Epiphysiolysis with/without metaphyseal wedge (Salter-Harris I and II)
Definition
Epiphyseal fractures of the proximal humerus are mainly Salter-Harris type-I and type-II fractures. These fractures are classified as 11-E/1.1 and 11-E/2.1, respectively.
Further characteristics
Proximal humeral fractures are common in children and often occur through the active proximal physis. This contributes to 80% of humeral growth and is therefore responsible for predictable healing and remodeling. This decreases the closer the patient is to skeletal maturity.
Read about the developmental anatomy in:
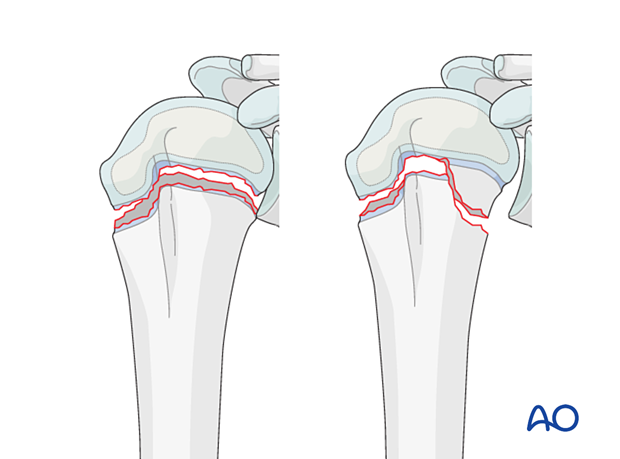
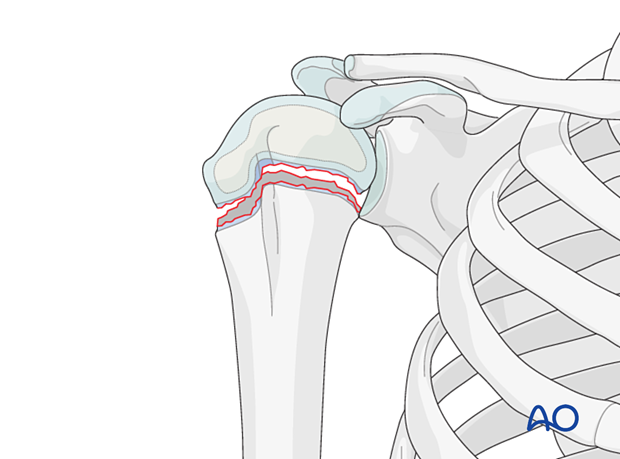
Epiphysiolysis (Salter-Harris I)
Salter-Harris type-I fractures are physeal injuries without epiphyseal or metaphyseal extension.
This fracture pattern is caused by significant traction and should raise concerns about the mechanism of injury.
They are seen in neonates and nonaccidental injuries in younger children.
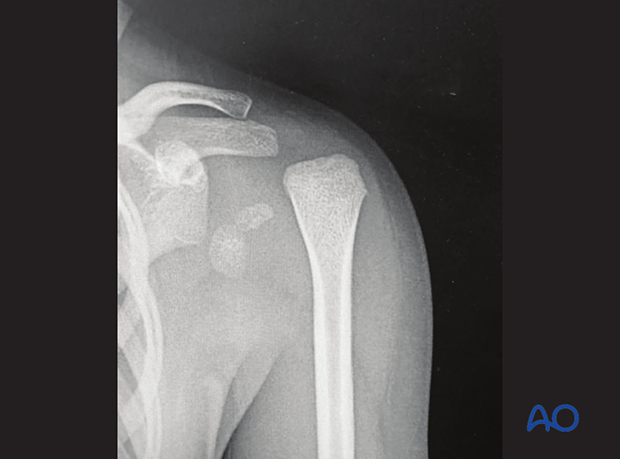
Imaging
Radiographs of Salter-Harris type-I fracture in infants do not demonstrate the fracture directly because the epiphysis is not ossified.
The x-ray may suggest a shoulder dislocation, but an ultrasound scan will demonstrate displacement of the epiphysis.
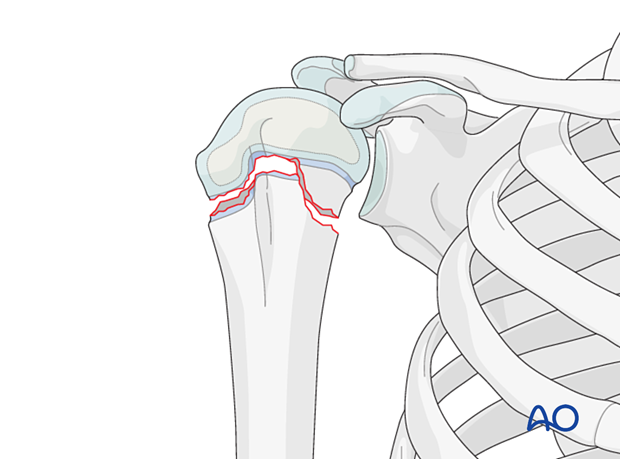
Epiphysiolysis with metaphyseal wedge (Salter-Harris II)
Salter-Harris type-II fractures are physeal injuries with metaphyseal extension. This metaphyseal component is known as the Thurstan-Holland fragment and remains attached to the epiphysis.
The Salter-Harris type-II fracture is the most common pattern of injury involving the proximal humeral physis.
Multifragmentary fractures may occur but are rare.
Imaging
AP and lateral x-rays should be obtained.
Transthoracic views should be avoided.













