Open reduction; plate fixation
1. General considerations
In Monteggia lesions two points are crucial for successful reduction of the radial head:
- Restoration of ulnar length
- Stable reduction of the radiocapitellar joint
An anatomical reduction of the ulna may not be sufficient to anatomically reduce and stabilize the radiocapitellar joint. An overcorrection of the ulna may be necessary, and this can make plating technically difficult.
2. Order of reduction and fixation
The usual strategy to deal with a Monteggia lesion is:
- Perform a stable anatomical reduction or overcorrection of the ulna.
- Assess the radial head position and stability using image intensification.
- If necessary, revise the position of the ulna.
- If necessary, perform an open reduction of the radial head.
3. Patient preparation
This procedure may be performed with the patient either in a supine position or in a lateral decubitus position.
4. Choice of approach
The ulna is exposed through a posterior approach.
If the radiocapitellar relationship is not perfect and stable, then the joint can be explored through a lateral approach.
An alternative is the posterolateral approach, which provides access to both the proximal ulna and the radial head. A disadvantage of this approach is the potential for cross-union.
5. Reduction and fixation of the ulnar fracture
Reduction of the ulna
The alignment of the ulna is addressed first.
The ulna needs to be fully out to length and stable. If this is not achieved the radial head can redislocate or sublux leading to permanent loss of forearm function.
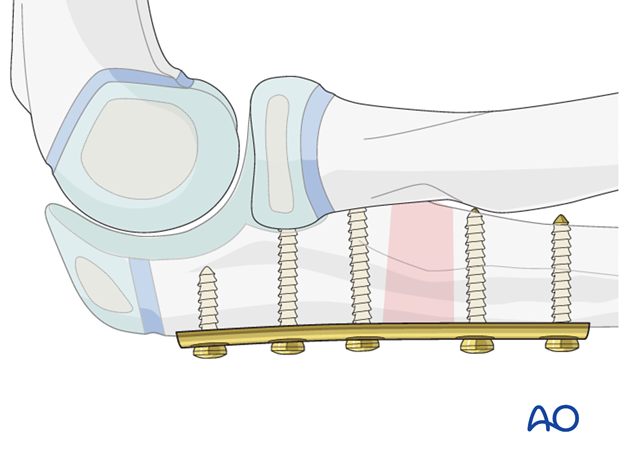
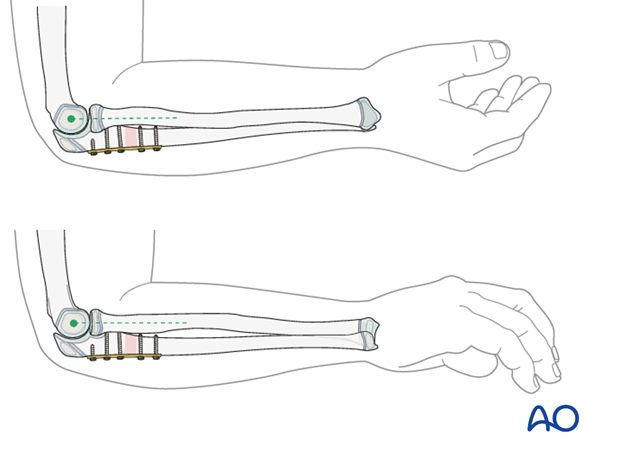
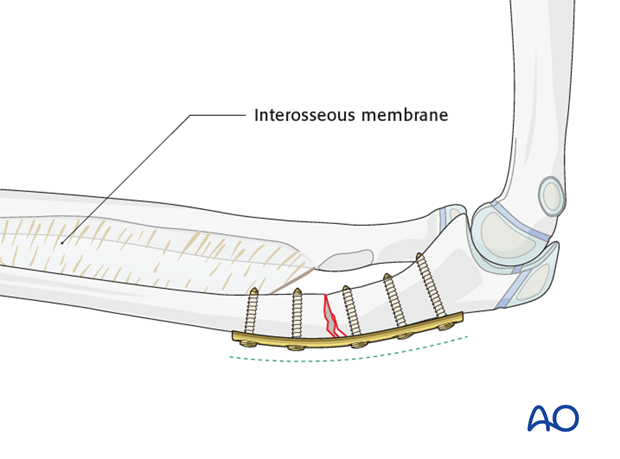
Prebending the plate for a Monteggia lesion
A plate can be contoured to overcorrect the proximal ulna and improve the stability of the radiocapitellar joint.
The overcorrected ulnar shaft will hold the radius reduced through tension in the interosseous membrane.
This may result in greater stability of the radiocapitellar joint than with an anatomically reduced ulna.
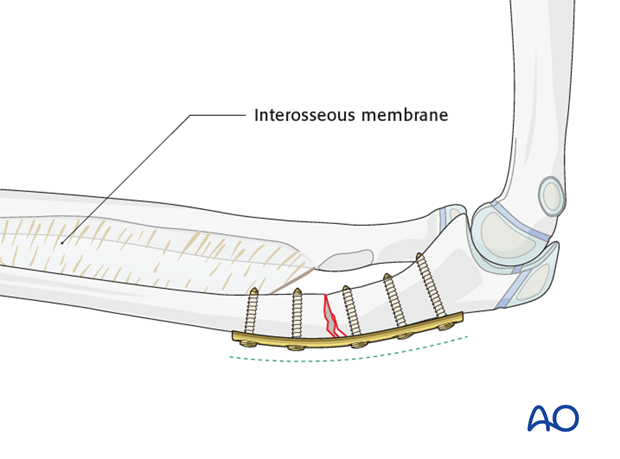
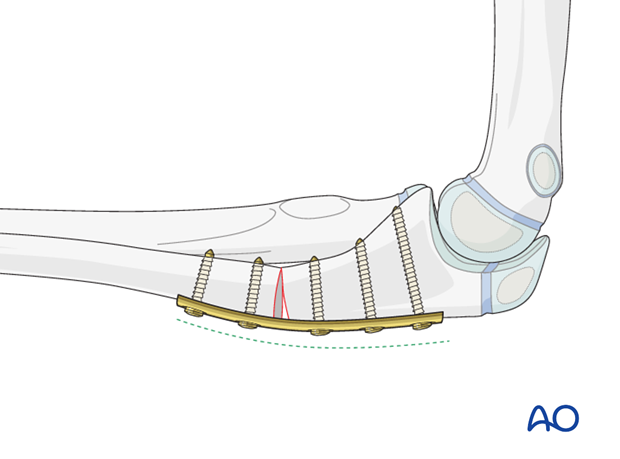
Ulnar osteotomy for plastic deformity
There is a strong tendency for the radial head to redislocate in a Monteggia lesion with plastic deformity of the ulna as the ulna rebounds to the original position.
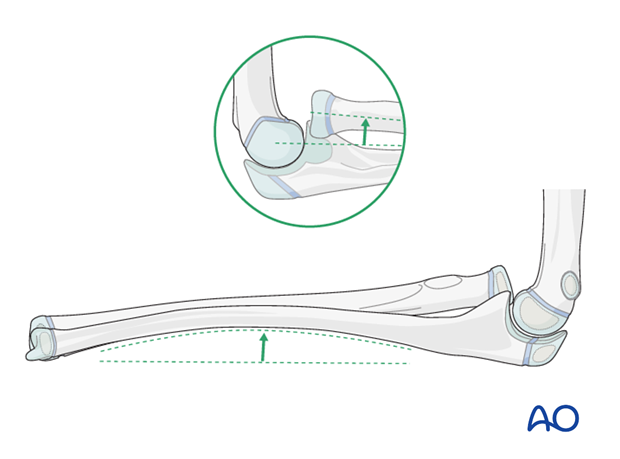
An osteotomy of the proximal ulnar shaft with overreduction can be held with an appropriately contoured plate.
In the illustrated example an apex dorsal angulation of the ulna prevents anterior redislocation of the radial head.
6. Assessing the radial head position
Reduction of radial head
The radial head will usually reduce closed and remain stable once the ulna has been aligned.
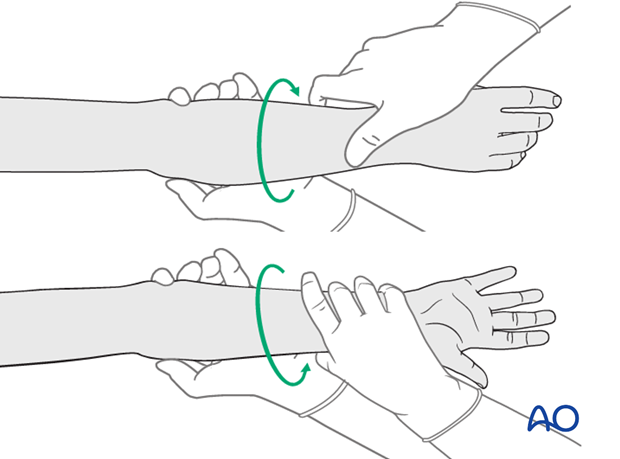
Rotation of the forearm may be necessary to complete the reduction of the radial head.
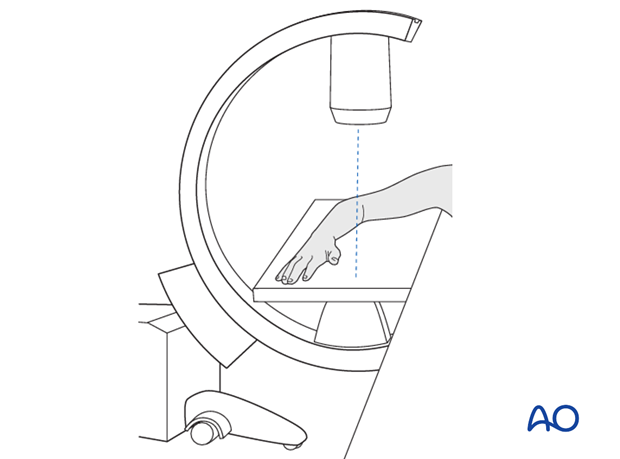
After fixation of the ulna, use an image intensifier to carefully evaluate the position of the radial head relative to the capitellum.
This must be confirmed through a full range of flexion, extension, pronation and supination.
Revision of ulnar reduction and fixation
At this stage the ulnar reduction can be revised if required, often to an overcorrected position, which usually results in stable anatomic reduction of the radial head.
If there is residual subluxation or instability in any position after optimization of the ulnar correction, there may be interposed tissue (usually annular ligament) in the radiocapitellar joint and an open reduction of this joint should be performed.
7. Open reduction of radial head
Approach to radial head
Perform a lateral approach and manually reduce the radial head.
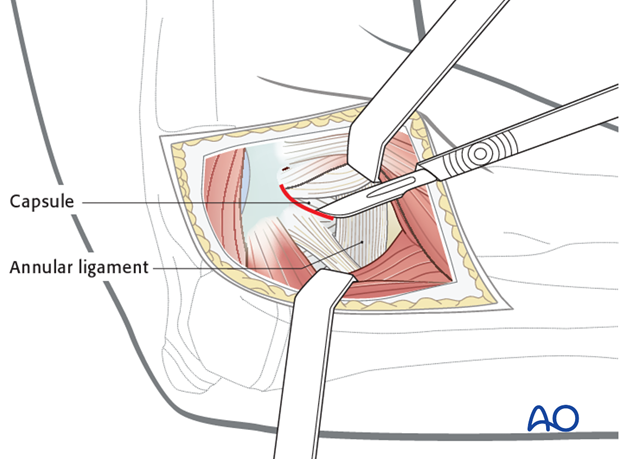
Removal of blocks to reduction
The annular ligament is the most common intraarticular block to reduction. In rare cases the ligament can be gently repositioned around the radial head.
More often the ligament must be incised or excised to allow reduction of the radial head.
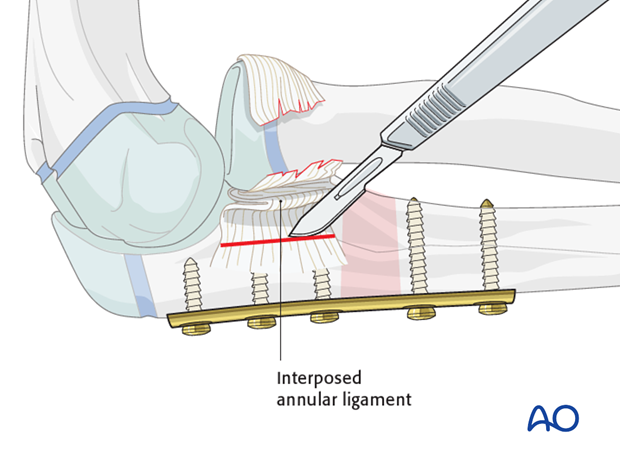
Reassessment of radial head position
Reassess the position and stability of the radial head by direct visual inspection and image intensification.
8. Final assessment
Check the completed osteosynthesis with image intensification. These images should be retained for documentation.
If an image intensifier is not available an x-ray should be obtained before discharge.
Make sure that the plate is at the correct location, the screws are of appropriate length, the desired reduction has been achieved and the radial head remains in the appropriate position.
Check the forearm rotation.
9. Aftercare following plating
Immediate postoperative care
Whilst the child remains in bed, the elbow and forearm should be elevated on pillows to reduce swelling and pain.

Cast or splint immobilization
Plate fixation of proximal ulnar fractures is intrinsically stable and supplementary casting or splinting is therefore not required, unless there are specific patient factors.
For Monteggia lesions treated with ulnar plating, the forearm may be immobilized in a cast in the position of maximum stability of the radial head for 2-4 weeks.
Analgesia
Ibuprofen and paracetamol should be administered regularly during the first 24-48 hours after surgery, with opiate analgesia for breakthrough pain.
Opiates should not be necessary after 48 hours and regular ibuprofen and paracetamol should be sufficient until 4-5 days after injury or surgery.
The child should be examined if the level of pain is increasing or prolonged analgesia is needed.
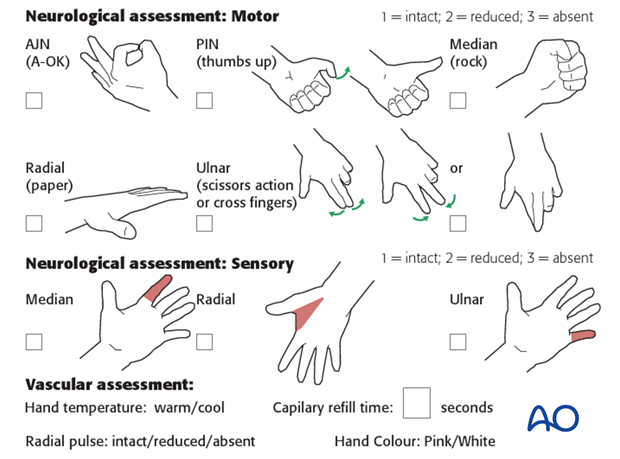
Neurovascular examination
The child should be examined regularly, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Compartment syndrome should be considered in the presence of increasing pain, especially pain on passive stretching of muscles, decreasing range of active finger motion or deteriorating neurovascular signs, which is a late phenomenon.
See also the additional material on complications and postoperative infections.
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The presence of full passive or active finger extension, without discomfort, excludes muscle compartment ischemia.
If there are signs of a compartment syndrome:
- Remove or split constrictive dressings or casts.
- Elevate the limb.
- Encourage active finger movement.
- Reexamine the child after 30 min.
If a definitive diagnosis of compartment syndrome is made, then a fasciotomy should be performed without delay.

Discharge care
Discharge from hospital follows local practice and is usually possible after 1-3 days.
The parent/carer should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger movement.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
The arm can be placed in a sling for a few days until the patient is pain free. Many children are more comfortable without support.
Mobilization
Early movement of the elbow and forearm should be encouraged as soon as the patient is pain free.
Formal physiotherapy is normally not indicated, but children should have a sheet of exercises to stimulate mobilization. See also the additional material on elbow stiffness.
Follow-up
The first clinical and radiological follow-up is usually undertaken 2-3 weeks postoperatively.
At this point, the child should be able to move the elbow with only slight restriction.
AP and lateral x-rays are required.
See also the additional material on complications and healing times.
Plate removal
Plate removal is delayed until function has fully recovered and can be performed as a day case, under general anesthesia.
Incise or excise the old scar. Incise the bursal tissue and remove the screws and plate. Close the wound in layers.













