Open reduction; screw fixation
1. General considerations
Introduction
Similar principles apply to treatment of avulsion fractures on the lateral and medial side of the distal femur.
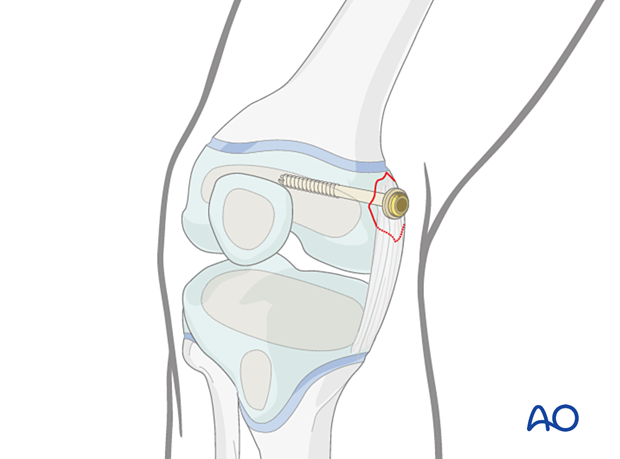
The following example describes reduction and fixation of a medial collateral avulsion injury using a lag screw.
If the bony fragment is very small then a suture anchor may be used for fixation.
Injury types
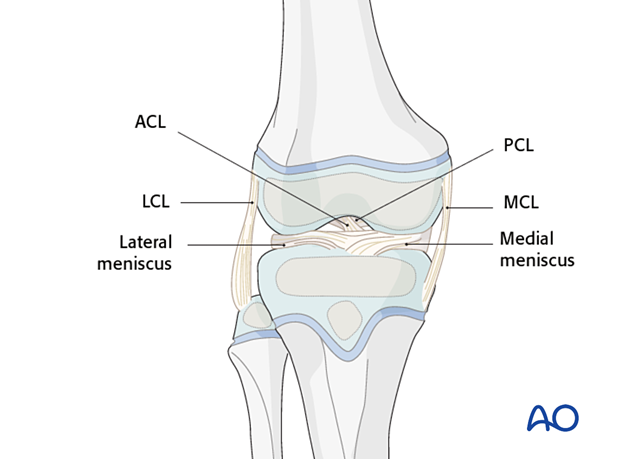
Twisting injuries may result in disruption of the medial or lateral collateral (MCL, LCL), anterior or posterior cruciate ligaments (ACL, PCL).
The MCL and ACL are most commonly injured.
Small avulsion fractures may represent markers of significant injuries, including knee dislocation and require MRI to determine the extent of the injury.
2. Instruments and implants
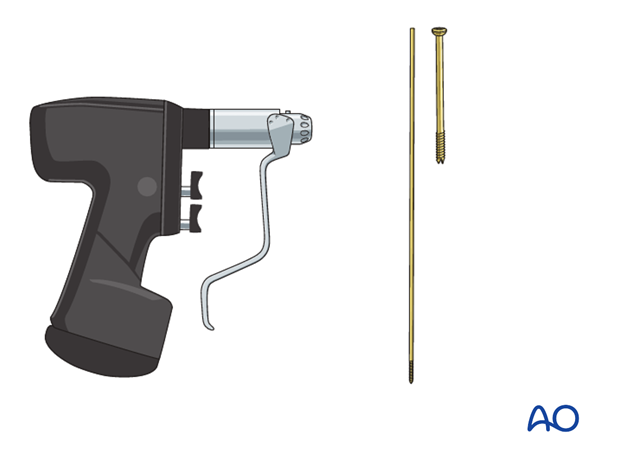
The following equipment is needed:
- Cannulated screw set
- Drill
- Ligament washer
- Threaded guide wire
- Image intensifier
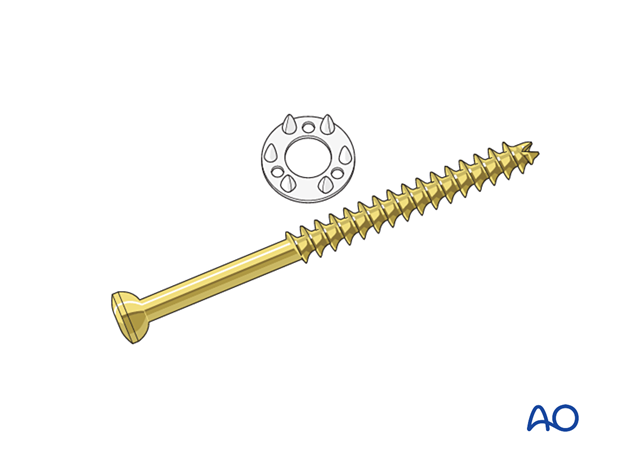
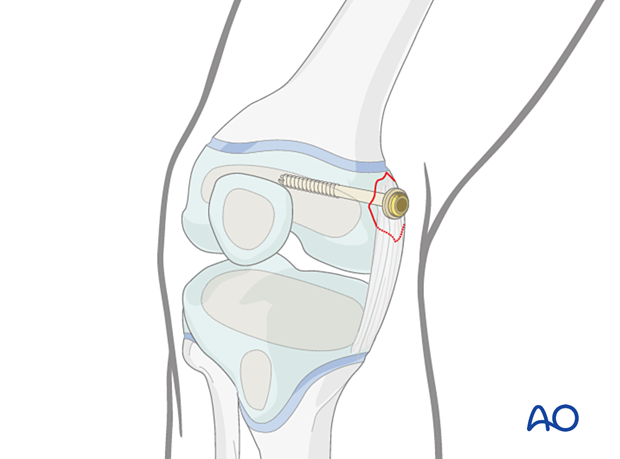
4.0–7.3 mm cannulated lag screws (ideally self-drilling, self-tapping) should be used.
To secure the ligament and small avulsion fragments, a metal or plastic ligament washer can be used with the screw.
3. Patient preparation and approach
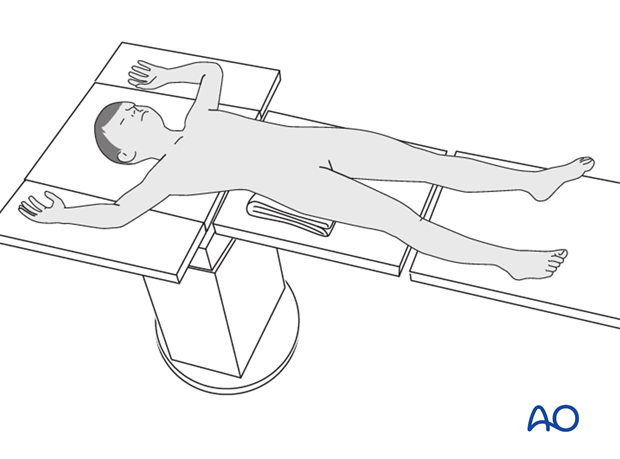
Patient positioning
Place the patient supine on a radiolucent table with a C-arm.
Approaches
For avulsion fractures of the lateral epicondyle, the lower end of the standard lateral/anterolateral approach is used.
For avulsion fractures of the medial epicondyle, a direct medial longitudinal incision is used, deepened to expose the medial face of the medial condyle.
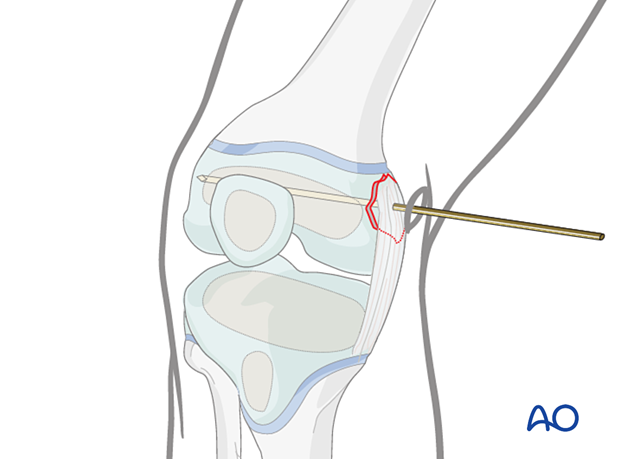
4. Reduction
Reduce the fracture and secure the reduction with the guide wire.
5. Fixation
Insert a screw with or without a ligament washer.
6. Final assessment
Assessment of ligament stability
Gently examine the knee under anesthesia to test for ligament instability.
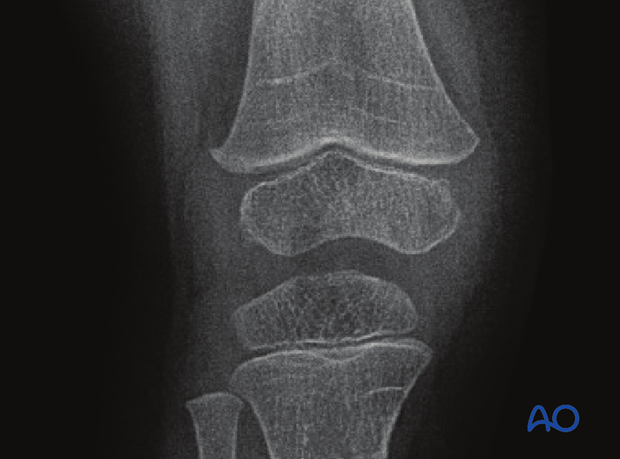
X-ray assessment
Check correct implant positioning and anatomical reduction with image intensification.
7. Aftercare
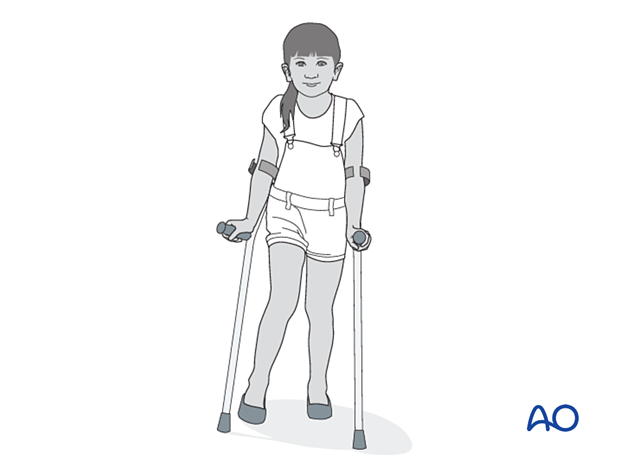
Immediate postoperative care
The patient should get out of bed and begin ambulation with crutches on the first postoperative day.
In most cases the postoperative protocol will be touch-weight bearing for the first 4 weeks.
Analgesia
Routine pain medication is prescribed for 3–5 days postoperatively.
Neurovascular examination
The patient should be examined regularly, to exclude neurovascular compromise.
With displaced high-energy fractures watch for signs of delayed vascular problems.
Compartment syndrome, although rare, should be considered in the presence of severe swelling, increasing pain, and changes to neurovascular signs.
Discharge care
Discharge from hospital follows local practice and is usually possible after 1–3 days.
Follow-up
Clinical and radiological follow-up is usually undertaken 2 weeks postoperatively.
Follow-up for growth deformity
All patients with physeal fractures of the distal femur should have clinical and radiological examination 8–12 weeks postoperatively to assess for signs of physeal growth disturbance or resumption of growth.
Examination should be repeated at intervals until resumption of normal growth is documented. This can be seen as a horizontal growth line (Harris line) that is parallel to the entire physis on both AP and lateral views.
A growth line that converges towards the growth plate may be the earliest sign of growth arrest and should prompt investigation/treatment or referral as appropriate.
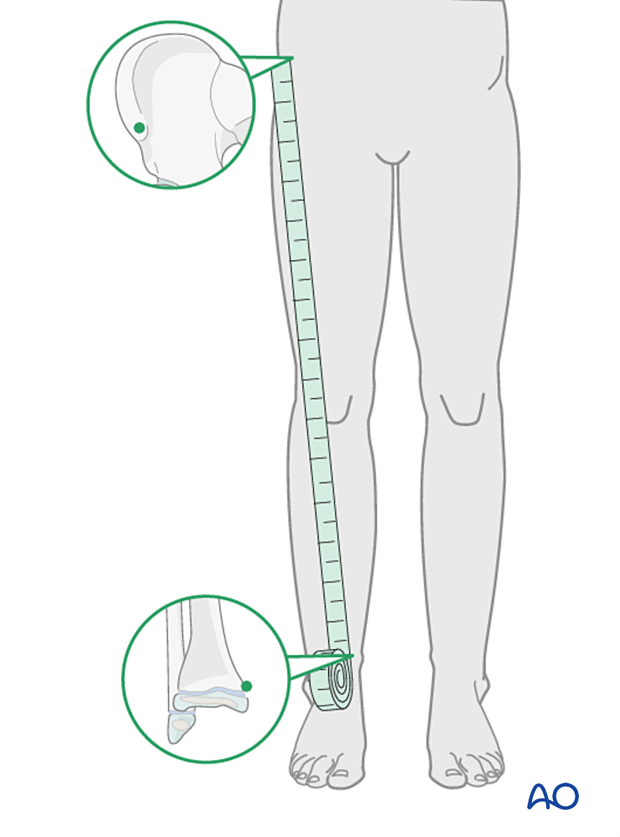
Clinical assessment of leg length and alignment is recommended at one-year.
Clinical assessment of leg length uses a tape measure from the ASIS to the medial malleolus.
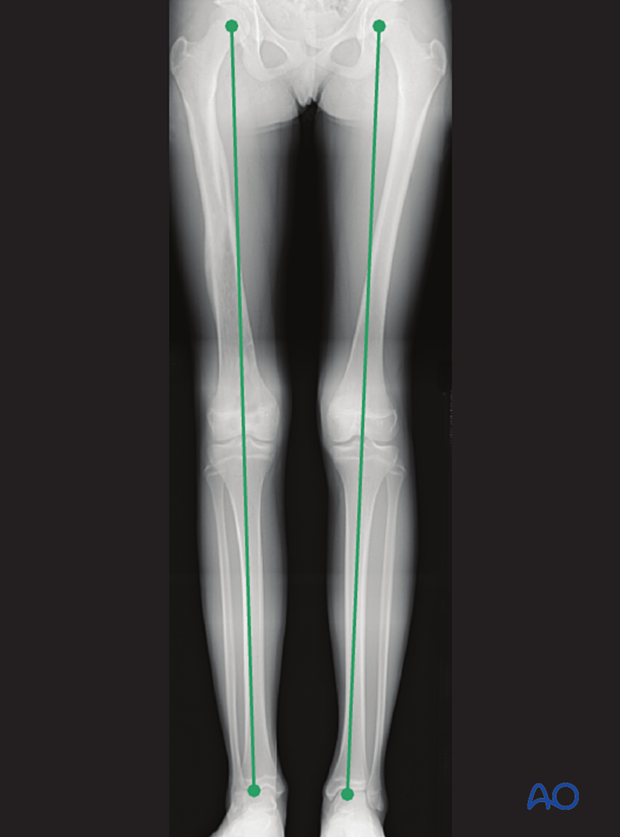
If there is any concern about leg length discrepancy or malalignment, long leg x-rays are recommended.
Leg length is measured from the femoral head to the ankle joint.
Implant removal
If symptoms develop, the screw can be removed once the fracture is completely healed, usually 6–12 months postoperatively.













