Revision arthroplasty with ORIF
1. Principles and strategy
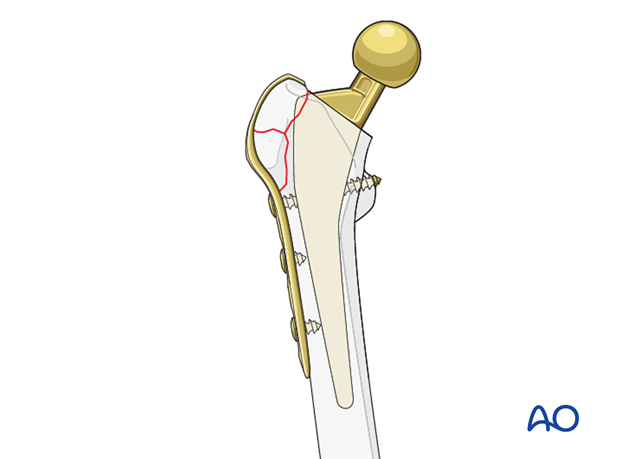
It is important to reconstruct a stable hip joint and to achieve rigid stem fixation in the distal fragment. Restoration of leg length, alignment, and rotation are equally important.
The arthroplasty revision should be preferably addressed first to reconstruct a stable hip joint. Internal fixation is then performed to reestablish bone stock.
Note on approaches
The surgeon should use the surgical approach that is the most familiar to him/her for any total hip arthroplasty.
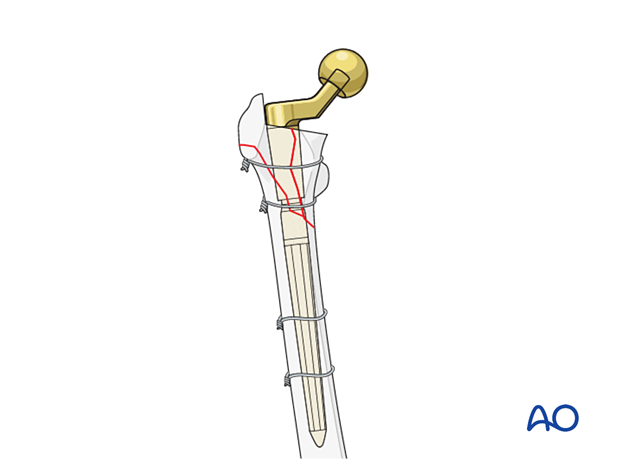
Extensile approach is necessary to access the fracture site for exposure and removal of the prostheses, revision of prostheses, and reduction and placement of fixation devices, such as cerclage wires, cables, strut grafts, or plates for fracture fixation.
2. Revision arthroplasty
Different options are available based on surgeon's preference and classification of periprosthetic fractures:
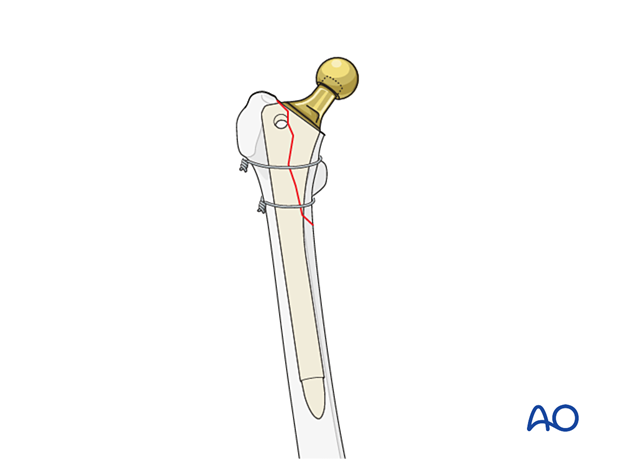
3. Fixation (ORIF)
4. Aftercare following a femoral revision
Physiotherapy guidelines
Routine physiotherapy protocols for elective total hip arthroplasty is followed.
Early mobilization is recommended. Weight bearing status is individualized based upon fixation and implant stability.
Hip dislocation precautions are given to the patient.
Imaging
Postoperative radiographs can be made at 2 to 3 weeks to determine maintenance of satisfactory fracture reduction and fixation, no evidence of stem subsidence, or fracture displacement.
Follow-up radiographs can be made at 6 to 8 weeks after surgery to determine sufficient fracture fixation to increase the weight bearing status, and physical activities.
Future follow-up is similar to the routine and standard protocol for total hip arthroplasty.