External fixation
1. General considerations
Modular external fixator
The versatility of a modular external fixator is an advantage in the management of children’s fractures and can accommodate age-specific variations in fracture biology and anatomy.
An external fixator may be used for definitive management of femoral fractures in younger children due to the short healing time.
Practical considerations are illustrated in detail in the basic technique for application of modular external fixator in children.
Specific considerations for the femoral shaft are given below.
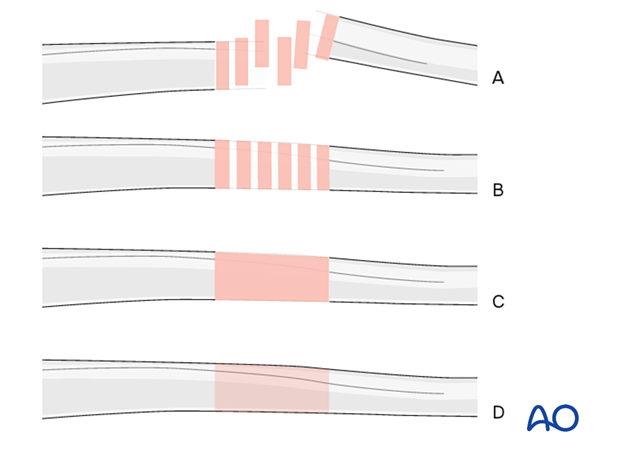
Throughout this section generic fracture patterns are illustrated as:
- Unreduced
- Reduced
- Reduced and provisionally stabilized
- Definitively stabilized
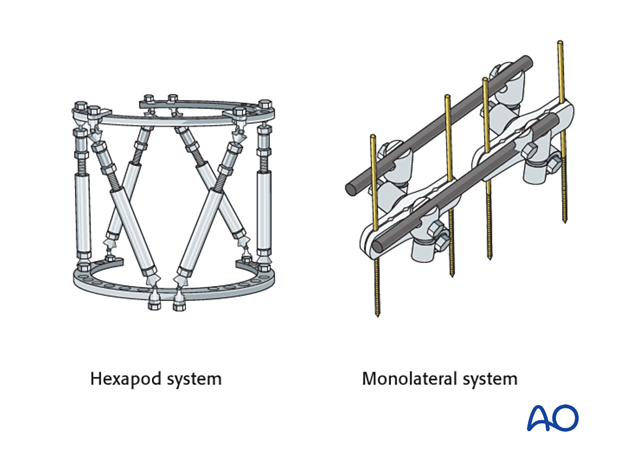
Other types of external fixator
Alternative configurations are available and include monolateral or ring systems.
Disadvantages of these systems in children include:
- Need for extensive inventory
- Excessively stiff construct
Pin size in femoral fractures
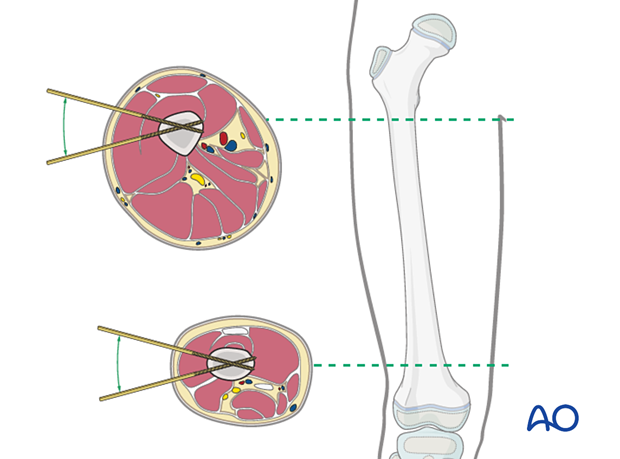
External fixation is suitable for all ages, but the pin diameter must be appropriate to the size of the bone.
Pins with a thread diameter of 3.0–6.0 mm are suitable for femoral fractures and should typically be between 1/4 and 1/3 of the external bone diameter.
2. Patient preparation and approach
Patient positioning
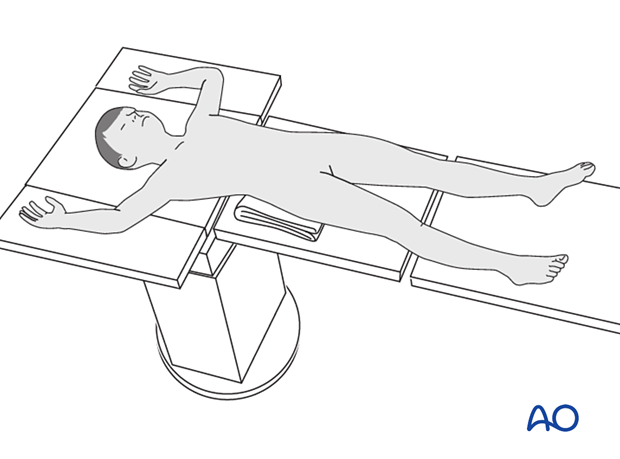
Place the patient in a supine position without traction on a radiolucent fracture table, with a bump under the ipsilateral flank.
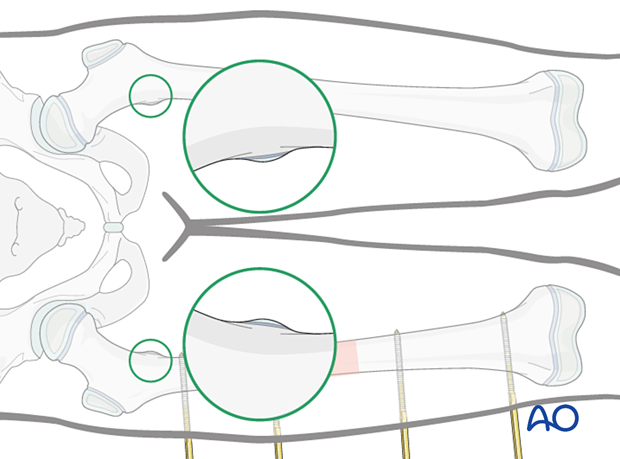
When positioning the patient check the rotational alignment of the uninjured femur.
Approaches for safe pin placement
For safe pin placement make use of the safe zones and be familiar with the anatomy of the femur.
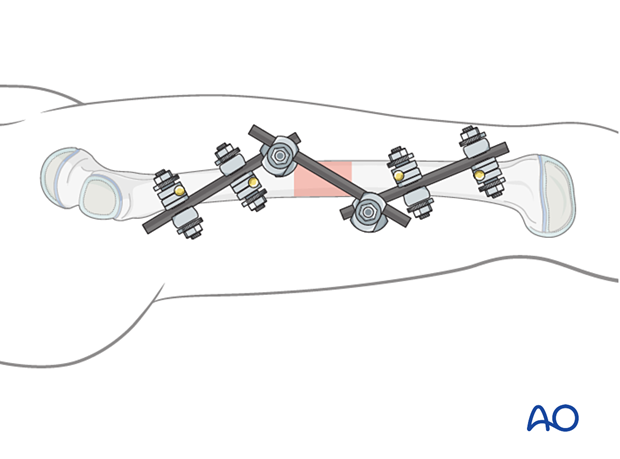
3. Frame construction
Pin insertion
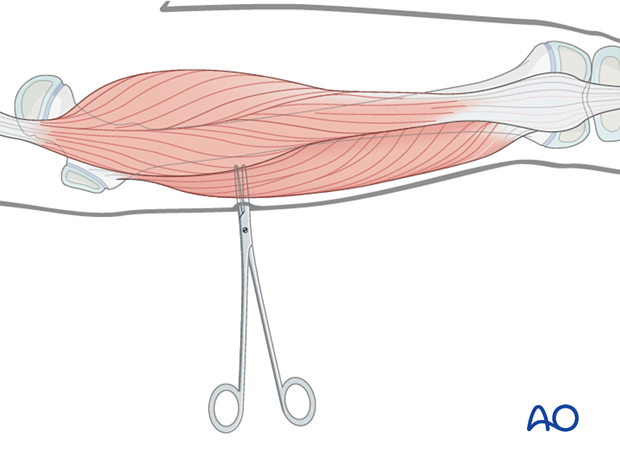
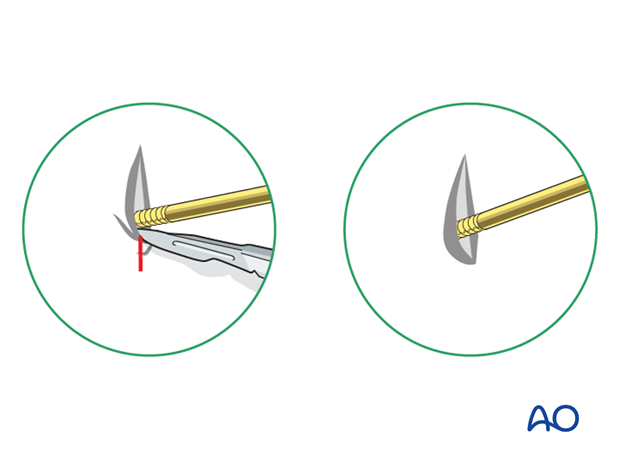
Insert the pins via a lateral incision with blunt dissection to the bone.
The exact sequence of pin placement is determined by fracture morphology and surgeon’s preference.
Make an adequate skin incision over the site of pin insertion.
Use an artery clip for blunt dissection down to the bone.
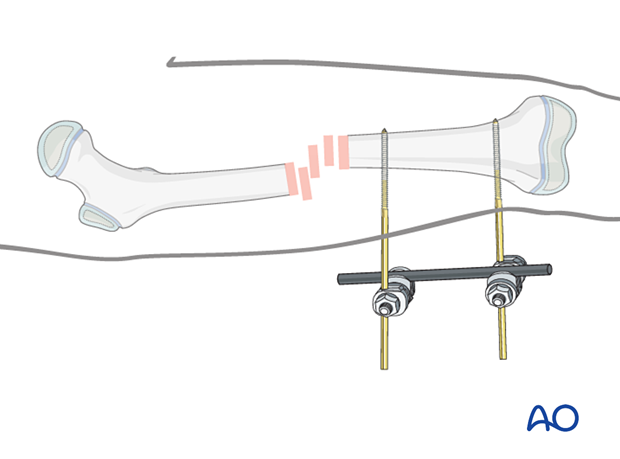
Distal frame assembly
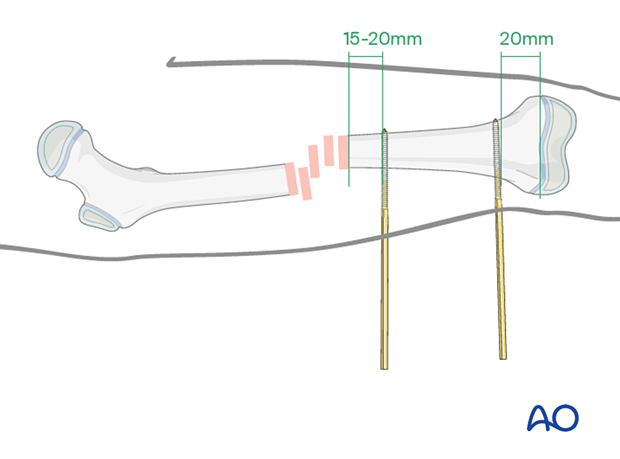
The most distal pin should be 20 mm proximal to the distal femoral growth plate.
The second pin in the distal fragment can be inserted 15–20 mm distal to the fracture site.
Attach the appropriately sized rod to the distal pins and tighten the rod-to-pin clamps.
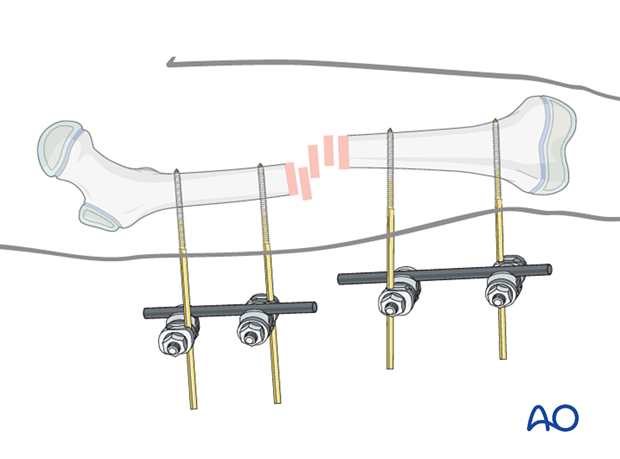
Proximal frame assembly
Insert pins in a similar fashion, typically just distal to the lesser trochanter and 15–20 mm proximal to the fracture.
Attach the appropriately sized rod to the pins and tighten the rod-to-pin clamps.
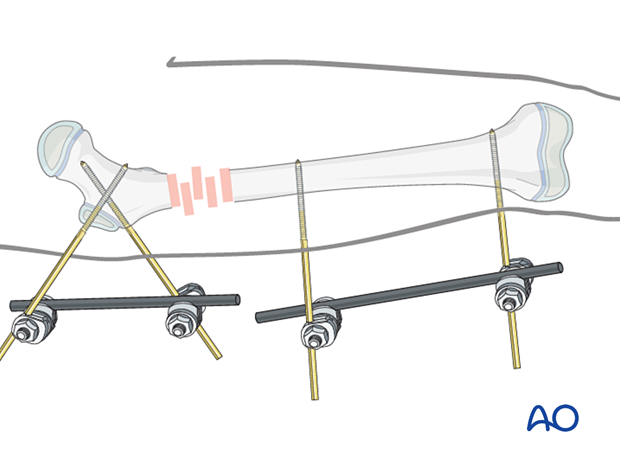
Proximal frame in very proximal fracture
For fixation of fractures in the proximal third of the femoral shaft insert the proximal pins in the proximal femoral metaphysis.
Avoid crossing the proximal femoral growth plate.
Crossing the trochanteric apophysis is usually well tolerated, particularly in older children.
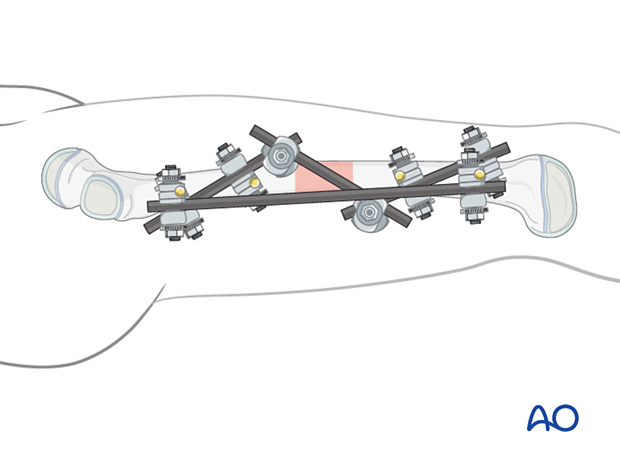
Connection of the two partial frames
Loosely apply a connecting rod to the two partial frames.
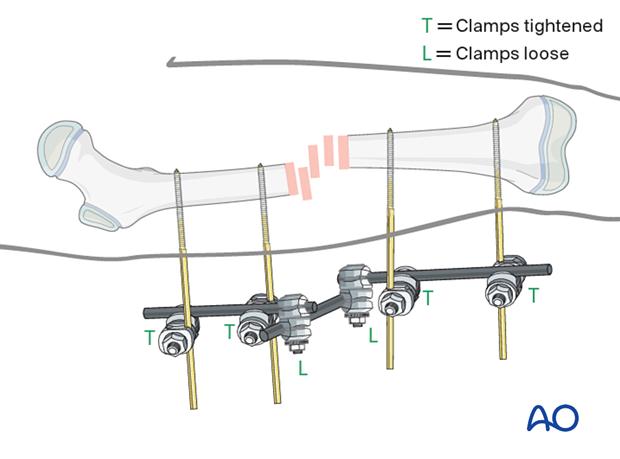
Reduction and fixation
Under image intensification manipulate the partial frames to achieve correct reduction.
Do not accept varus angulation.
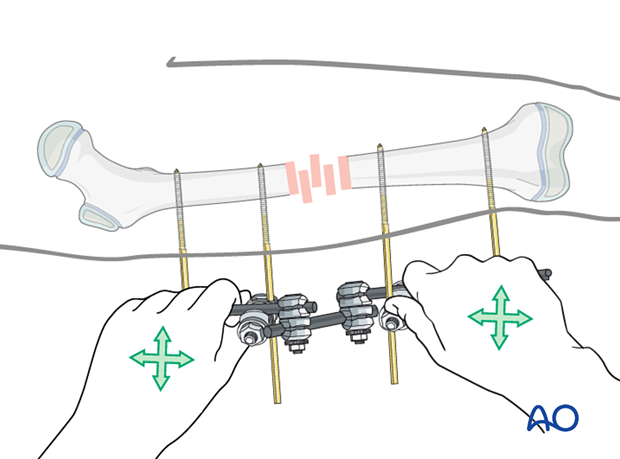
Tighten the rod-to-rod clamps.
Assessment of rotational alignment
Confirm rotational alignment of the femur clinically by comparing internal and external rotation to the contralateral side.
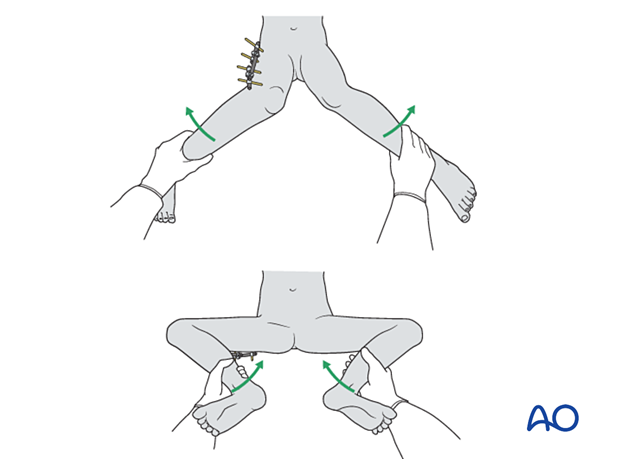
In addition to clinical examination, an intraoperative radiological assessment of rotational alignment may be useful.
For more detail see the additional material on assessment of rotation.
In this example, the knee is placed in the true AP position and the appearance of the lesser trochanter is compared with the uninjured limb.
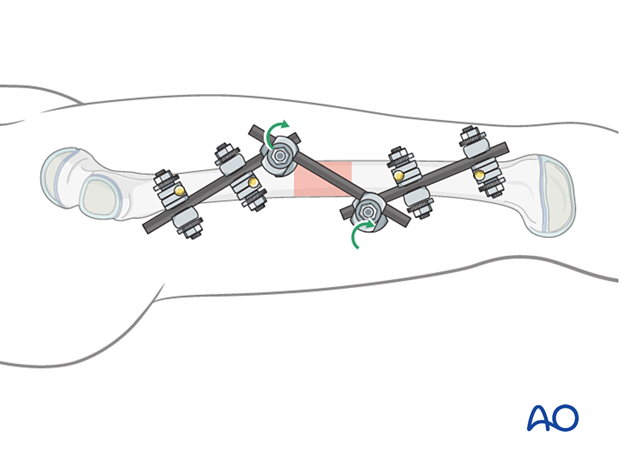
Reinforcing the frame
A second bar may be used to span the construct for additional stability. This may be placed from bar to bar or onto a pin depending on available space.
Pin sites
Check the skin at the pin sites and incise if tethered.
Fully flex the hip and knee to release tethering of vastus lateralis by the pins.
Ensure that there is sufficient space between skin and fixator to accommodate postoperative swelling.
Dress the pin sites to prevent skin motion.
4. Aftercare
Pin-site care
Pin-care protocolThere is no universally agreed protocol for pin-site care.
The following points are however recommended:
- Pin-site care should continue until removal of the external fixator.
- The pin sites should be kept clean.
- Crusts or exudates should be removed.
- The pins may be cleaned with water, saline, disinfectant solution or alcohol. The frequency of cleaning varies from daily to weekly.
- Ointments or antibiotic solutions are not recommended for routine pin-site care.
- Pin sites do not need to be protected whilst showering or bathing with clean water, but should be dried immediately.
Initial management is with oral anti-staphylococcal antibiotics.
In case of pin loosening or unresponsive pin site infection, the following steps should be taken:
- Remove all involved pins and place new pins in a healthy location.
- Debride the pin sites in the operating theater, using curettage and irrigation.
- Take specimens for microbiological culture to guide appropriate antibiotic treatment.
Internal fixation following an infected external fixator pin has a high risk of infection and should be avoided unless no reasonable alternative is available.
Mobilization
The patient should be encouraged to move the hip and knee, within the limits of comfort.
In most cases the fixator is not stable enough to allow initial weight bearing. Partial weight bearing can be resumed when callus is visible, typically at 4 weeks.
Follow-up
The patient should be seen 7–10 days after surgery for a wound check.
X-rays are taken to check stability and alignment.
Fixator removal
Fixator removal is determined by the age of the child and healing rate.
Look for mature callus bridging 3 or 4 cortices of the femur before removing the frame.
Refractures are a common complication and many surgeons recommend partial weight bearing with crutches after fixator removal to allow further strengthening of the callus.

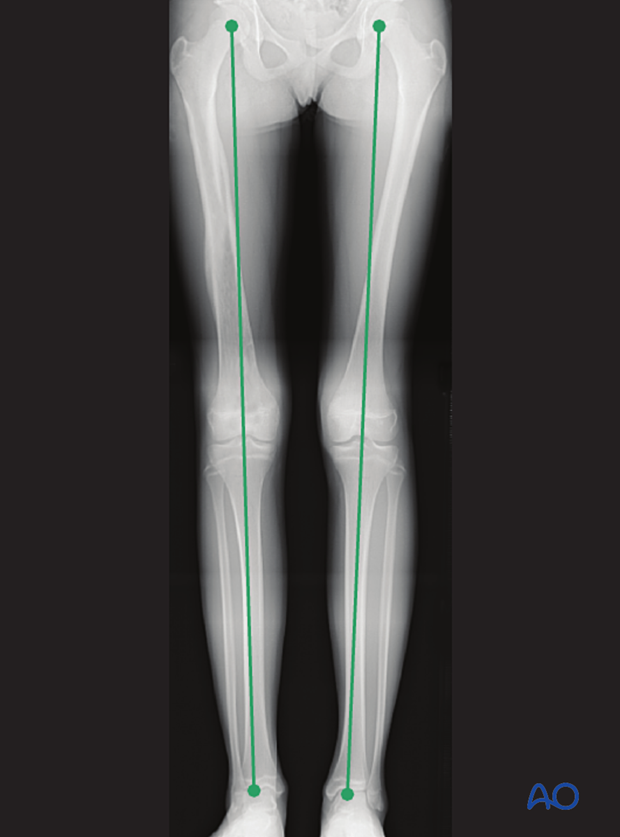
Follow-up for leg-length assessment
Clinical assessment of leg length and alignment is recommended at one-year.
Clinical assessment of leg length uses a tape measure from the ASIS to the medial malleolus.
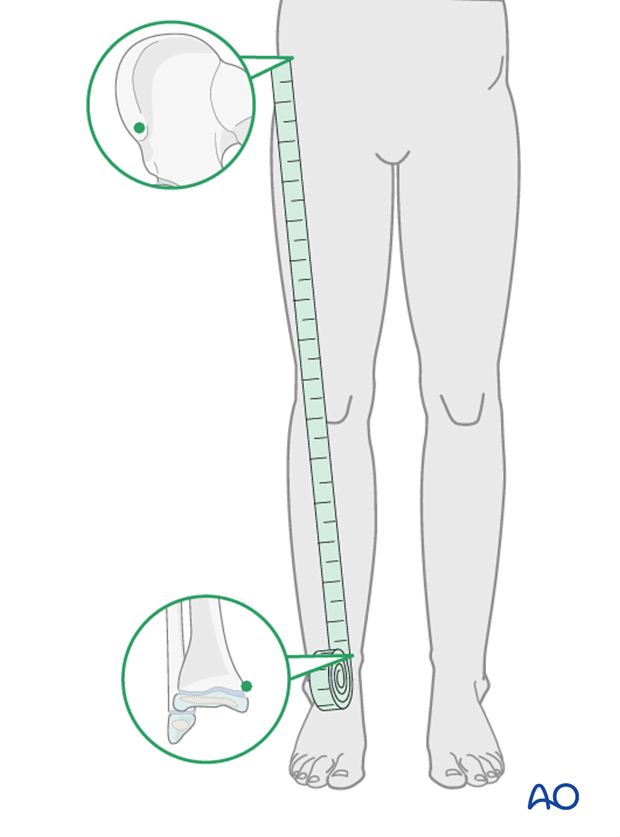
If there is any concern about leg length discrepancy or malalignment, long-leg x-rays are recommended.
Leg length is measured from the femoral head to the ankle joint.