Minimally invasive cannulated screw fixation
1. Introduction
Goals
The main goals of treatment of these fractures are:
- Uncomplicated healing
- No secondary displacement
- Avoiding overgrowth due to unstable fixation
- Avoiding secondary complications, such as nonunion, leading to additional problems (eg, ulnar nerve irritation)
Principles
The main principles for this treatment are:
- Anatomical reduction
- To get initial stable fixation (by screw fixation)
- Minimally displaced fractures with a gap up to 2-3 mm are mostly incomplete at the joint level (so-called "hanging fractures"), especially in younger children with very thick joint cartilage. Only such fractures can be treated with closed reduction and insertion of a cannulated screw from behind, to close the gap and stabilize the fracture
Suitable fracture types
13-E/4.1L with no more than 2 mm of metaphyseal displacement, and stable in the joint.
Note: Salter-Harris IV fractures of the medial column are very rare. Care must be taken not to damage the ulnar nerve and they should only be treated by open procedure.

General considerations
Normally, all undisplaced intraarticular fractures (which in children always are epiphyseal fractures) require absolute anatomical reduction, which can only be performed by an open method. However, for "hanging fractures" minimally invasive treatment can be attempted.
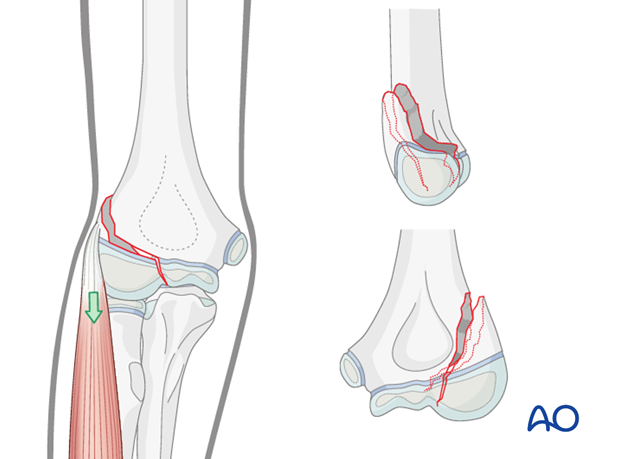
The problem of any nonoperative treatment of this fracture is that the fracture can be completed and displaced by extensor muscle tension, thereby becoming unstable (as illustrated). It is therefore recommended that the fracture be fixed by insertion of a metaphyseal compression screw.
2. Preparation
Instruments and implants
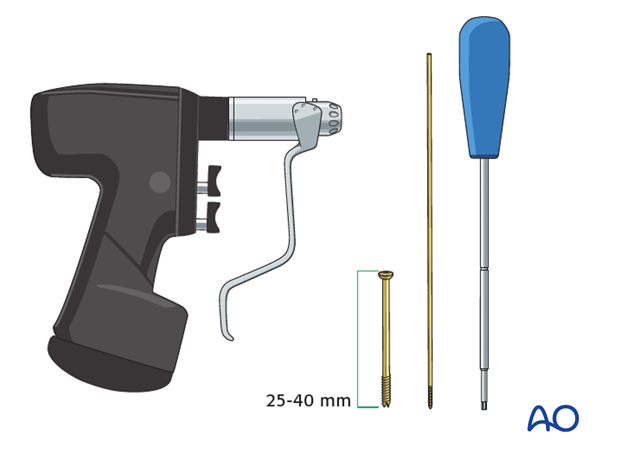
As this is a minimally invasive surgical technique, only a few instruments are necessary.
3.0 or 3.5 mm cannulated cancellous lag screws (ideally self-drilling, self-tapping titanium screws) should be used.
The following equipment is needed:
- Cannulated screw set
- Drill
- Cannulated screws (length 25-40 mm)
- 1.25 mm threaded guide wire
- Image intensifier
- If necessary, contrast medium for arthrography
Anesthesia and positioning
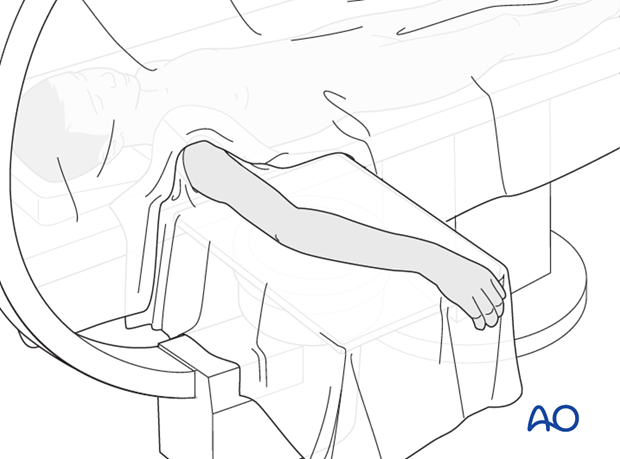
General anesthesia is recommended and a sterile tourniquet should be available. Muscle relaxation is not necessary.
The patient is placed supine with the arm draped up to the shoulder.
3. Reduction and fixation
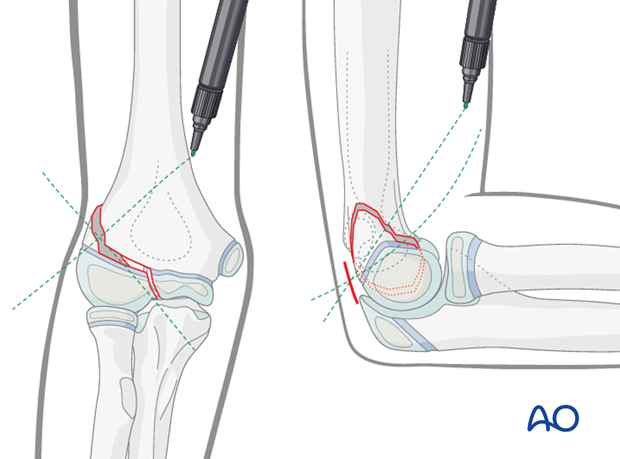
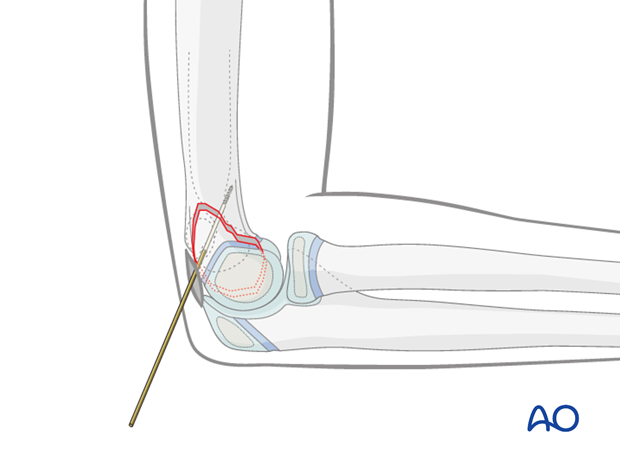
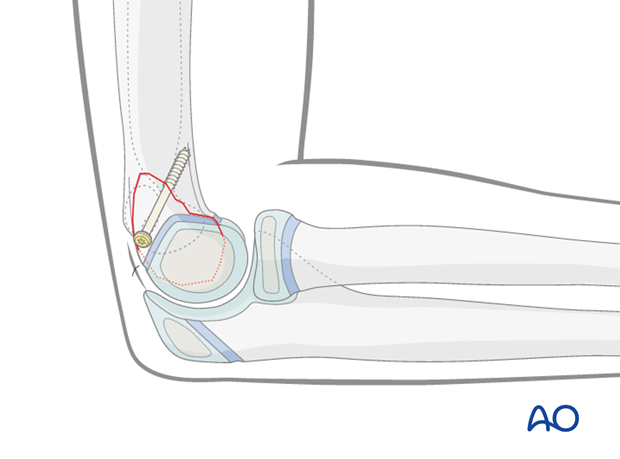
Planning of the entry point
In the AP view, a line is drawn from the most prominent part of the visible capitellum and perpendicular to the fracture.
The arm is positioned in a clear lateral view and a line is drawn from the posterior metaphyseal fragment to the anterior cortex (as illustrated).
The crossing point of these two lines on the skin is the entry point for the guide wire.
Skin incision and approach to the bone
A small (5 mm) skin incision is made using a pointed knife.
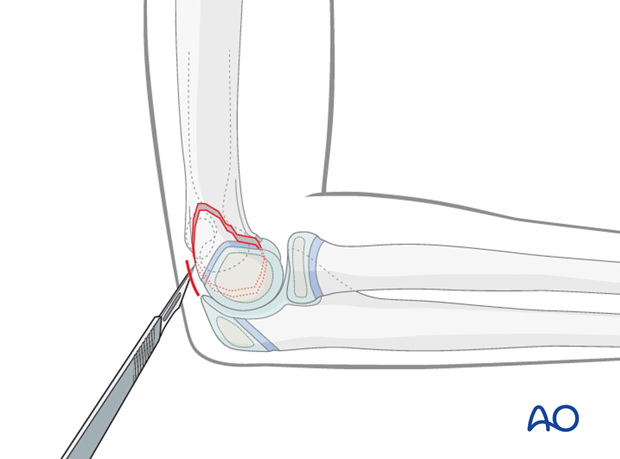
The wound is deepened by blunt dissection using a small artery forceps, down to bone contact.
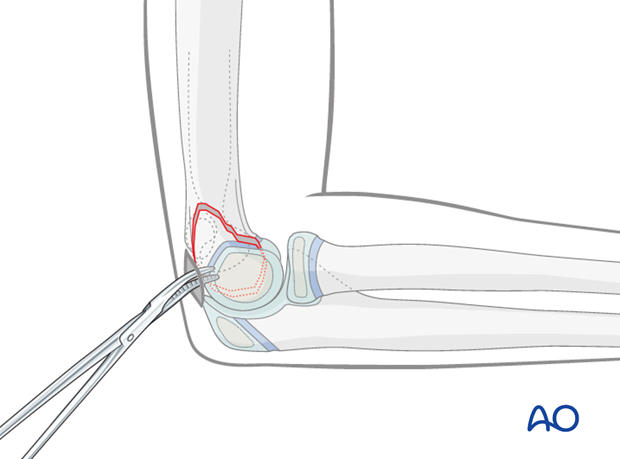
Guide wire insertion for cannulated screws
A 1.25 mm threaded guide wire is used for the cannulated screw.
The guide wire is inserted by hand until it has good bone contact.
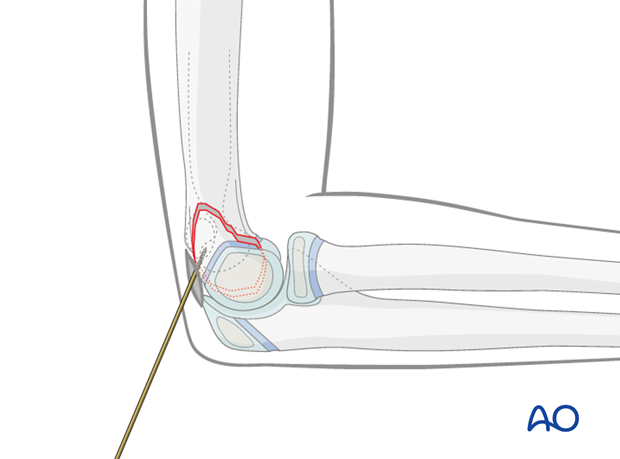
The guide wire is then advanced 1-2 mm inside cartilage of the capitellum.
The position and direction are checked in AP and lateral views using an image intensifier.
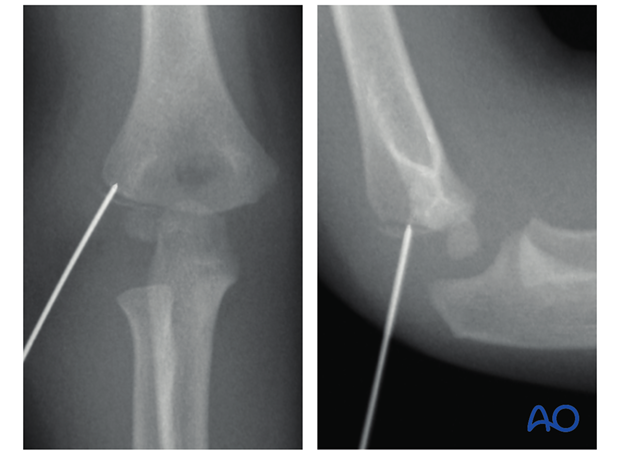
Once the position and direction are correct, the guide wire is advanced as far as the anterior cortex in a lateral view.
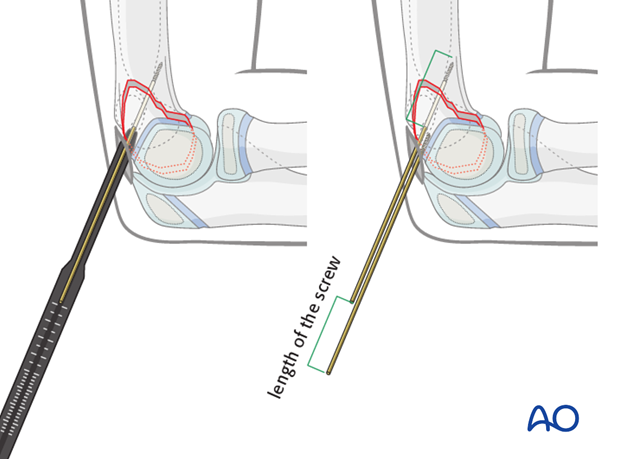
Screw insertion
The appropriate screw length and size can be determined in two different ways:
- By using a measuring device
- By positioning a second guide wire, of the same length, with its tip on the bone at the entry point and measuring the difference between the protruding lengths of the two wires
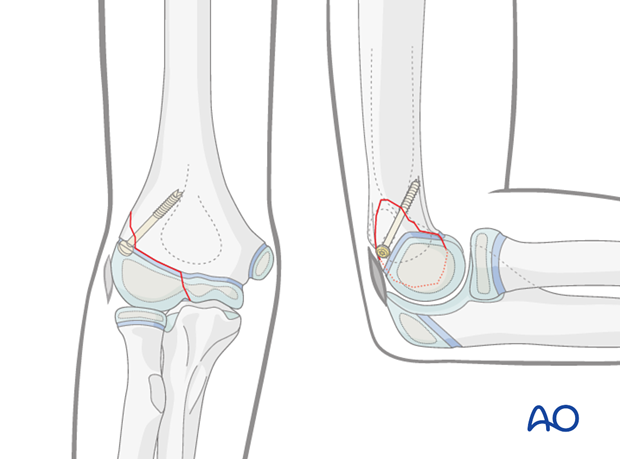
Note: According to the posterior/anterior orientation of the guide wire, the cortex is perforated in the AP view, not on the medial border, but almost centrally in the humerus.
The screw is passed by hand over the guide wire, the screw driver is placed over the guide wire, and the screw is fully inserted.
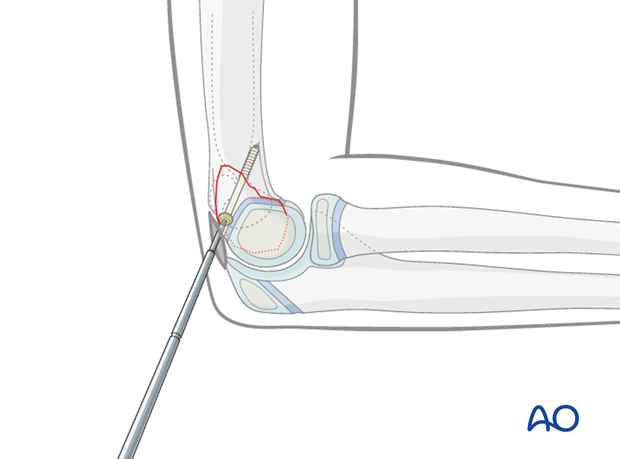
The screw positon and fragment compression are verified using image intensification.
The small incision is closed with one suture or a strip.
4. Aftercare
Note: According to the age of the child, plaster cast or posterior splint immobilization for two weeks (for pain management) can be useful. In children of school age, an arm sling is sufficient. Depending on the level of pain, early movement is allowed for gentle daily activities only.
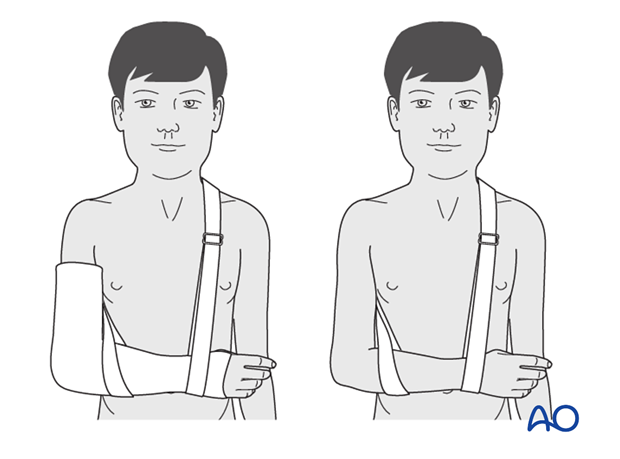
Note: In any case of elbow immobilization by plaster cast, careful observation of the neurovascular situation is essential both in the hospital and at home.
See also the additional material on postoperative infection.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
If the child remains for some hours/days in bed, the elbow should be elevated on pillows to reduce swelling and pain.
The postoperative protocol is as follows:
- Discharge from hospital according to local practice (1-3 days)
- First clinical and radiological follow up, depending on the age of the child, is undertaken 4-5 weeks postoperatively
- In most cases, at this first control, the child is able to move the elbow through a nearly normal range
- During the first clinical follow-up parents/carers should be informed about the timing of implant removal
- Physiotherapy is normally not indicated
Screw removal
The screw can be removed after 2-3 months. Screw removal can be performed as a day case under light general anesthesia.













