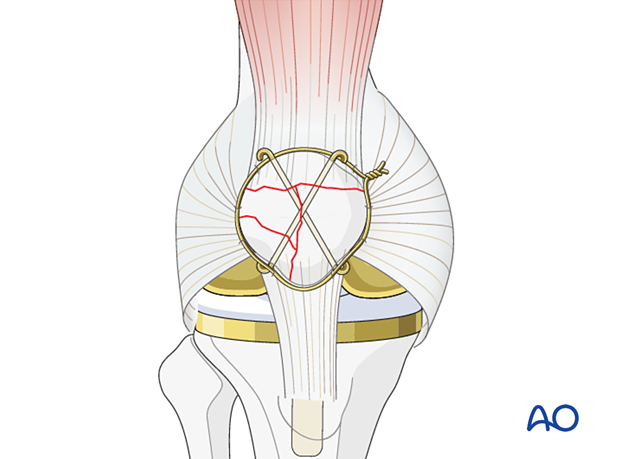
Cerclage wire
1. Introduction
Periprosthetic patella fractures occur typically through fall onto a bent knee. With this simple mechanism comes significant surgical care issues and potential complications.
The difficulty in treatment of a patella that has been resurfaced include the diminutive size of the remnant patella and the disruption of the blood supply that occurs at the time of the knee arthroplasty. If the extensor mechanism is disrupted due to displacement of the fracture, then the patellar button is likely also unstable. This will therefore require open reduction and internal fixation in conjunction with revision of the patellar component.
Preoperative planning is critical and can be complicated by the scatter produced by the metallic components during a CT scan. However, plain radiographs are often inadequate to understand the comminuted nature of these fractures.
A surgeon should prepare for multiple modalities of fixation.
2. Patient preparation and approach
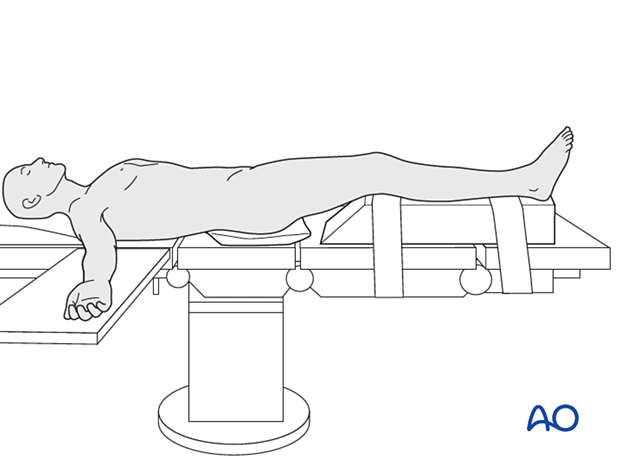
The patient should be positioned supine with the affected lower extremity on a ramp that will allow for full knee extension and ease of biplanar fluoroscopy.
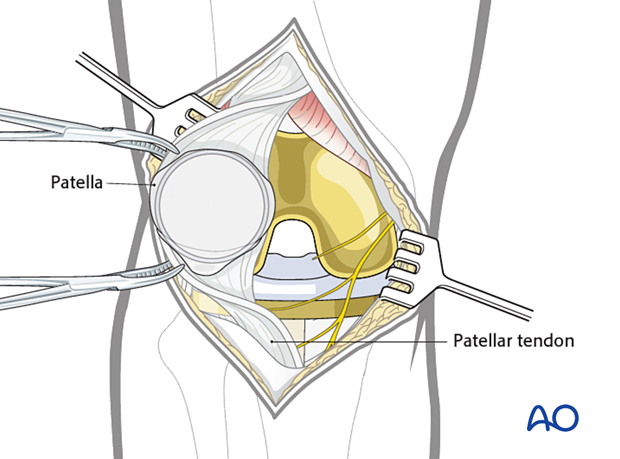
The prior surgical incision should be utilized over the mid patella. The deep dissection should be carried out with an arthrotomy that will allow for exposure of the undersurface of the patella. Utilization of a proximal thigh tourniquet can be helpful during reconstruction. The surgeon may also choose to have appropriate polyethylene implants available for revision, particularly in knee replacements that have been in place for many years.
3. Cerclage wire
Interrogation of patellar component
When exposure is complete, the surgeon will be able to evaluate the patellar button for stability. Occasionally the patient may have a peripheral fracture that may disrupt the extensor mechanism without disrupting the prosthetic patella. However, if the patella component is unstable, it should be removed with careful extraction of all cement.
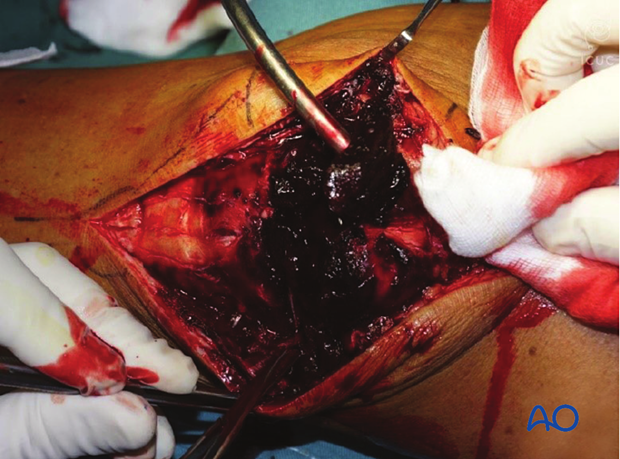
Fracture debridement
The knee joint and fracture lines must be irrigated and cleared of blood clot and small debris to allow exact reconstruction.
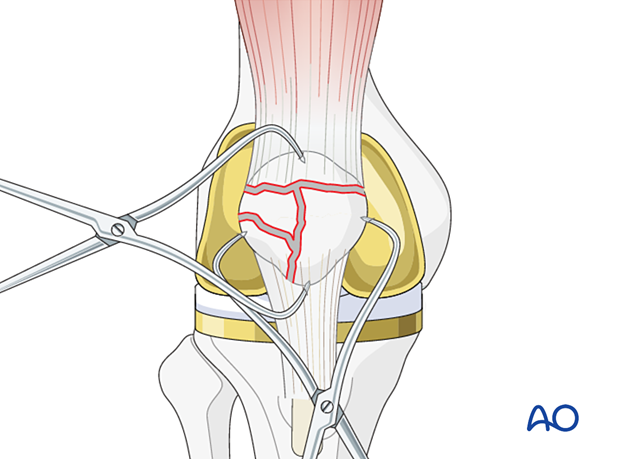
Reduction
Reduce the major fracture fragments using a pointed bone reduction forceps or tenaculum. Transverse fractures are more easily reduced with the leg in extension and sagittal fractures are more easily reduced with the leg in flexion.
Precise reconstruction of the articular surface is not possible or necessary when the patella has been previously resurfaced. However, restoration of the extensor mechanism and a recipient bed for a new patellar button are the ultimate goals.
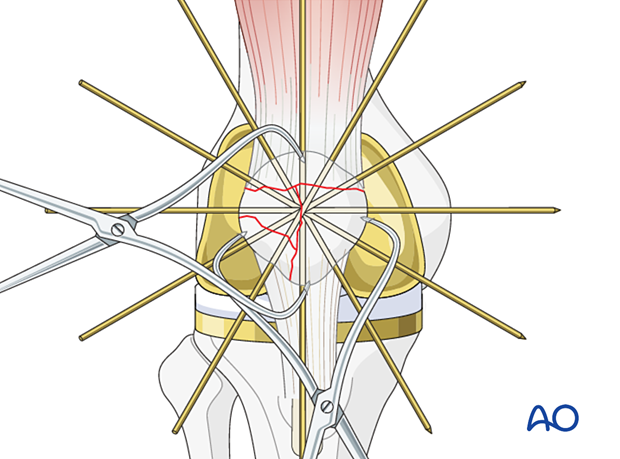
Provisional stabilization
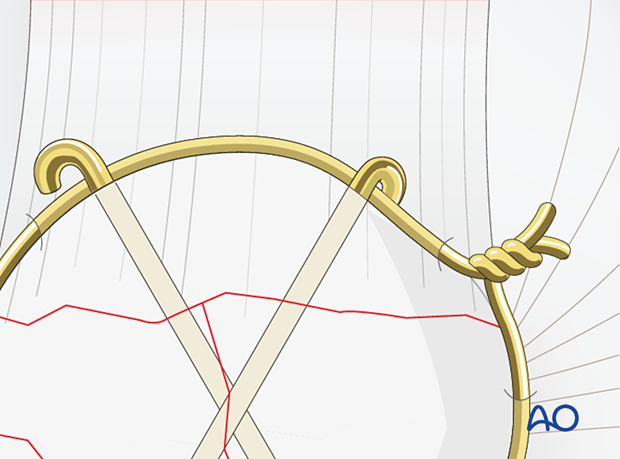
When the fracture configuration is amenable to cerclage stabilization, it is helpful to insert multiple K-wires in a stellate pattern. This will not only allow for stabilization of multiple fracture fragments but also provide a simple aid for cerclage.
Inserting the cerclage wire
Choose a wire of enough strength to withstand the tensile forces generated in the cerclage (1.0 – 1.25 mm diameter / 18-16 gauge wire).
The wire should be as close as possible to the bone throughout its whole course both superiorly and inferiorly. The use of a large bore injection needle may be helpful.
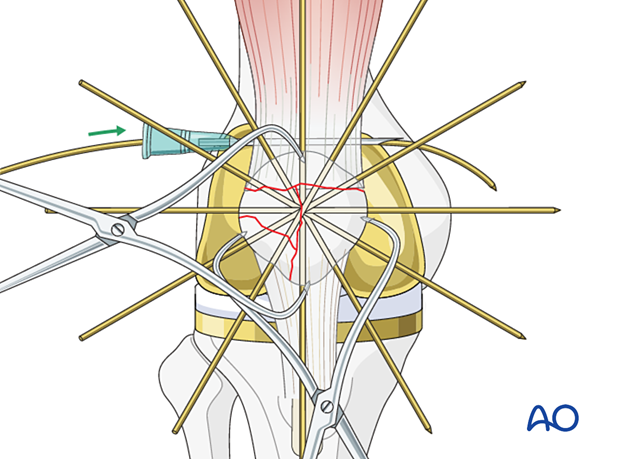
The wire is then similarly threaded around the circumference of the body of the patella and its lower pole, as illustrated.
With the patella everted, such that the undersurface is easily visualized, the cerclage wire can be woven between the provisional K-wires.
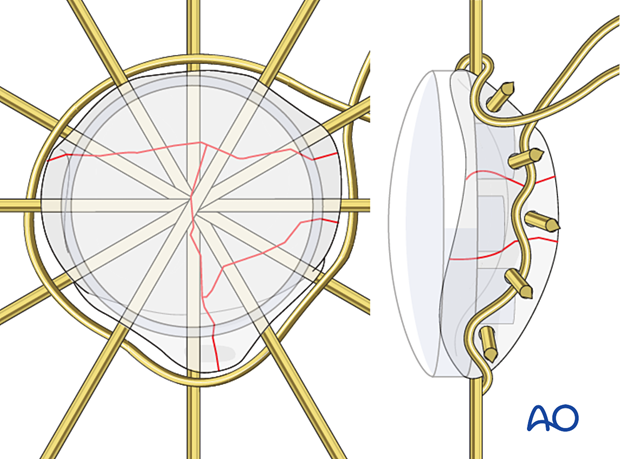
Wire tightening
Loosely prepare the wire twist ensuring that each end of the wire spirals equally - the twist should not comprise one spiral around a straight wire.
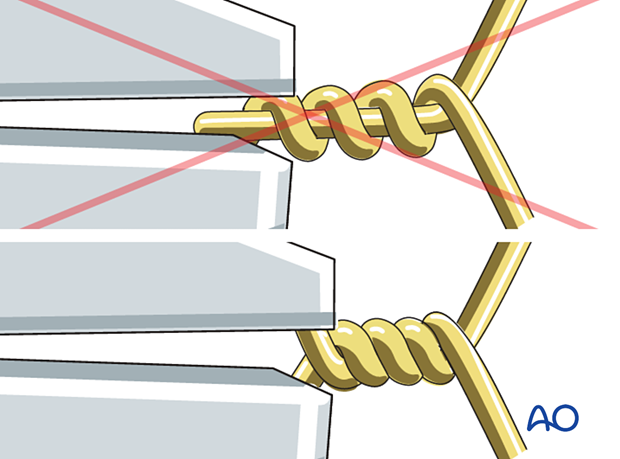
Carefully tighten the wire while pulling away from the patella as the wires are twisted. Avoid over-tightening as this may distort the overall shape of the patella. The provisional K-wires will help prevent this deformation.
The wires should be twisted at least 5 times to prevent fixation failure. When stainless steel wires tighten, they will lose the surface sheen and if tightened further the wire may break.
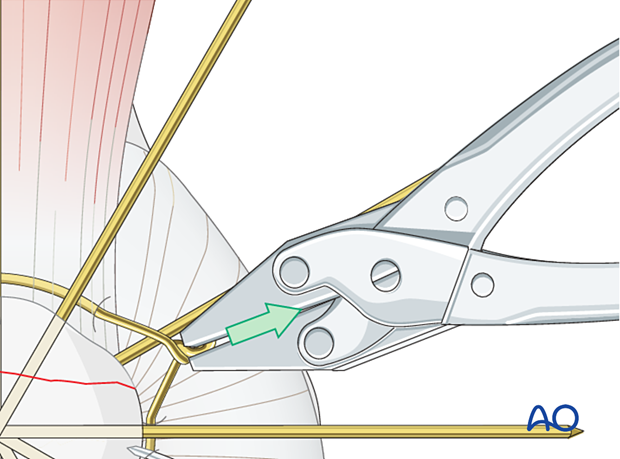
When the correct tension is achieved, twist and trim the wire ends.
The provisional K-wires can be either removed or cut and bent and left in place.
Care should be taken finally to position the twisted wire into deeper soft-tissue muscle layers, if possible.

Patella component revision
After the successful reconstruction of the patellar anatomy, the patellar button can be revised. Please refer to the dedicated section of the AO Surgery Reference.
4. Aftercare
The patient can typically be full weight-bearing in extension until wound healing. Gentle range of motion exercises can be continued until bony consolidation.













