Closed reduction; splint immobilization
1. Introduction
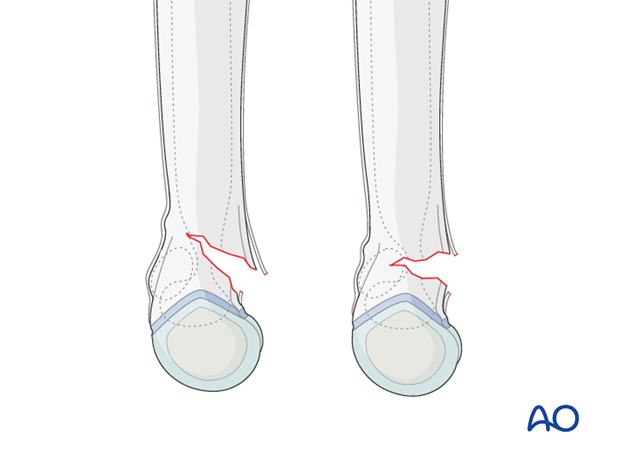
Extension type supracondylar fractures that are minimally displaced may be treated with closed manipulation and splinting.
The stability of the distal fragment cannot be ensured in a splint and loss of reduction, or incomplete reduction, leading to malunion is possible.
The best time to assess the carrying angle of the elbow is during examination and manipulation.
If the extended elbow is in an anatomical or slightly valgus position, compared with the uninjured elbow, closed reduction and splinting of minimally displaced (less than 15° of extension) 13-M/3.1 II fractures is an option.
Note: A control x-ray should be taken within 7 days to monitor for loss of reduction.
If the extended elbow appears to be in a varus position compared to the uninjured elbow, then reduction in the operating room and intraosseous pin fixation is required.
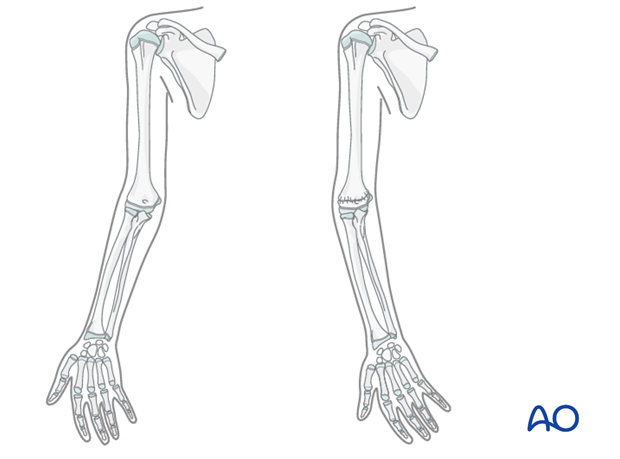
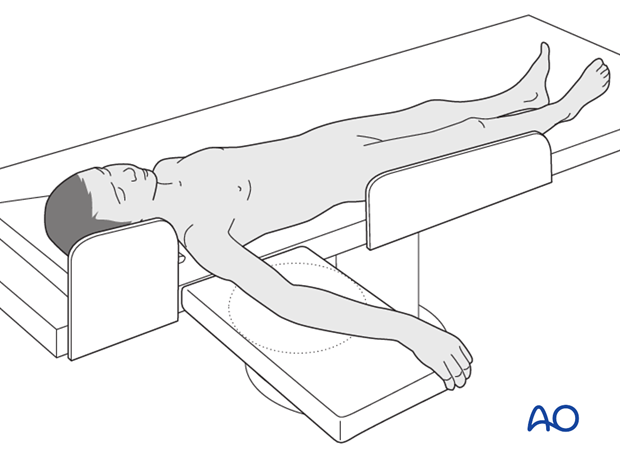
2. Patient preparation
This procedure is normally performed with the patient in a supine position.
3. Closed reduction
Correction of extension type supracondylar fractures
Any incomplete fracture which is oblique in an AP view will have a small component of varus or valgus deformity.
This will correct itself at the same time as the extension angulation and with the following maneuver.
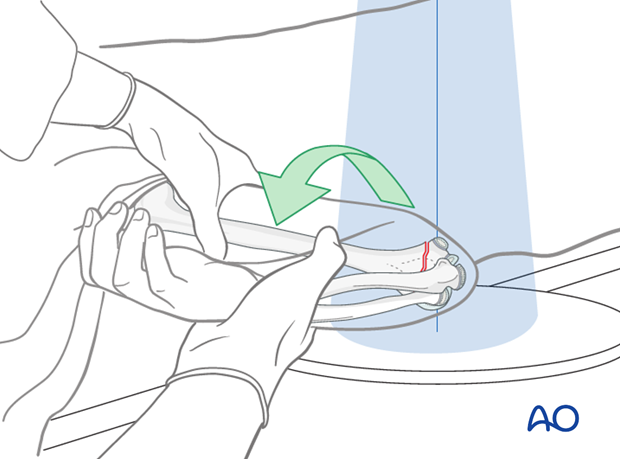
With the elbow extended, a thumb is positioned on the back of the olecranon and pushed distally and anteriorly whilst the elbow is smoothly flexed.
If the elbow will not flex fully it is likely that the reduction is incomplete. A complete reduction may be felt.
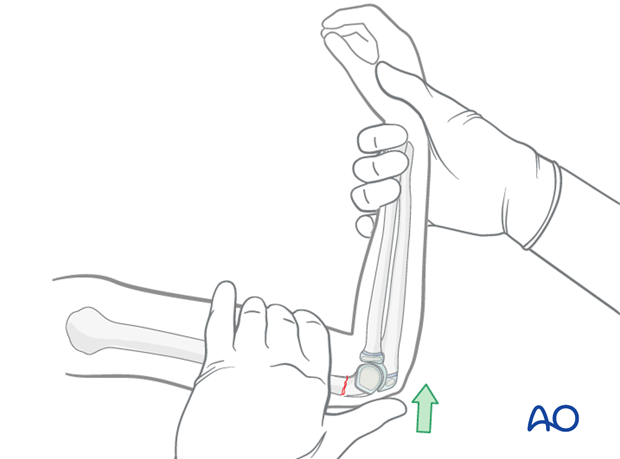
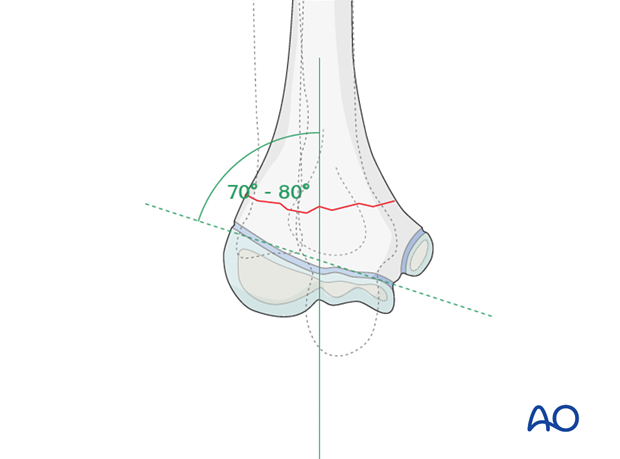
The elbow is maintained in maximal possible flexion and the reduction is verified on an AP image. Baumann's angle should be correct (70-80°) at this stage.
Visually evident varus malposition should not be accepted. The carrying angle should be equal to the opposite arm.
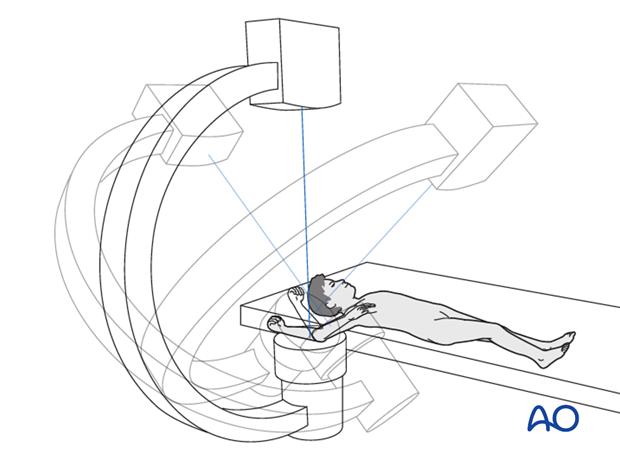
The reduction is also verified on a lateral view taken by externally rotating the entire arm as a unit held with the elbow maximally flexed.
An alternative is not to rotate the arm, but to rotate the C-arm.
Note: Anatomical closed reduction is the objective of this procedure.
See also the additional material on closed reduction of supracondylar fractures.
4. Splint application
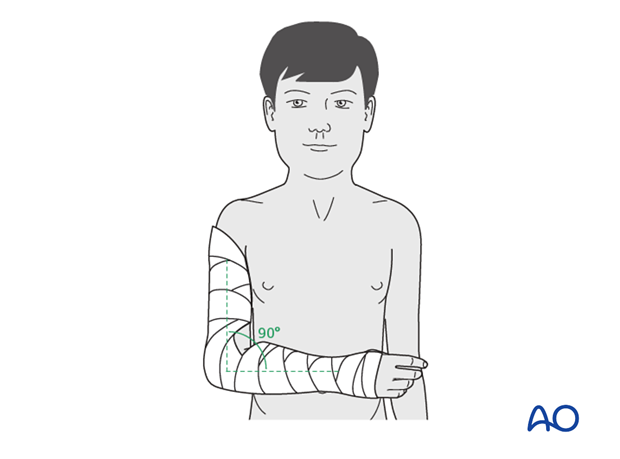
With the elbow positioned in 90° of flexion, a posterior plaster backslab is applied.
The addition of medial and lateral slabs stiffens the splint and prevents it from flexing and extending.
Application of cast padding
Cast padding is wrapped around the upper arm, elbow, forearm and hand, as far as the transverse flexor crease of the palm (the MP joints are left free). According to surgeon's preference a tubular bandage may be applied to the arm beneath the padding.
The elbow is held in 90° flexion and the forearm in neutral rotation.
It is important to make sure that the epicondyles of the humerus and the antecubital area are padded well.
Application of splint
A splint of fiberglass or plaster is applied on the posterior aspect of the arm and forearm. It should be wide enough to cover more than half the circumference of the arm and forearm.
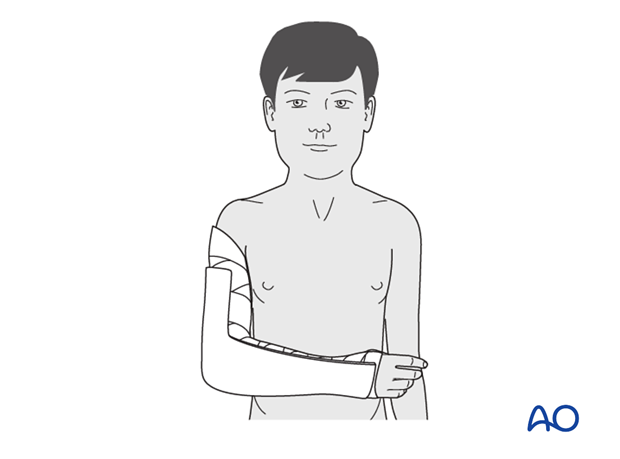
The splint is secured with a noncompressive bandage.
It is very important to ensure that this is not tight and can accommodate subsequent swelling.

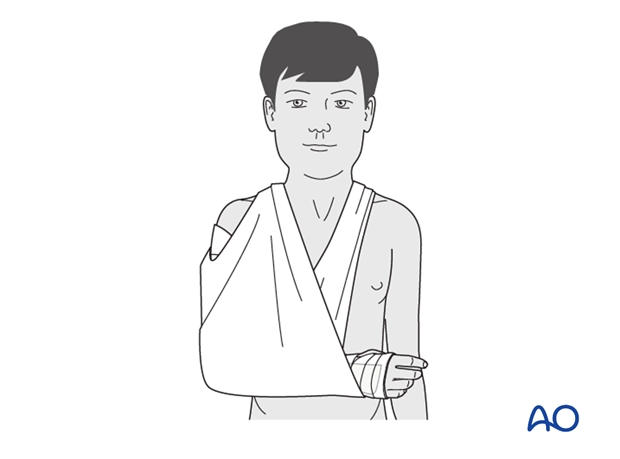
Sling
The injured arm is supported with a sling.
Analgesia
Nonnarcotic analgesia may be required.
Caregivers should be taught to monitor for excessive pain or other signs of potentially dangerous swelling.
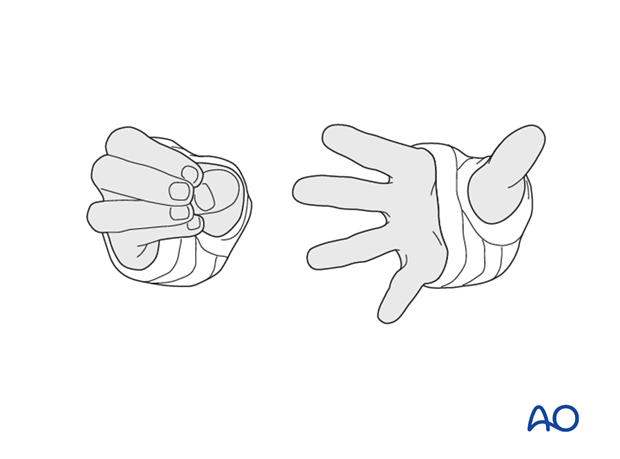
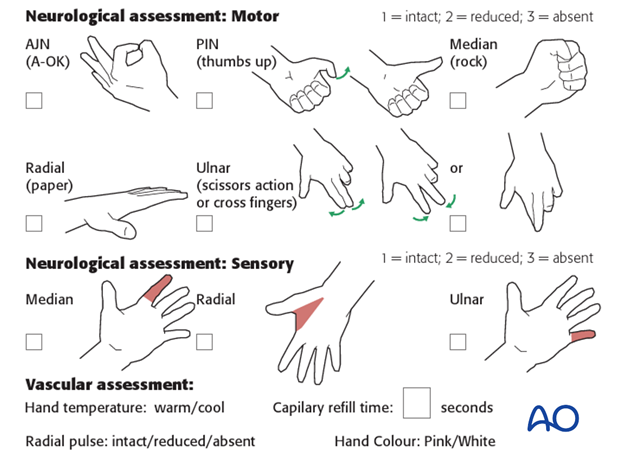
The ability to passively or actively fully extend the fingers without discomfort indicates normal perfusion and absence of neurological compression.
5. Aftercare
Supracondylar humeral fractures heal rapidly and often within 3–5 weeks.
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The child should be examined frequently, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Increasing pain, decreasing range of finger motion, or deteriorating neurovascular signs should prompt consideration of compartment syndrome.
Discharge care
When the child is discharged from the hospital, the parent/caregiver should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger motion.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.

Follow-up x-rays
Control x-rays may be taken at one week following injury to assess fracture position. Further x-rays may be necessary at three weeks to assess fracture healing. This should be performed after the splint has been removed.
Removal of cast or splint
Splints or casts are usually removed within 3 weeks of the injury.
Recovery of motion
As symptoms recover, the child should be encouraged to remove the sling and begin active movements of the elbow.
The majority of elbow motion is recovered rapidly, usually within two months of splint removal. The older child may take a little longer.
Once the child is comfortable, with a nearly complete range of motion, he/she may resume noncontact sports incrementally. Resumption of unrestricted physical activity is a matter of judgment for the treating surgeon.













