Lateral approach to the pediatric distal femur
1. General considerations
The lateral approach allows visualization, reduction and fixation of metaphyseal, physeal, and articular fractures of the distal femur.
More complex intraarticular fractures (particularly those involving the medial femoral condyle) are better exposed with a lateral parapatellar approach.
The lateral approach relies on an atraumatic elevation of the vastus lateralis from the lateral aspect of the distal femur and if required a lateral arthrotomy for joint visualization. The approach can be extended proximally, as described in the lateral approach to the femoral shaft.
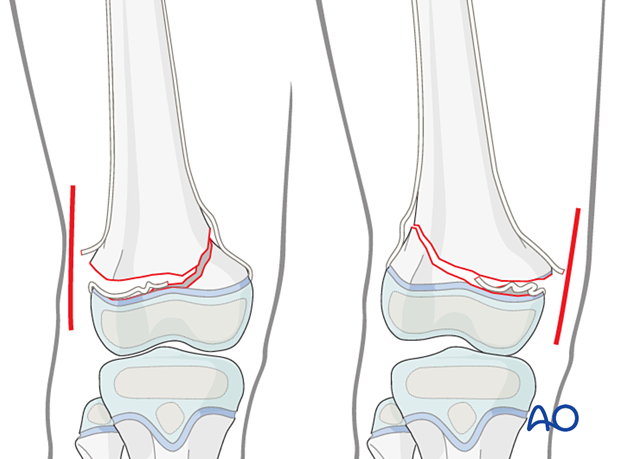
2. Open reduction of Salter-Harris II fractures
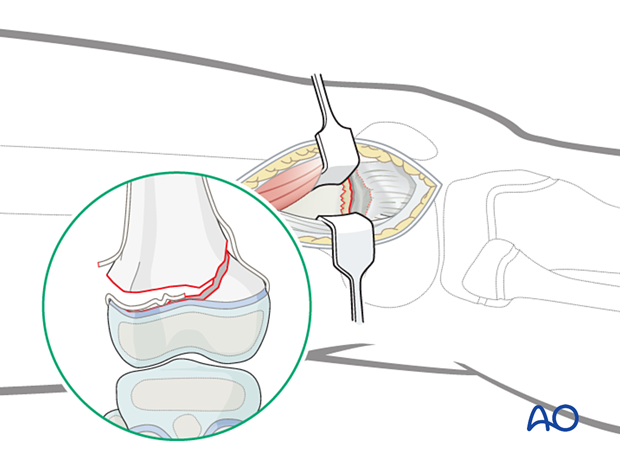
This approach is commonly used if closed reduction of a Salter-Harris II fracture has failed.
In this case the block to reduction is almost always periosteum entrapped in the fracture on the side that has failed in tension. The initial approach should be made from this side.
This means making the initial incision on the side where the shaft fragment is prominent. This is opposite to the side with the metaphyseal (Thurstan Holland) fragment.
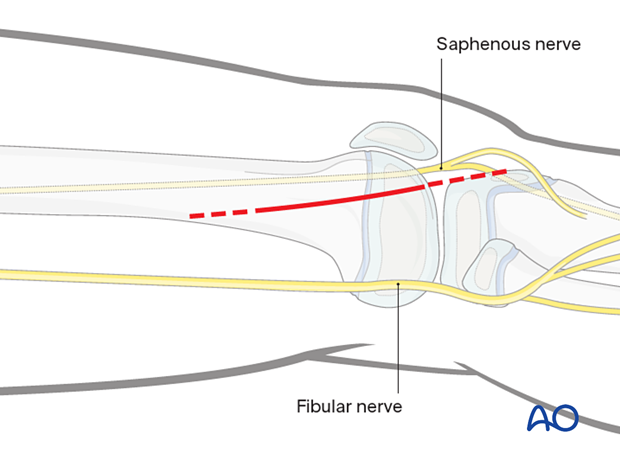
3. Skin incision
Begin the skin incision in the midlateral line of the femoral shaft and curve it anteriorly over the lateral femoral condyle, towards the tibial tubercle. The proximal starting point for the skin incision is often just proximal to the physis if the approach is being used for open reduction of a physeal fracture.
If joint visualization is required, carry the incision to the level of the tibial tubercle (dashed line). If an arthrotomy is not necessary, the skin incision ends at the level of the joint line.

4. Division of the iliotibial band
Divide the iliotibial band in line with the skin incision. Distally, the fibers slope anteriorly towards the tibial tubercle. The incision through the iliotibial band should follow the fiber orientation.
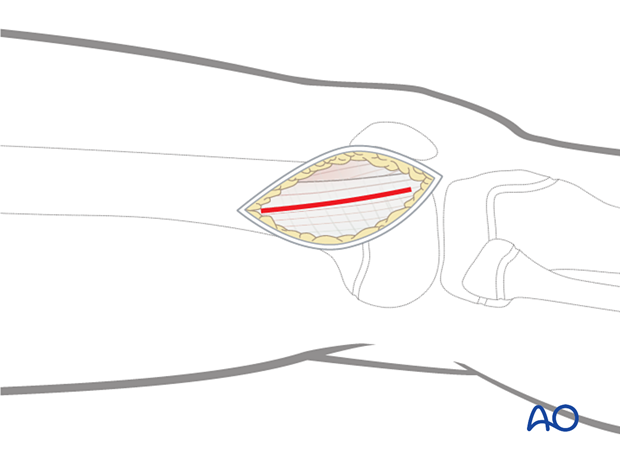
5. Elevation of vastus lateralis
Incise the fascia investing the vastus lateralis at the posterior border of the muscle and follow it proximally and posteriorly. This is most easily accomplished with a large elevator.
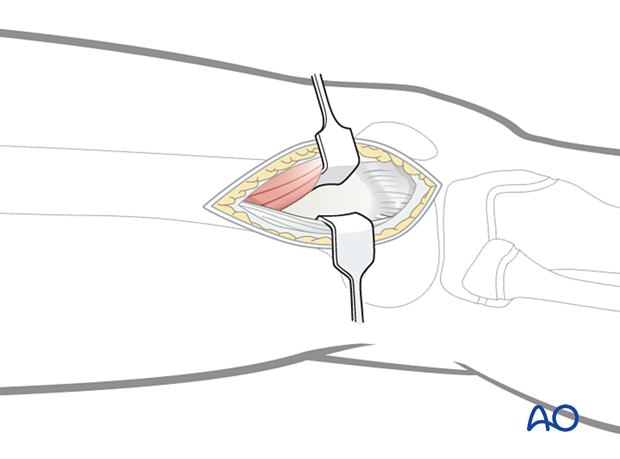
Retract the vastus lateralis anteromedially. A displaced physeal fracture will be immediately evident.
Look for interposed periosteum attached to the distal epiphyseal fragment.
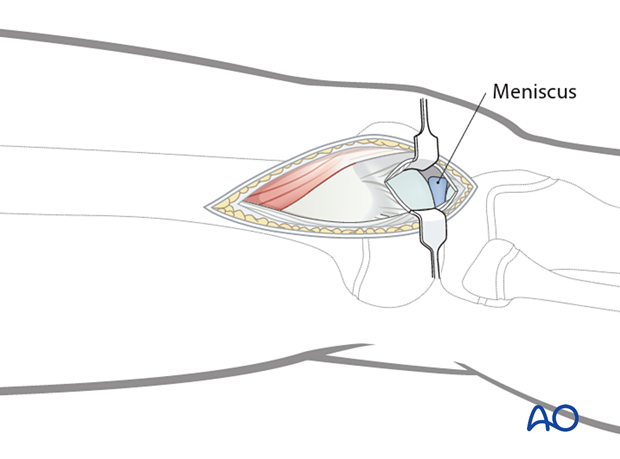
6. Joint capsule arthrotomy for articular surface visualization (optional)
For cases in which the articular surface needs to be exposed, incise the joint capsule over the anterior third of the lateral femoral condyle.
This can be extended distally as far as the lateral meniscus.
A blunt angled retractor can be used to improve exposure of the articular surface.
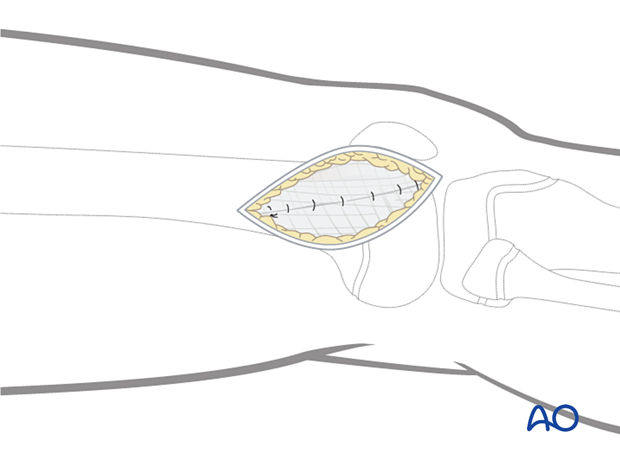
7. Wound closure
Close the joint capsule with absorbable sutures.
Close the fascia of the vastus lateralis with a running absorbable suture or interrupted sutures.
Close the iliotibial band with absorbable sutures.
After careful hemostasis, close the skin and subcutaneous tissues in a routine manner.