ESIN
1. Introduction
General considerations
The ESIN method involves closed reduction and internal fixation with an elastic nail.
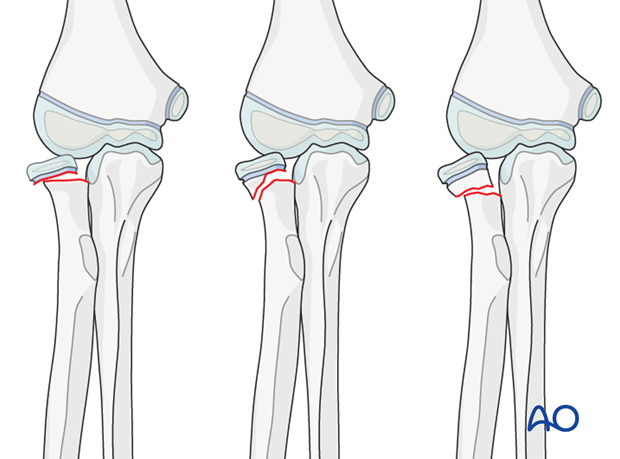
This method is a standard treatment option for all displaced radial neck fractures (p21r-E or p21r-M, types II and III).
It can be used in any age group.
ESIN without image intensifier
The ESIN method is possible without an image intensifier or perioperative x-ray examination.
The procedure is modified to include direct visualization of the fracture with an open approach. Disruption of the fracture hematoma is a disadvantage.
Note: The risk of avascular necrosis of the radial head is higher after open reduction, which should be avoided if possible.
2. Instruments and implants
Instrument set for ESIN
- 1.5-2.5 and occasionally 3.0 mm elastic nails
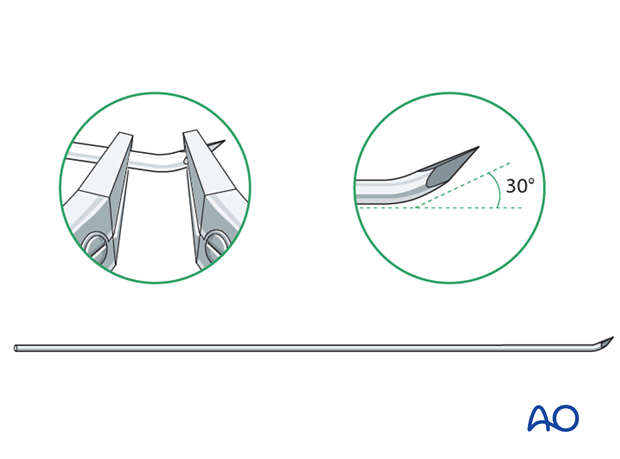
- Alternatively: 30 cm long, 1.6-2.5 mm K-wires with the tip bent
- Awl or drill
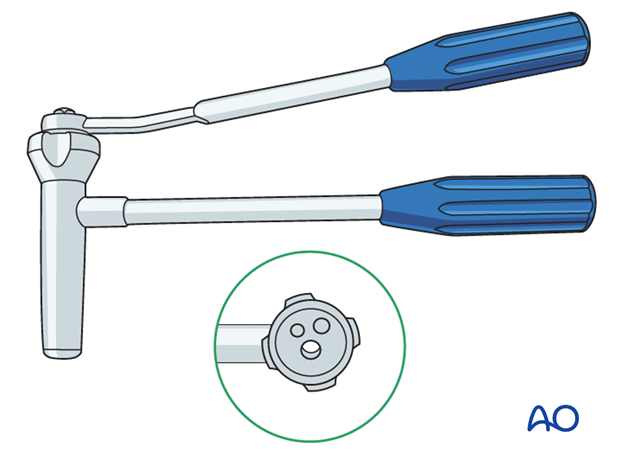
- Inserter
- Nail cutter
- Small hammer
- End caps (optional)
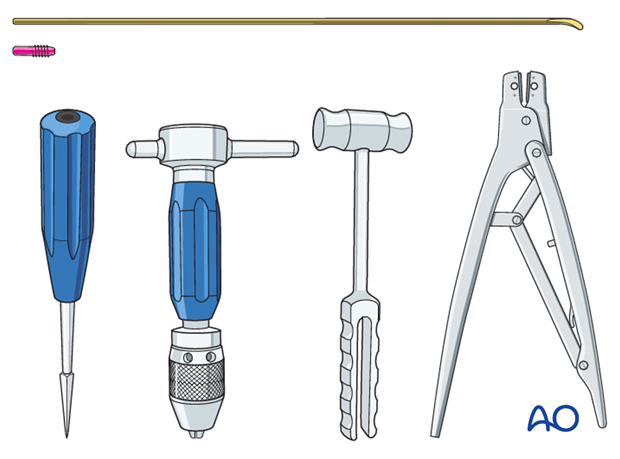
The end cutter is useful to avoid sharp ends and soft-tissue irritation.
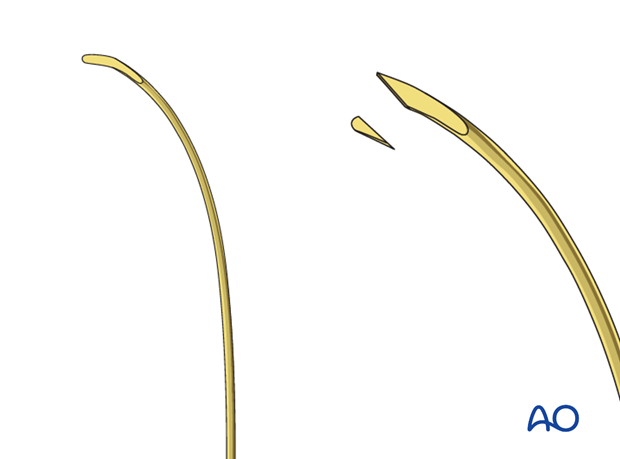
Use of K-wires
Ring fixator wires may be used.
Bend the tip by approximately 30° to provide a gliding aid.
Nail diameter
For optimal stability, the nail diameter should be between 60% and 70% of the medullary canal.
3. Patient preparation
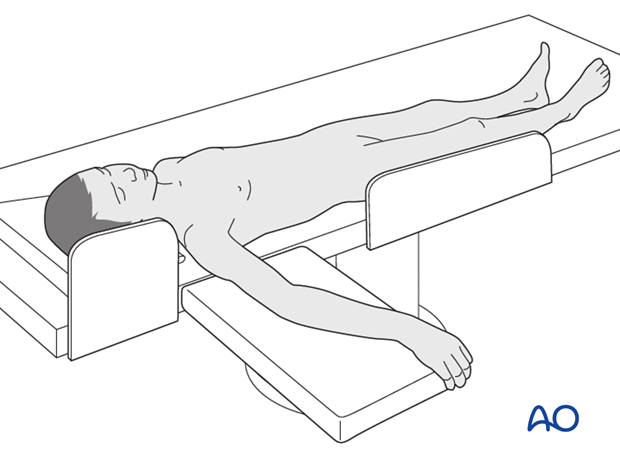
This procedure is normally performed with the patient in a supine position.
4. Entry points
The distal lateral entry point is in common use and shown in this example.
The dorsal entry point ((Lister’s tubercle)) is also well established and offers more versatile nail manipulation.
Find more details in ESIN entry points (radius).

5. Opening the canal
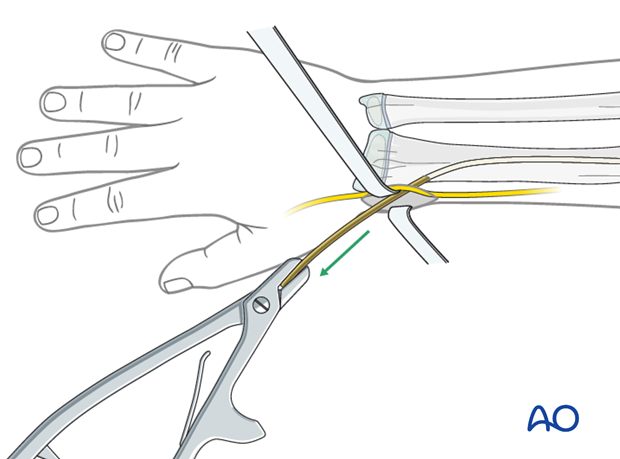
Use small scissors or a surgical clip and small retractors to dissect to the bone under direct vision.
Note: Avoid injury to the superficial radial nerve and the cephalic vein.
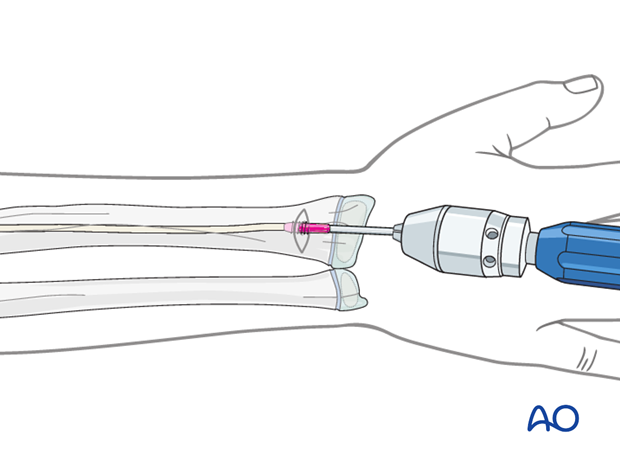
Place the awl or drill directly onto the bone and perforate the near cortex, under direct vision, perpendicular to the bone.
Do not hammer the awl to avoid perforation of the far cortex.
When the medullary canal is reached, lower the awl or drill 45° to the shaft axis and advance it with oscillating movements to produce an oblique canal.
6. Nail insertion
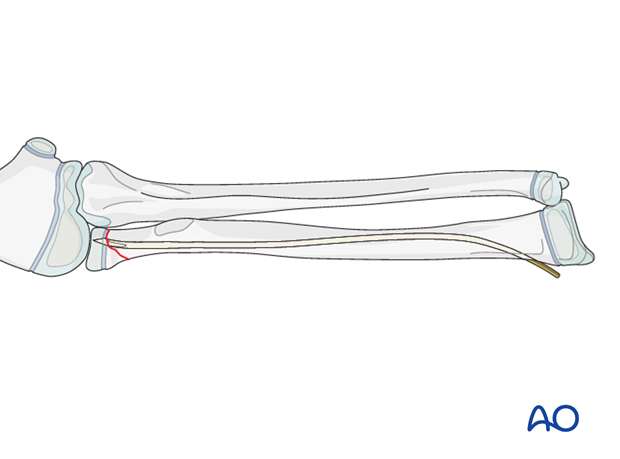
Precontour the first 5 cm of the nail as this enhances reduction of the displaced radial head.
Produce a sharp tip by cutting the inner end of the nail.
This facilitates entry into the hard bone of the epiphysis.
The manufactured blunt end will displace the radial head.
Some surgeons prefer to use a sharp K-wire with a bent tip.
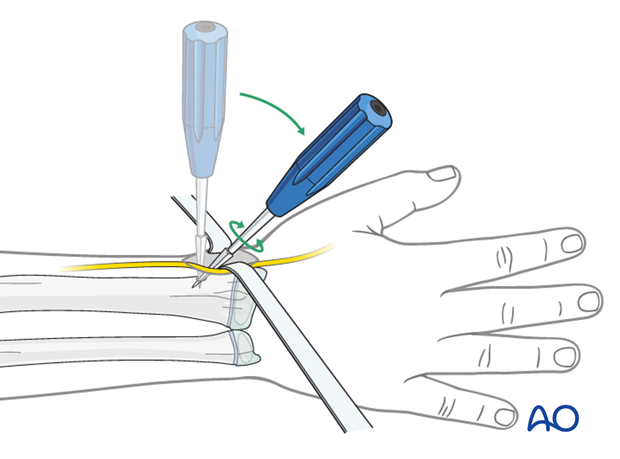
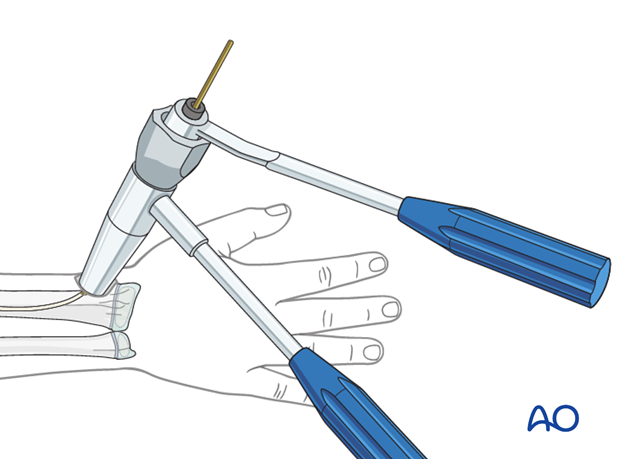
Fix the nail into the inserter and pass it into the canal.
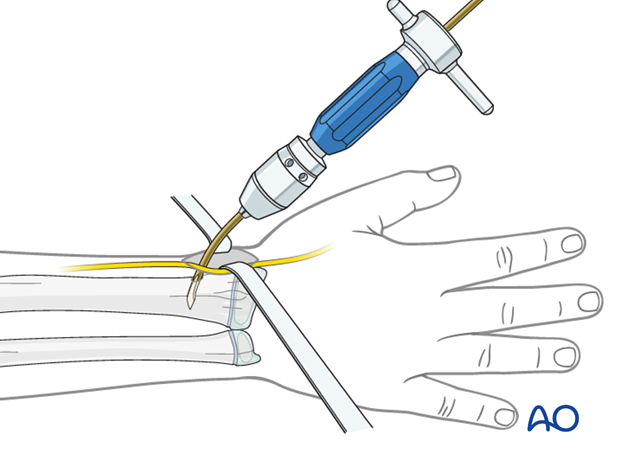
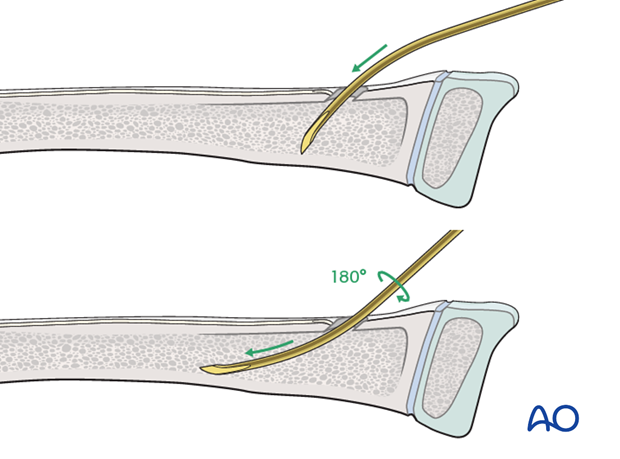
Pearl: insertion of nail tip perpendicular to shaft
Insert the nail with the tip perpendicular to the shaft axis until the far cortex is felt . Rotate the nail 180° and advance it using the curved side of the tip as a gliding aid.
If the tip is stuck in the far cortex and cannot be advanced, remove the nail and bend the tip to give a slightly more pronounced curvature.
Advance the nail to the fracture site with an oscillating maneuver.
Pearl: A short working length (3-5 cm) between the entry point and the inserter improves control of the nail during insertion.
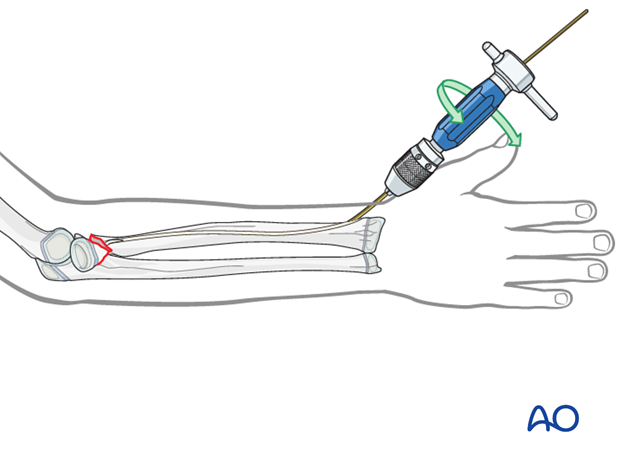
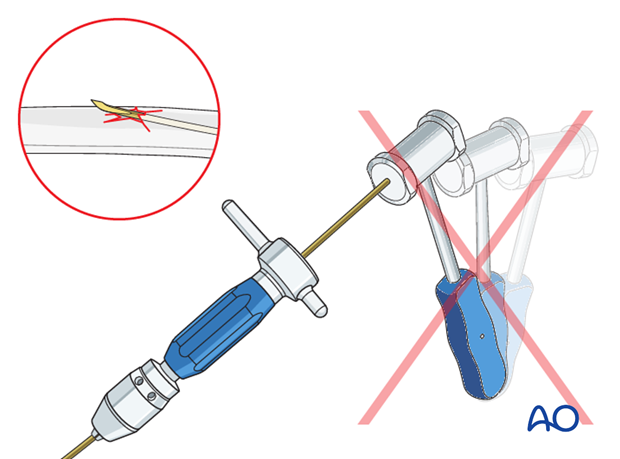
Pitfall: iatrogenic fracture
In young children, the nail tip may become stuck because of the narrow medullary canal.
Do not use a hammer if the nail is stuck as this risks iatrogenic fracture.
Withdraw by 2 cm, rotate the nail to free the tip and continue advancing.
7. Reduction
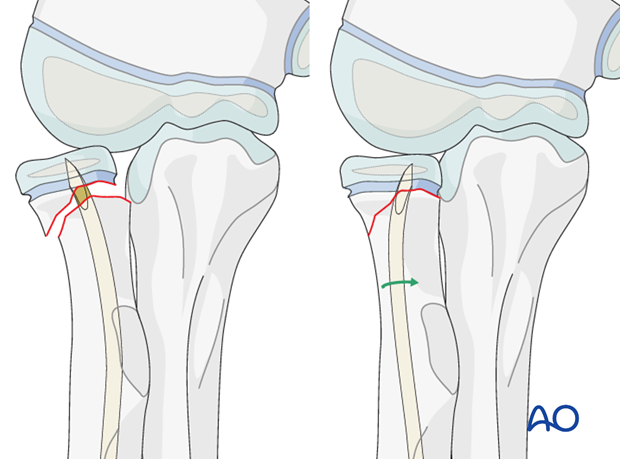
Orientation of forearm and nail
Rotate the arm to obtain the maximal displacement of the neck fracture on the image intensifier.
Point the nail tip to the head fragment.
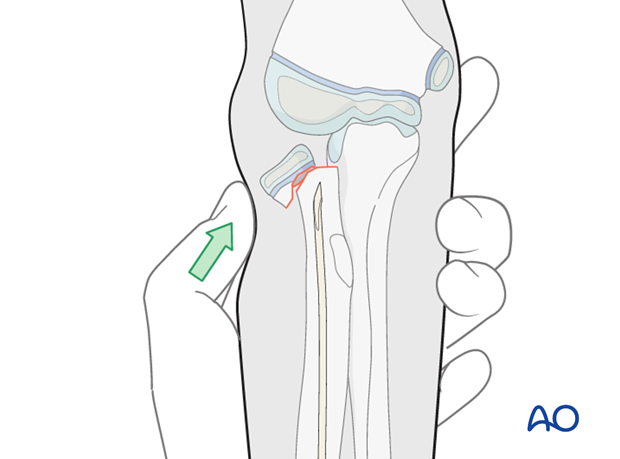
Manual reduction
If the radial head displacement does not allow the nail tip to be advanced into the head, try partial reduction of the head by traction and/or manual pressure under varus stress and/or pro- and supination.
If this is not successful remove the radial nail and recontour the first 3-4 cm with a more pronounced bend and reinsert it.
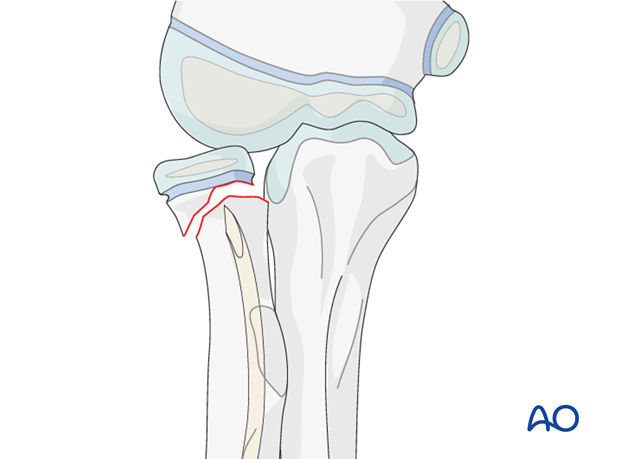
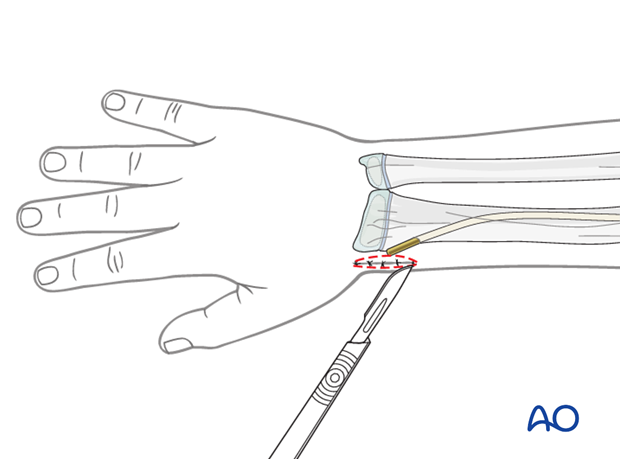
Percutaneous K-wire reduction
If manual reduction and recontouring is not successful, use the blunt end of a large percutaneous K-wire (3 mm) to push the radial head into a partially reduced position. Pushing with the sharp end or levering in the fracture may injure the blood supply.
Use a stab incision in the skin to avoid pressure necrosis.
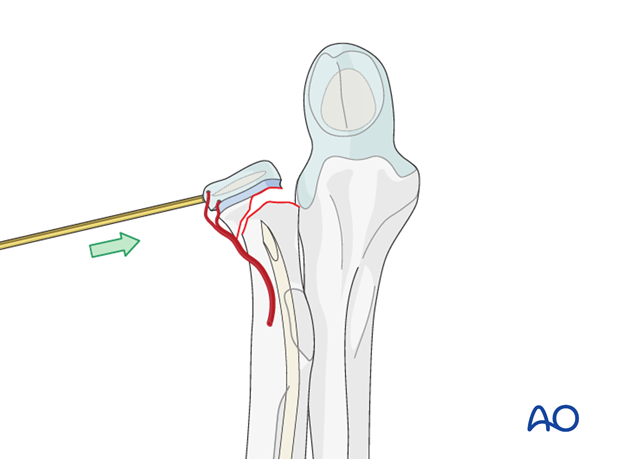
Joystick reduction
If reduction with the blunt end is not successful (eg fragment too small) insert the sharp tip carefully into the epiphysis and reduce the fragment with the K-wire as a joystick.
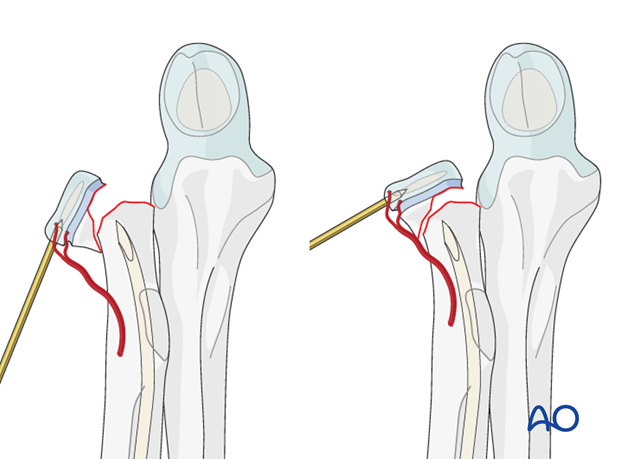
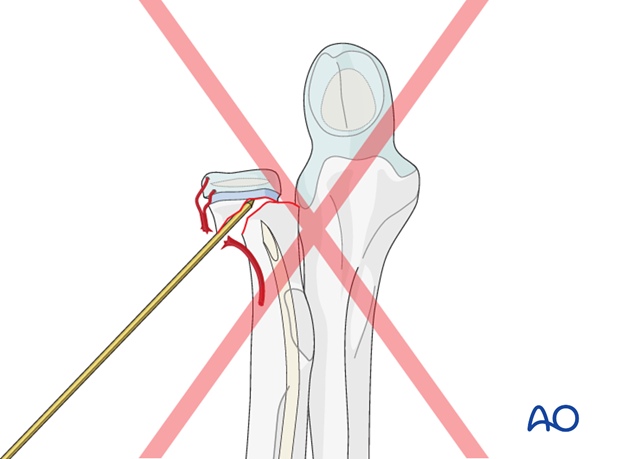
Pitfall: K-wire as lever arm
To preserve the critical blood supply do not use the K-wire as a lever arm.
Open reduction
Proceed with open reduction if:
- Radial head is grossly displaced
- Image intensifier unavailable
A direct lateral or a posterolateral approach may be used. This is associated with a high risk of disruption of the remaining blood supply.
Protect the remaining periosteum throughout the reduction maneuvers.

Pearl: minimizing additional vascular damage to the radial head
To minimize the risk of additional vascular damage to the radial head the following procedure is recommended:
1. Attempt initial reduction of the fracture through the closed capsule.
2. If unsuccessful, perform a dorsolateral arthrotomy with irrigation of the joint. The displaced radial head can usually be seen , irrespective of the direction of displacement.
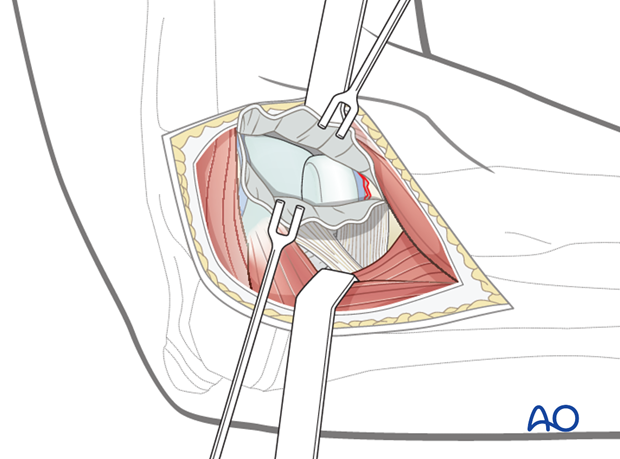
3. With a dental hook or an identical shaped K-wire push/pull the radial head to an appropriate position for final reduction with the nail.
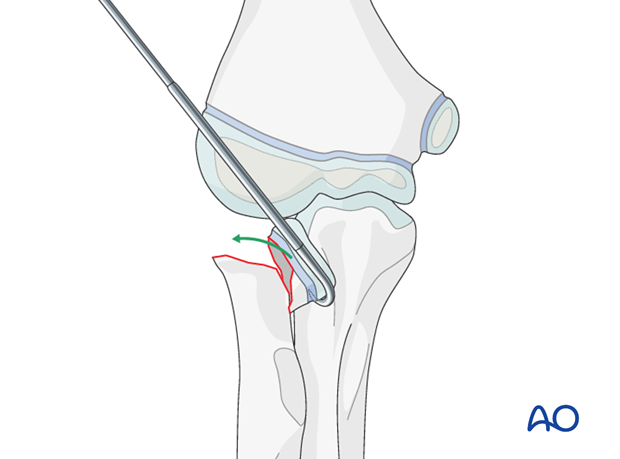
8. Fixation
Following partial reduction, advance the nail into the head.
Disimpact the head with gentle hammer blows to the nail end to free impacted annular ligament.
Turn the nail clockwise (right arm) or counterclockwise (left arm) to anatomically reduce the head.
If reduction is not anatomical, withdraw the nail tip to the metaphysis, turn it back to the initial position, advance it and repeat the reduction maneuver.
This correction should only be performed once.
Perforate the growth plate in Salter-Harris type I and II fractures to obtain sufficient hold in the head fragment. A sharpened tip is helpful to fix the nail in the final position.
In metaphyseal fractures, the tip of the nail is usually anchored in the head fragment provided the nail is of the correct length.
In very proximal metaphyseal fractures, perforate the growth plate to obtain sufficient hold.
Most of the head is unossified and not radiologically visible in young children.
If the tip of the nail is advanced just beyond the visible ossification center, it will be within the chondral tissue and not in the joint.
Pearl: If the ossification center is not visible on a normal x-ray, an arthrogram may be performed .
9. Cutting the nail and wound closure
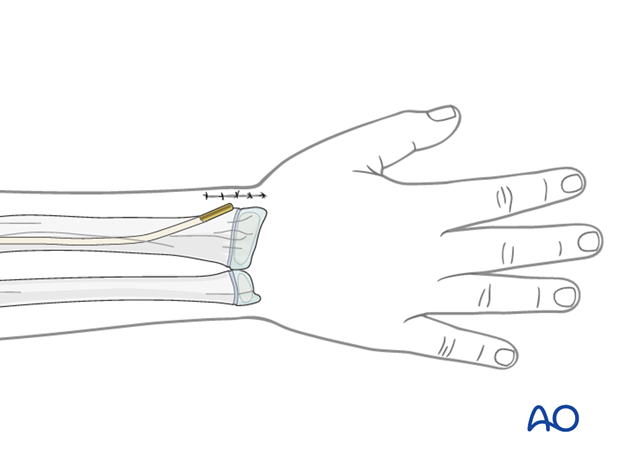
When using the lateral entry point, cut the nail near the bone.
If a dedicated nail cutter is not available, cut the nail slightly shorter as the end will be sharper and this prevents skin perforation.
Gently withdraw the nail by 1 cm.
The risk of redisplacement is low because of the pressure of the radial head on the capitellum.
Cut the nail outside the skin and reinsert to the original position with an impactor.
Ensure that the nail tip does not irritate the superficial radial nerve.
When using the dorsal entry point, the nail should be left long or protected with small end cap to prevent rupture of the extensor pollicis longus.
Close the subcutaneous tissue and skin in a standard manner.
10. Option: end caps
End caps may be useful for protection of soft tissues (eg EPL).
The nail should be advanced using the beveled impactor.
A small end cap can be inserted over the nail using the inserter.
11. Aftercare following ESIN
Immediate postoperative care
Whilst the child remains in bed, the elbow and forearm should be elevated on pillows to reduce swelling and pain.
They should be encouraged to use the arm.

Cast immobilization
Cast immobilization is not necessary and hinders early recovery of joint movement.
Analgesia
Ibuprofen and paracetamol should be administered regularly during the first 24-48 hours after surgery, with opiate analgesia for breakthrough pain.
Opiates should not be necessary after 48 hours and regular ibuprofen and paracetamol should be sufficient until 4-5 after injury or surgery.
The child should be examined if the level of pain is increasing or prolonged analgesia is needed.
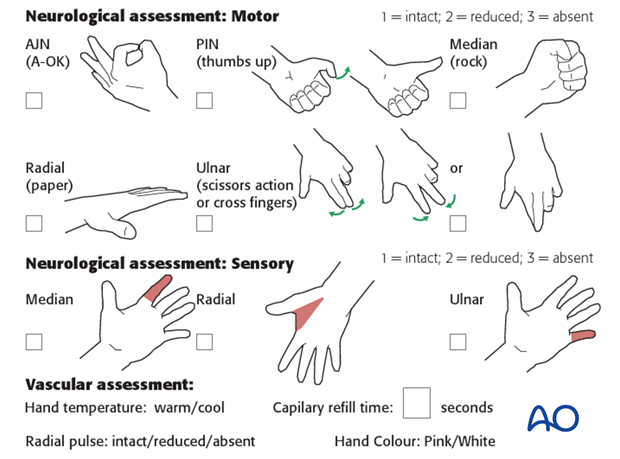
Neurovascular examination
The child should be examined regularly, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Compartment syndrome should be considered in the presence of increasing pain, especially pain on passive stretching of muscles, decreasing range of active finger motion or deteriorating neurovascular signs, which is a late phenomenon.
See also the additional material on complications and postoperative infections.
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The presence of full passive or active finger extension, without discomfort, excludes muscle compartment ischemia.
If there are signs of a compartment syndrome:
- Remove or split constrictive dressings or casts.
- Elevate the limb.
- Encourage active finger movement.
- Reexamine the child after 30 min.
If a definitive diagnosis of compartment syndrome is made, then a fasciotomy should be performed without delay.

Discharge care
Discharge from hospital follows local practice and is usually possible after 1-3 days.
The parent/carer should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger movement.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
The arm can be placed in a sling for a few days until the patient is pain free. Many children are more comfortable without support.
Mobilization
Early movement of the elbow and forearm should be encouraged as soon as the patient is pain free.
Formal physiotherapy is normally not indicated, but children should have a sheet of exercises to stimulate mobilization. See also the additional material on elbow stiffness.
Follow-up
The first clinical and radiological follow-up depends on the age of the child and is usually undertaken 4-6 weeks postoperatively.
At this point, the child should be able to move the elbow and forearm almost fully with some limited rotation caused by callus formation.
AP and lateral x-rays are required.
See also the additional material on complications and healing times.
Nail removal
Nail removal is delayed until the fracture has modelled completely and can be performed as a day case, under general anesthesia.
The nail end may slip under tendons and nerves. This may irritate the soft tissues and make it difficult to palpate the nail tip.
Exposure of the nail end should be performed under direct vision with small retractors.
In most cases, a small bursa forms over the nail tip. Once this bursa is opened, the end of the nail can be seen.
The nail can be removed with the extraction pliers, or a similar clamp. A strong needle holder is also useful.