Open reduction - Plate fixation
1. General considerations
Introduction
Diaphyseal fracture healing in pediatric patients occurs more rapidly as the periosteum has the ability to form new bone. Therefore, periosteal stripping or compression should be avoided.
Open plating is less biologically favorable because soft-tissue and especially periosteal stripping will slow fracture healing. In addition, muscle dissection can contribute to discomfort and joint stiffness.
Soft-tissue dissection should be minimized during open plating. The approach that involves the least dissection of the fracture site to obtain stable fixation is preferred.
There should be at least three bicortical cortical or two locking head screws in each main fragment.
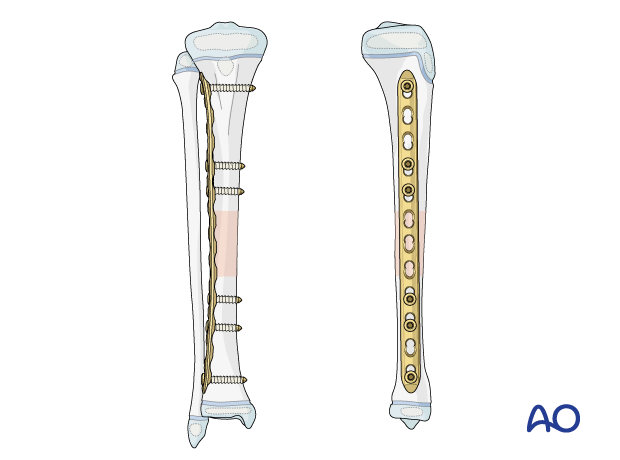
Typically, the plate is applied laterally as there is better soft-tissue coverage. If there is lateral soft-tissue damage, medial plating may be selected as an alternative.
In this procedure, plating of a generic fracture of the middle third of the tibia is shown.
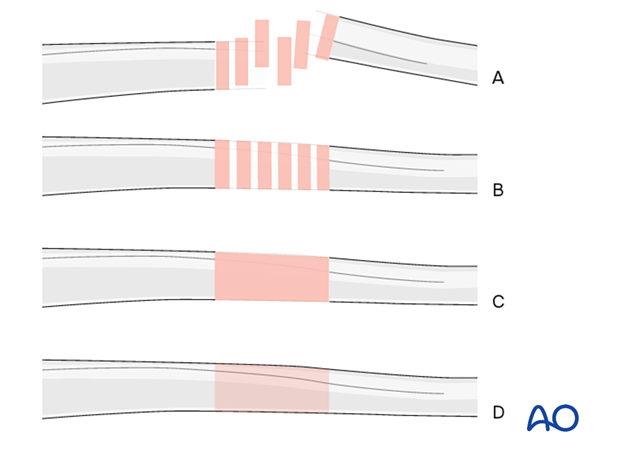
Throughout this section, generic fracture patterns are illustrated as:
- Unreduced
- Reduced
- Reduced and provisionally stabilized
- Definitively stabilized
2. Implant selection
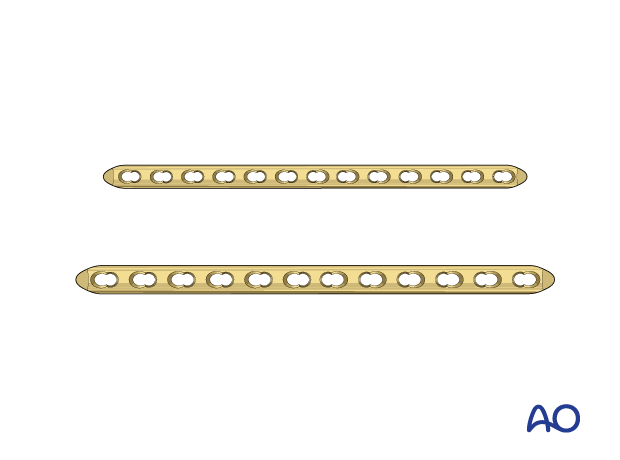
For younger children, a 3.5 mm plate can be used.
For older children and adolescents, a narrow 4.5 mm plate is typically used.
A locking plate is a good option for fractures with a short end segment. The plate does not need to be contoured precisely to fit the bone, as it functions as an internal fixator. Attaching it to the bone does not alter fracture alignment, as locking screws do not pull the main bone fragments to the implant. If cortical screws are used, contouring is important.
3. Patient preparation and approaches
Patient positioning
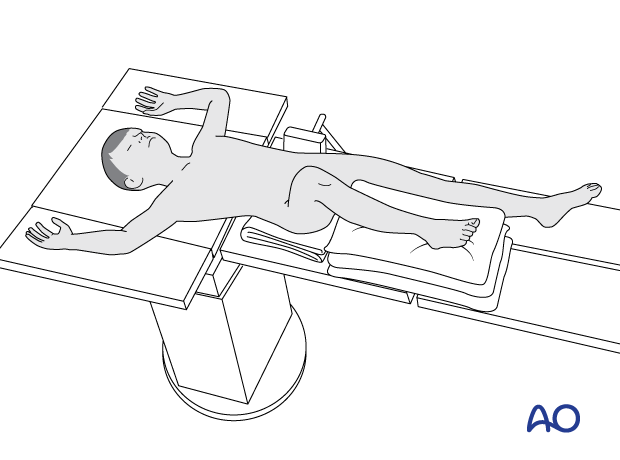
Place the patient in a supine position on a radiolucent table.
Elevate the lower leg with a stack of towels.
Approaches
For this procedure, an anterolateral approach is typically used.
If there is lateral soft-tissue damage, an anteromedial approach for medial plating may be selected.
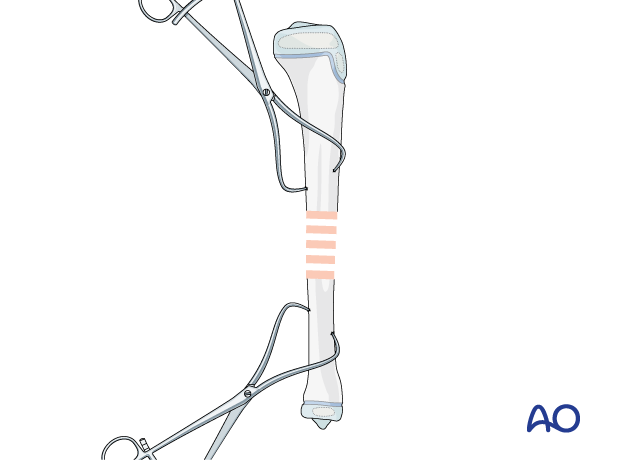
4. Reduction
After extraperiosteal exposure of the tibia, perform direct reduction using manual traction and/or bone reduction forceps.
Fracture reduction can be observed directly.
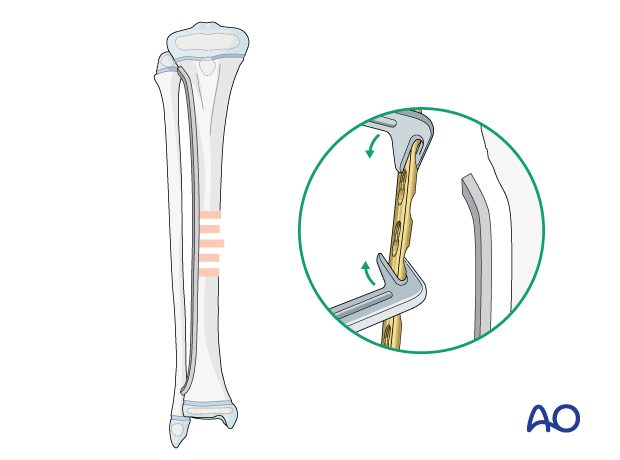
5. Plate contouring
Depending on the planned location, proximal and distal contouring of the plate may be necessary.
Contouring is aided by a stable provisional reduction and a malleable template that can be shaped along the bone surface. The malleable template is then used as a guide for shaping the plate to the bone.
6. Fixation
Plate fixation of tibial shaft fractures is typically performed in bridging mode as described in the following basic technique.
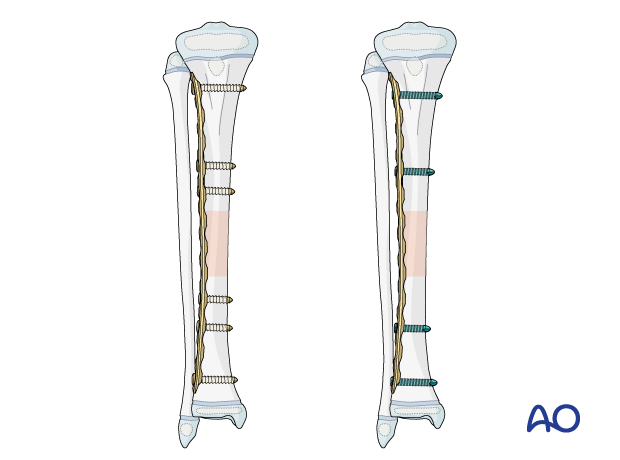
Either cortical, locking head, or a combination of screws may be used.
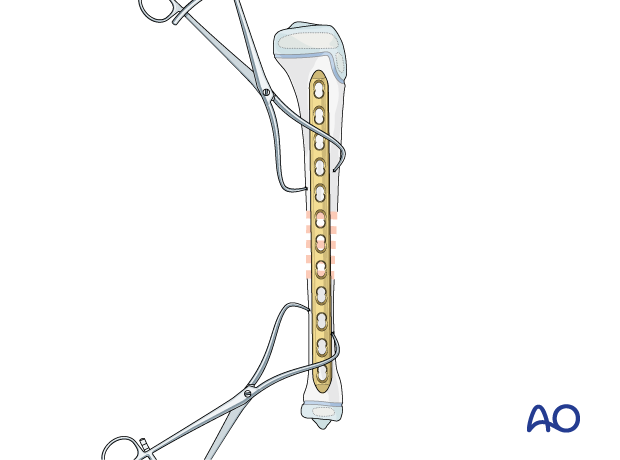
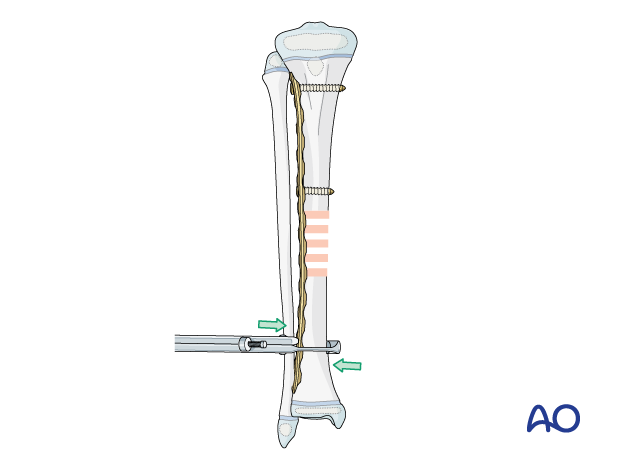
Application of the plate
Avoid periosteal stripping when exposing the bone for plate fixation.
Position the plate over the fracture so that at least three holes are available in the proximal and distal fragments.
Avoid compression of the perichondral ring by the plate.
Screw insertion
Insert the first screw close to the fracture site.
Confirm plate position relative to the other main fragment before placing the second screw.
Insert the second screw through the plate in the same fragment and tighten both screws.
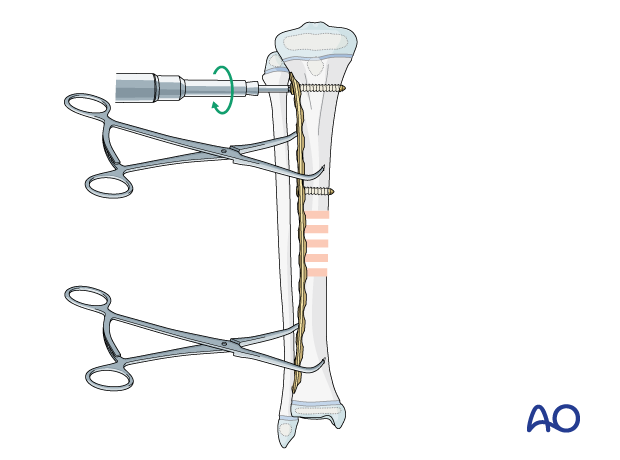
If the construct is unstable, fix the plate to one fragment and then reduce the other fragment onto the plate, using a bone holding forceps.
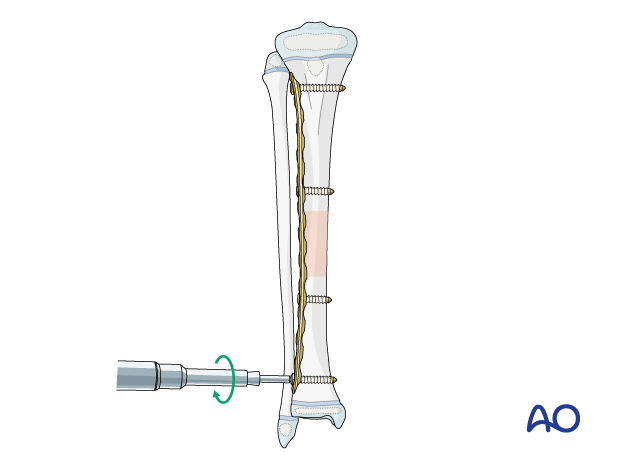
Assessment of rotational alignment
Confirm rotation, translation, and angular alignment of the tibia clinically and radiographically before fixing the second fragment.
Insertion of screws in the other main fragment
Insert the third and fourth screws in the other main fragment.
Finalizing plate fixation
Insert the remaining screws so there are at least three bicortical cortical or two locking head screws in each main fragment.
7. Final assessment
Compare leg length and rotation with the uninjured leg.
Confirm and document the final construct with an image intensifier in two planes.
8. Aftercare
Postoperative documentation
X-rays in two planes (AP and lateral) of the tibia with adjacent joints should be taken to confirm fracture reduction.
Immediate postoperative care
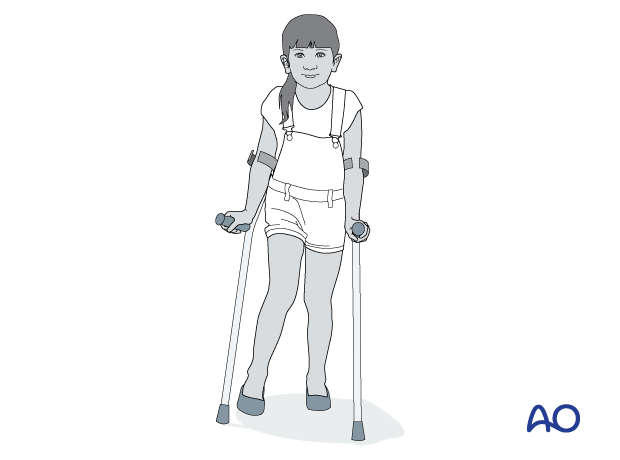
Toe-touch weight bearing is recommended for 2–6 weeks and depends on fracture stability.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Follow-up
Clinical follow-up is undertaken to check wound healing.
A radiological follow-up for bone healing should be taken after about 4–6 weeks.
Mobilization
Graduated weight bearing is usually possible after early clinical and radiological signs of consolidation.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be necessary in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms and function.
Implant removal
Implant removal is not mandatory and requires a risk-benefit discussion with patient and carers.
A medial subcutaneous plate may cause local soft-tissue irritation.
Follow-up for growth disturbance
Leg length should be evaluated up to 2 years following injury due to the effect of growth stimulation.













