Open reduction; plate fixation
1. General considerations
Pediatric considerations
Bridge plating is used primarily for comminuted olecranon fractures. These fractures often involve a high energy mechanism in brittle metaphyseal bone.
They are rarely seen in pediatric practice and almost always in adolescent patients at or nearing skeletal maturity.
In this case periarticular plates designed for adult patients are often suitable. The residual growth from the olecranon apophysis is minimal and can be ignored.
Children who are too small for such a plate may be treated with a modified 1/3 tubular plate cut and bent into a hook plate configuration.
Every effort should be directed at anatomical reduction and stable fixation of the major articular surface fragments, particularly the coronoid process.
In this situation, the fracture must be bridged without compression to preserve the size and shape of the olecranon fossa. Small interfragmentary screws or K-wires may be used to improve stability of larger fragments.
Bridge plating
In multifragmentary fractures of the olecranon, anatomical reconstruction of the articular surface is the primary goal. Intermediate, nonarticular fragments do not need to be reduced anatomically.
Directly manipulate only the articular fragments. Excessive manipulation of intermediate fragments risks disturbing their blood supply. If the soft-tissue attachments are preserved, and the fragments are relatively well aligned, healing is predictable. Alignment of the main fragments can usually be achieved indirectly using traction and soft-tissue tension.
Mechanical stability, provided by the bridging plate, is adequate for indirect healing (callus formation).
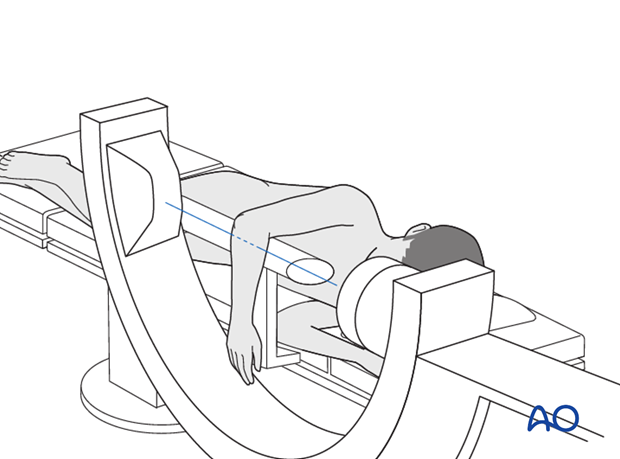
2. Patient preparation
This procedure may be performed with the patient either in a prone position or in a lateral decubitus position.
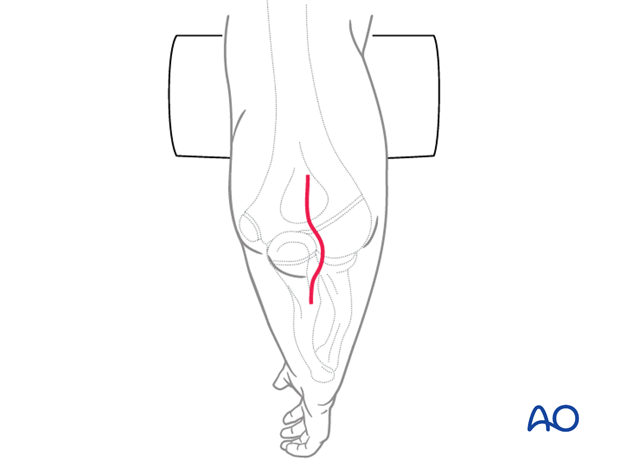
3. Choice of approach
The ulna is exposed through a posterior approach.
An alternative is the posterolateral approach, which provides access to both the proximal ulna and the radial head. A disadvantage of this approach is the potential for cross-union.
4. Reduction
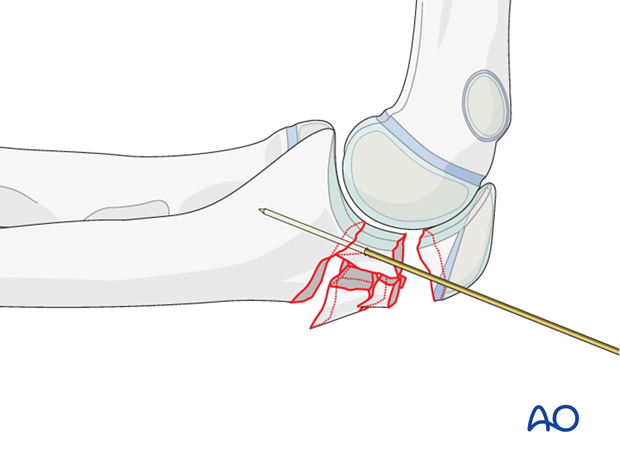
Reduction of articular fragments
Through a posterior incision, release the joint capsule medially and laterally at the fracture site. If necessary, identify and protect the ulnar nerve. With direct visualization, manipulate and anatomically reduce the articular fragments. Use the distal humerus as a template for reduction. Provisionally fix the fragments with 1.0 mm K-wires.
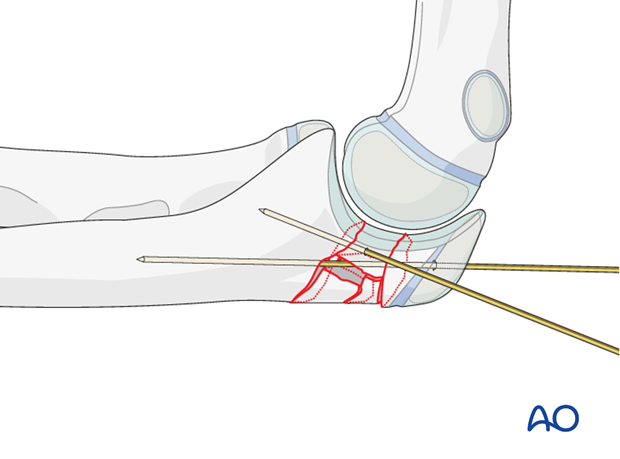
Reduction of proximal segment
Reduce the proximal part of the olecranon with pointed reduction forceps and temporarily hold the reduction with one or two K-wires.
Insert all K-wires in a position where they do not interfere with the planned plate and screws.
Check reduction with direct visualization of the sigmoid notch and the posterior cortex of the olecranon and confirm with image intensifier.
5. Plate preparation
Implant choice
An adult sized periarticular plate of any design will fit most adolescent elbows. Some of these systems have a left and right side specific to the anatomy. Small diameter 2.7 locking screws with flexible configuration are useful for comminuted fractures.
For smaller children cut a 1/3 tubular plate and fashion it into a hook plate.
Choose the length of the plate so that at least three screws may be inserted in the most proximal fragment and three in the diaphysis.
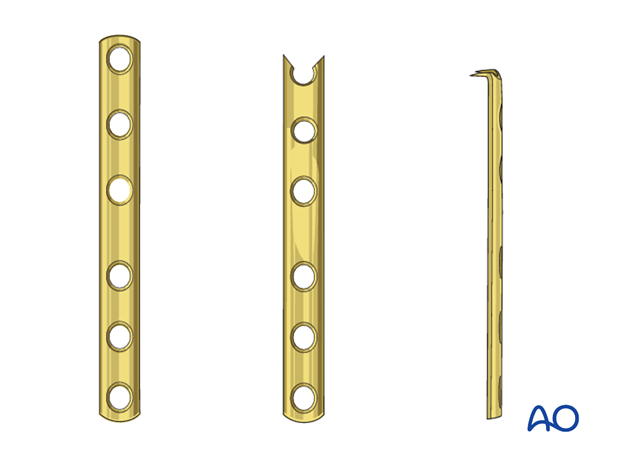
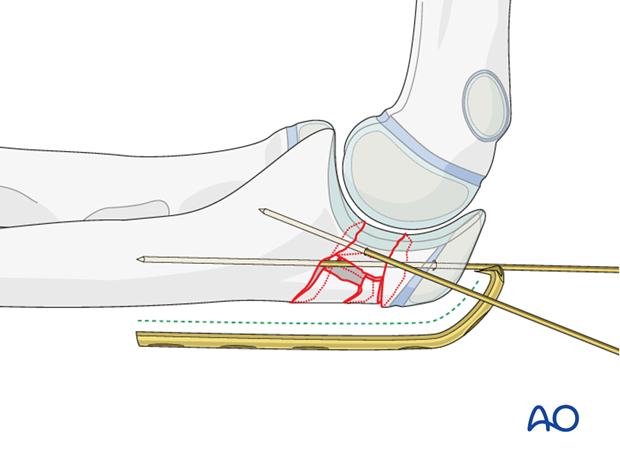
Plate contouring
If an anatomic plate is not used, contour the plate to fit the proximal ulna, bending around the tip of the olecranon. Make sure to follow the curvature of the olecranon.
Contouring is done with bending irons and a bending press.
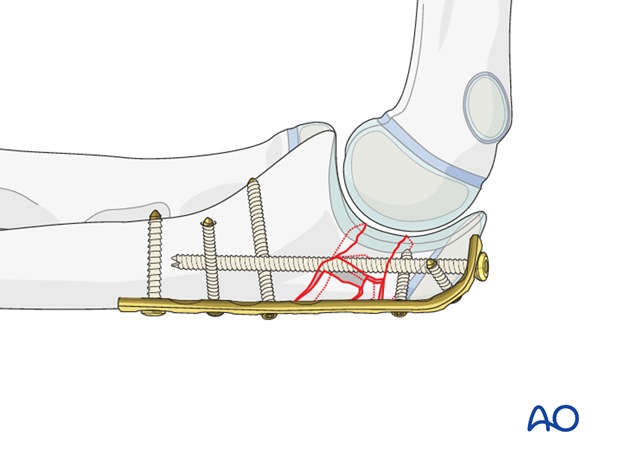
6. Plate fixation
Split of triceps attachment
To achieve close bone plate contact, split the triceps attachment before positioning the plate.
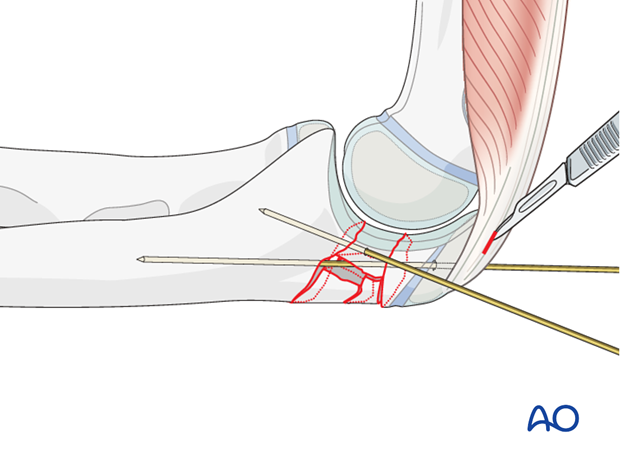
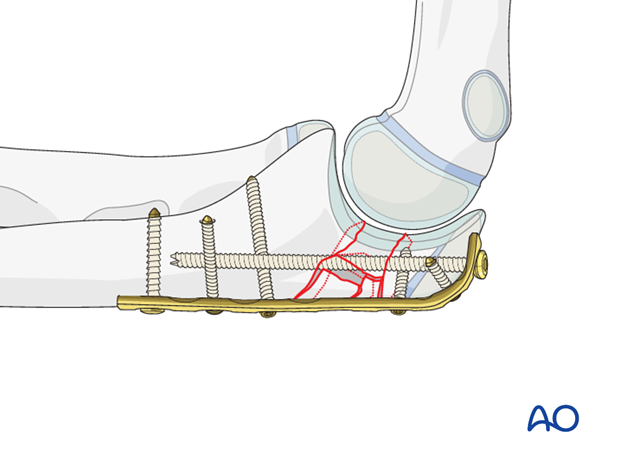
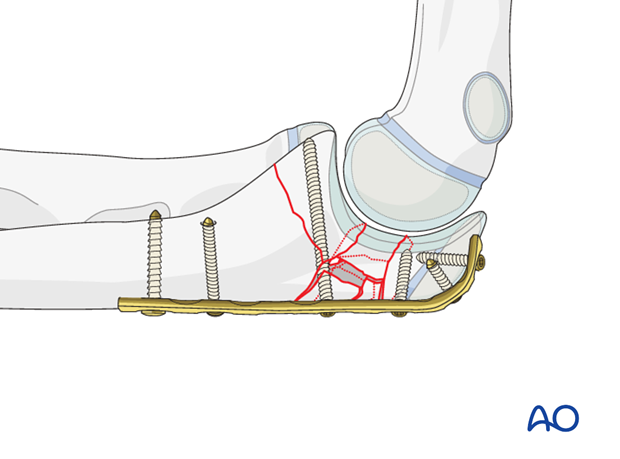
Plate placement and insertion of proximal screws
Hold the plate provisionally to the bone with K-wires and check with an image intensifier before inserting screws.
Anchor the plate with three screws to the proximal olecranon. Make sure that the screws do not protrude into the joint. A long medullary screw can add considerable stability.
Whenever possible, insert the screws bicortically, aiming the drill to the lateral or to the medial cortex.
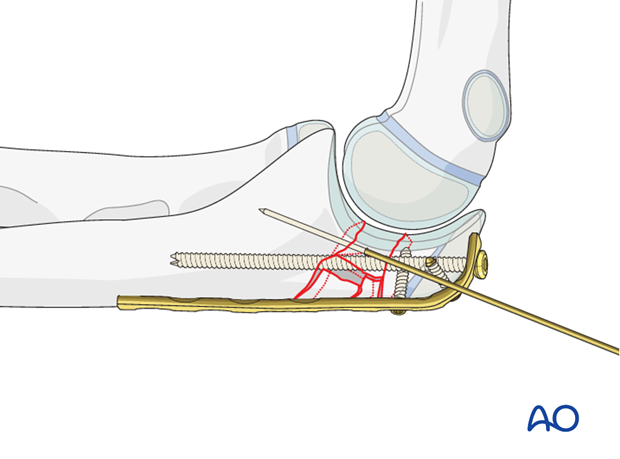
Insertion of distal screws
Insert three divergent bicortical screws into the distal fragment.
Make sure that the contour of the articular surface of the olecranon is maintained
Remove the K-wires.
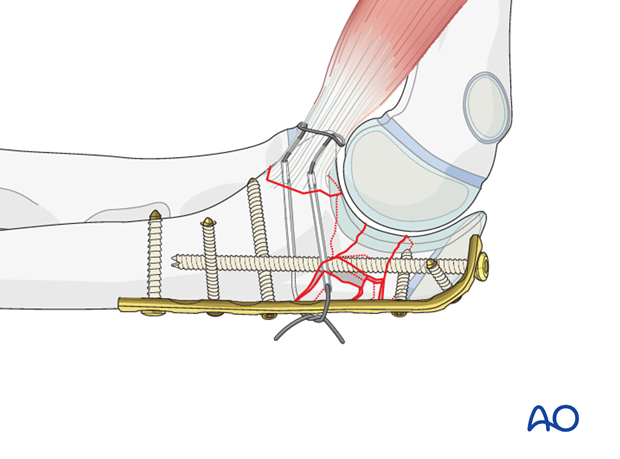
7. Fixation of a coronoid fragment
Reduction of a large coronoid fragment of multifragmentary proximal ulnar fractures may often be performed through the fracture site. Provisional or definitive fixation may be implemented at that time, but sometimes it helps to use a screw through a posterior plate for its fixation, as shown here.
Insert this as a lag screw, as perpendicular as possible to the fracture plane at the base of the coronoid. Smaller diameter screws should be used if possible.
Stabilize a coronoid fragment that is too small for screw fixation with sutures.
8. Final assessment
Take AP and lateral views.
Confirm that there is no screw penetration into the joint.
Examine for full pronation/supination and for construct stability through flexion/extension.
9. Aftercare following plating
Immediate postoperative care
Whilst the child remains in bed, the elbow and forearm should be elevated on pillows to reduce swelling and pain.

Cast or splint immobilization
Plate fixation of proximal ulnar fractures is intrinsically stable and supplementary casting or splinting is therefore not required, unless there are specific patient factors.
Analgesia
Ibuprofen and paracetamol should be administered regularly during the first 24-48 hours after surgery, with opiate analgesia for breakthrough pain.
Opiates should not be necessary after 48 hours and regular ibuprofen and paracetamol should be sufficient until 4-5 days after injury or surgery.
The child should be examined if the level of pain is increasing or prolonged analgesia is needed.
Neurovascular examination
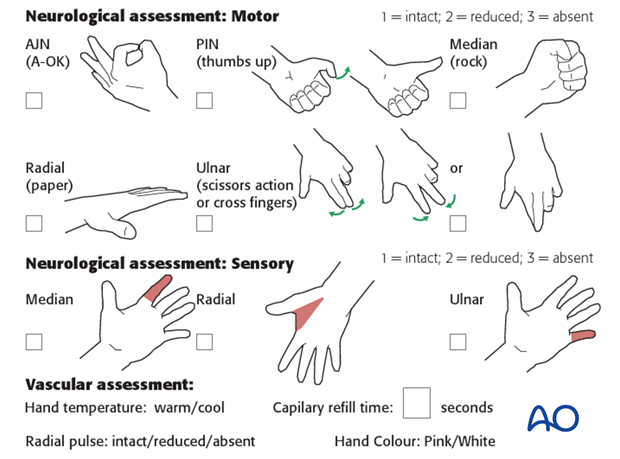
The child should be examined regularly, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Compartment syndrome should be considered in the presence of increasing pain, especially pain on passive stretching of muscles, decreasing range of active finger motion or deteriorating neurovascular signs, which is a late phenomenon.
See also the additional material on complications and postoperative infections.
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The presence of full passive or active finger extension, without discomfort, excludes muscle compartment ischemia.
If there are signs of a compartment syndrome:
- Remove or split constrictive dressings or casts.
- Elevate the limb.
- Encourage active finger movement.
- Reexamine the child after 30 min.
If a definitive diagnosis of compartment syndrome is made, then a fasciotomy should be performed without delay.

Discharge care
Discharge from hospital follows local practice and is usually possible after 1-3 days.
The parent/carer should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger movement.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
The arm can be placed in a sling for a few days until the patient is pain free. Many children are more comfortable without support.
Mobilization
Early movement of the elbow and forearm should be encouraged as soon as the patient is pain free.
Formal physiotherapy is normally not indicated, but children should have a sheet of exercises to stimulate mobilization. See also the additional material on elbow stiffness.
Follow-up
The first clinical and radiological follow-up is usually undertaken 2-3 weeks postoperatively.
At this point, the child should be able to move the elbow with only slight restriction.
AP and lateral x-rays are required.
See also the additional material on complications and healing times.
Plate removal
Plate removal is delayed until function has fully recovered and can be performed as a day case, under general anesthesia.
Incise or excise the old scar. Incise the bursal tissue and remove the screws and plate. Close the wound in layers.













