Bridge plate
1. Introduction
Nonoperative treatment of periprosthetic fractures of the proximal tibia often leads to nonunion or malunion. However, operative stabilization can be challenging because of the limited available bone stock for fixation. Bone healing is expected to proceed in a secondary fashion. This requires indirect reduction techniques with bridge plating constructs.
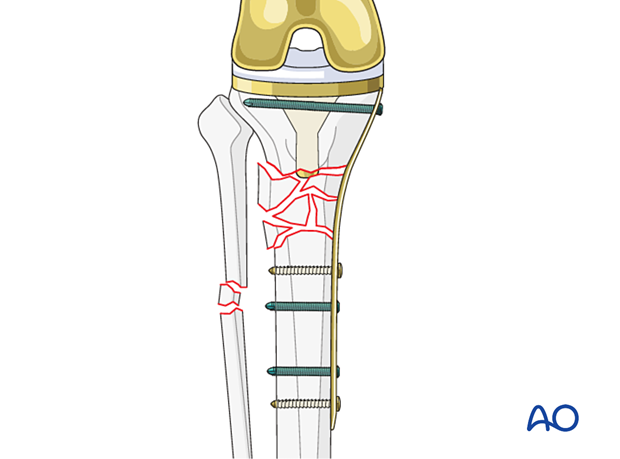
Plate selection
Fracture fixation is largely dependent on the anatomy of the fracture and the selected approach. The proximal tibia requires the use of low-profile plating constructs due to poor soft tissue coverage. Medial, lateral, and posteromedial options are possible.
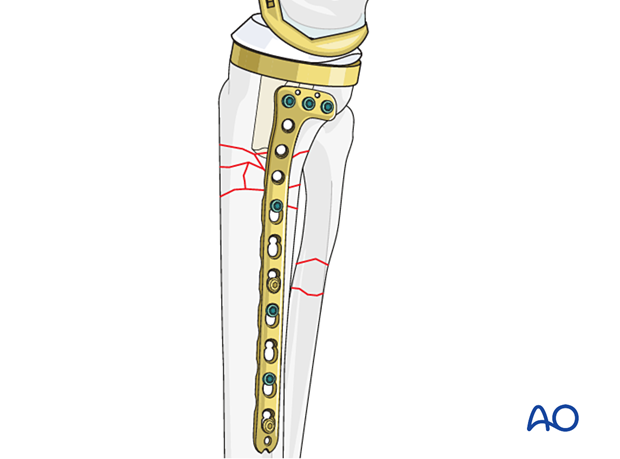
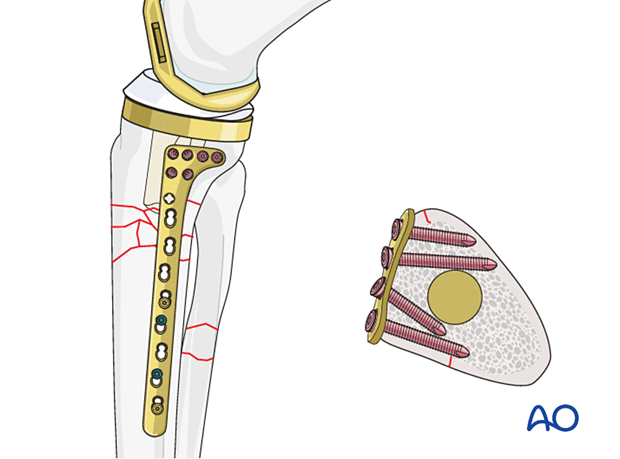
Variable angle locking options are advantageous in the proximal tibia when screw placement is limited by the prosthesis and the cement mantle.
Some plates offer small fragment and large fragment options at opposite ends of the plate, which allows for a low-profile option on the proximal tibia (metaphyseal plate).

2. Patient preparation and approach
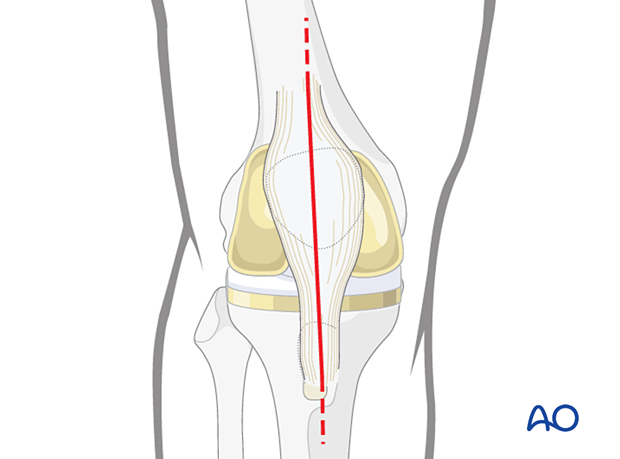
In some cases, the midline approach to the knee that was used for the knee arthroplasty will be extended in order to adequately expose the fracture.
Small incisions may be made over the distal aspect of the plate utilizing fluoroscopy as a guide, in order to minimize larger surgical approaches.
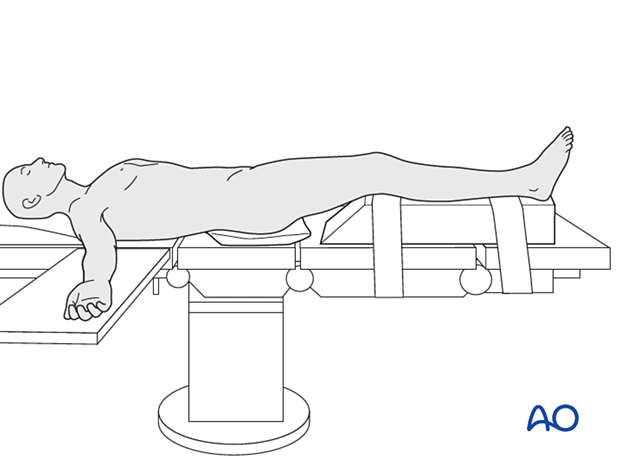
Supine positioning with a bump under the ipsilateral greater trochanter helps face the patella forward.
Flexion of the knee can aid in fracture reduction and careful evaluation of preoperative radiographs will predict the need for flexion. A radiolucent triangle or a ramp for the extremity can be utilized based on the surgeon's preference. The following patient preparations can be used:
3. Reduction
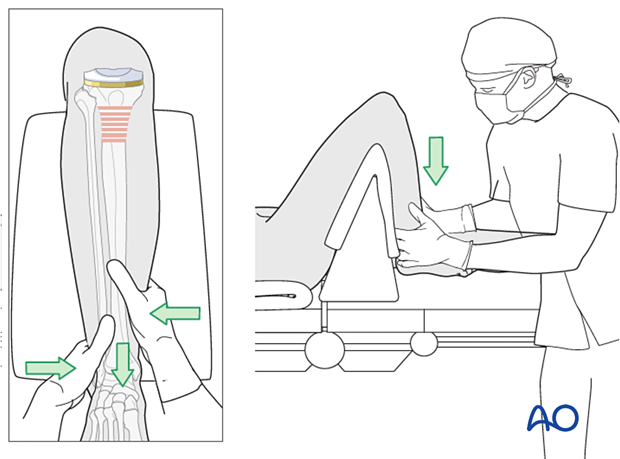
Indirect techniques of reduction are used. This includes:
- Traction
- Manual limb manipulation
- Use of external fixator
Preoperative or intraoperative radiographs of the contralateral extremity should be obtained. This in combination with clinical assessment of length and rotation will allow for accurate reconstruction of the injured extremity.
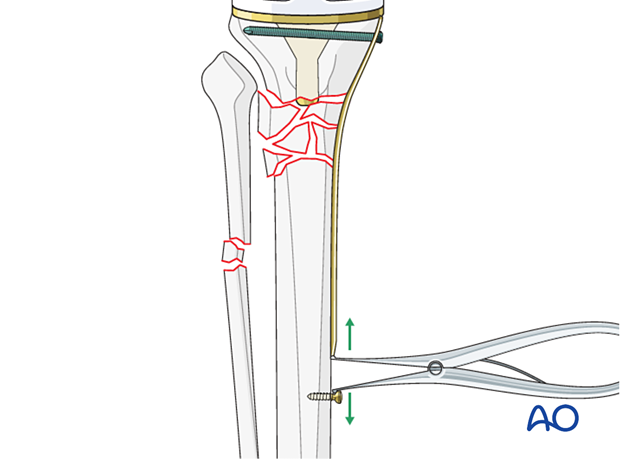
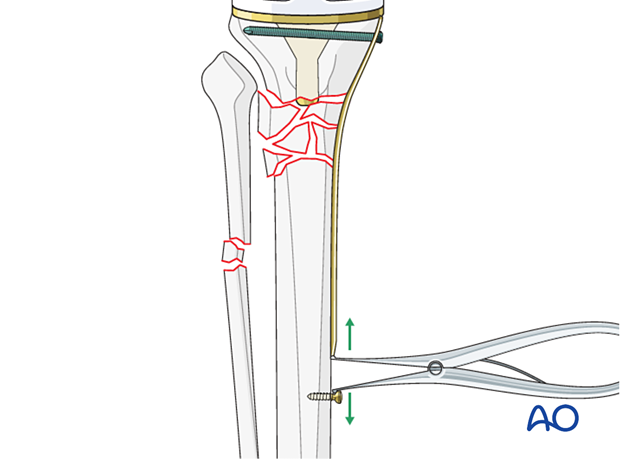
Push-pull screws in combination with a Verbrugge clamp or a laminar spreader can be utilized to fine-tune a reduction.
4. Plate contouring and fixation
The plate selected should be perfectly contoured to match the bone to maintain the indirect reduction when it is secured to the bone.
Small fragment plates are easier to contour and allow locked screws anterior and posterior to the keel.
Typically, fixation into the proximal tibia will first be performed. AP and lateral radiographs are then utilized to confirm reduction and implant placement before distal stabilization.
If the plate is imperfectly contoured to the bony anatomy, locking screw fixation can be used distally to prevent secondary loss of reduction.
Options for additional stability
Additional stabilization can be achieved with locking and nonlocking screw fixation above and below the fracture site.
If there is no room for bicortical screw fixation, different options may be used around the component stem to secure the plate:
- Unicortical locking screw fixation
- Cerclage cables integrated into the plate
- Locking attachment plate
For additional details on these implants please refer to adjunct plate options.
5. Radiographic verification
Anteroposterior, mediolateral, and oblique radiographs of both the fracture site and the arthroplasty are obtained at the end of the procedure, to ensure that:
- There is no displacement
- The joint articulation is preserved
6. Aftercare
Because of limited bone stock sometimes protective weight bearing will be needed until fracture consolidation is visible.
Knee bracing is not essential and should be considered optional for patient comfort.













