Open reduction, headless screw fixation
1. Introduction
Preliminary remarks
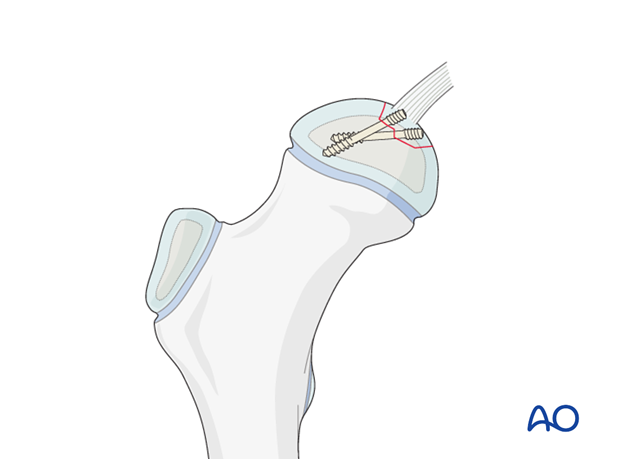
Large osteochondral fragments can be reattached with cannulated headless screws.
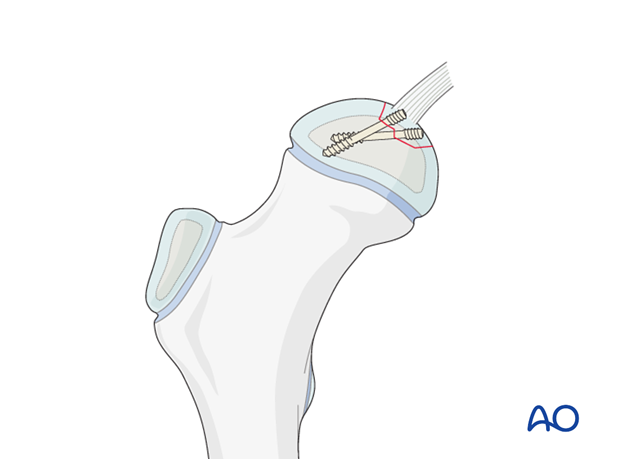
As headless screws are not resorbable, it is important that the ends of the screws are below the cartilage. The bony part of the fragment must therefore be large enough to accommodate the proximal thread of the headless screw.
Note: The osteochondral fragment can become necrotic, leading to prominence of the screw end. This is suggested by pain during movement, and mandates screw removal.
At least two divergent screws should be used to provide satisfactory fixation and some axial compression.
2. Patient preparation and approach
Patient preparation
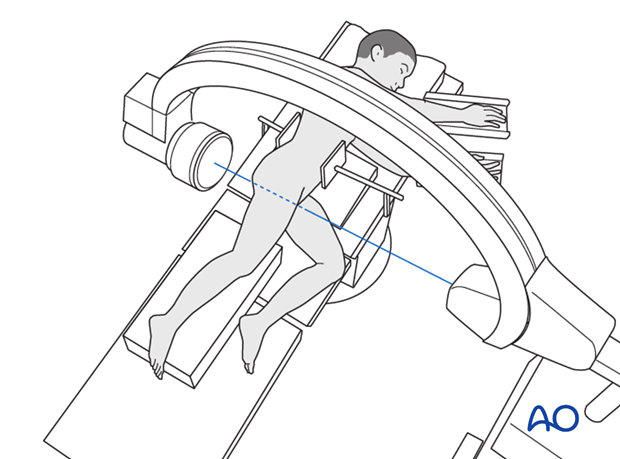
This procedure is normally performed with the patient in a lateral position.
Approach
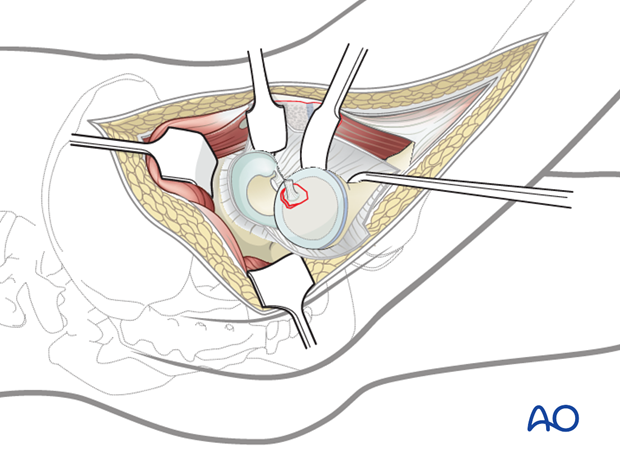
The preferred approach is via a surgical hip dislocation. This approach offers optimal assessment, reduction, and fixation.
3. Reduction
Once the femoral head is dislocated, the fragment is anatomically reduced.
If there is a delay to surgery, swelling of the cartilage of the fragment may be seen. This may need to be trimmed in order to reduce it fully.
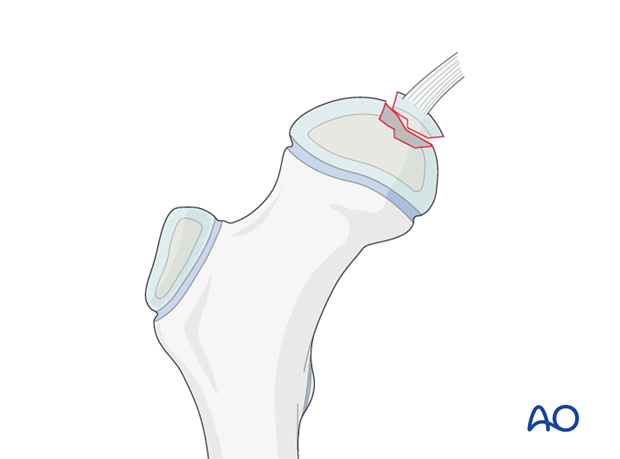
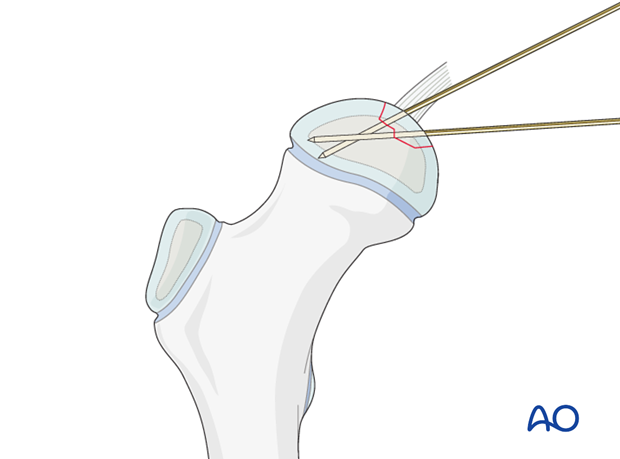
The fragment is then secured with finger pressure and two or three divergent guide wires (corresponding to the screw size) are inserted.
4. Fixation
Screw insertion
When the fragment is anatomically reduced, screws with a length of approximately 2/3 of the femoral head diameter are inserted over the guide wires.
Completely intraepiphyseal placement is preferred.
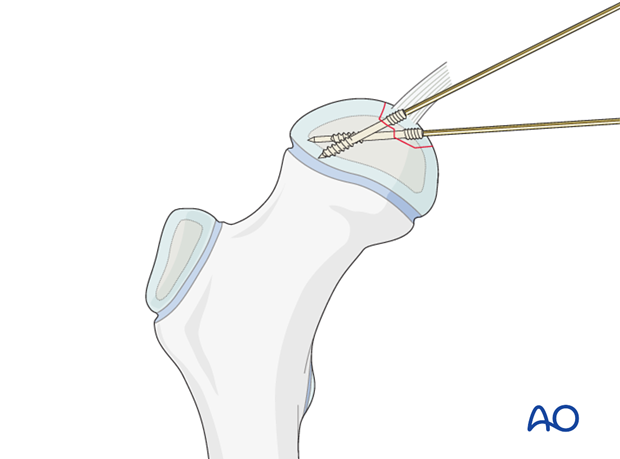
The guide wires are removed.
Hip reduction
After fixation, the hip is reduced and free movement of the head is checked without moving the fragment.
5. Aftercare
Introduction
After surgical stabilization, the construct should be sufficiently robust to allow protected weight bearing. Smaller children may not be able to comply with this and may need immobilization.

Infection
See the additional material on postoperative infection.
Range of movement
Only controlled range of motion, without forced movements, is permitted for 4-6 weeks postoperatively.
Weight bearing
Full weight bearing is permitted after wound healing.
Sports
Swimming can be allowed as soon as partial weight bearing is permitted.
Contact sports should be avoided for at least six months.
Follow-up
X-rays are generally taken immediately after the surgery and at 6 and 12 weeks.
The onset of pain and reduction in the range of motion may indicate prominence of the screws.
CT scan and dynamic arthrography are useful in assessment of screw position and stage of healing.
Implant removal
Only prominent screws must be removed.













