ORIF - Compression plating
1. General considerations
Compression plate
The objective of compression plating is to produce absolute fracture stability, prohibiting interfragmentary motion.
Compression plating is mainly useful in two-part fracture patterns, where the bone fragments can be compressed. In wedge fractures, where there are large enough fragments, one or two lag screws should be used to add additional stability of the fracture, either through or outside the plate.
The plate length has to be chosen long enough, so that on both sides of the fracture six cortices will be involved.
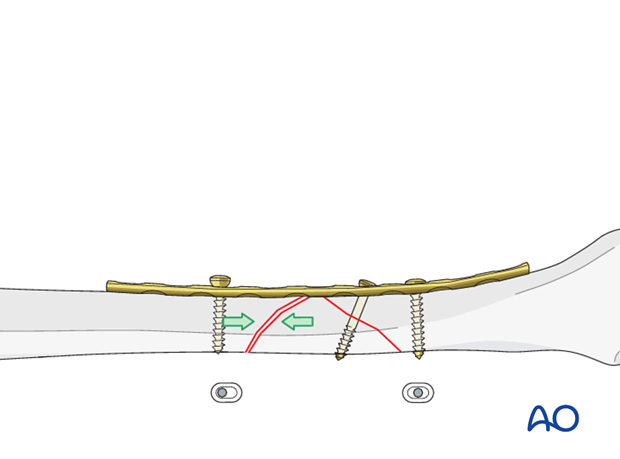
Dynamic compression principle
Compression of the fracture is usually obtained by eccentric screw placement at one or more of the dynamic compression plate holes. These holes are shaped like an inclined and transverse cylinder. The screw head slides down the inclined cylinder as it is tightened, forcing the plate to move along the bone, thereby compressing the fracture.
Before dynamic compression can be applied, the intact wedge has to be fixed to one of the main fragments with a lag screw. Thus an axilla is created which allows compression by eccentric screw insertion.
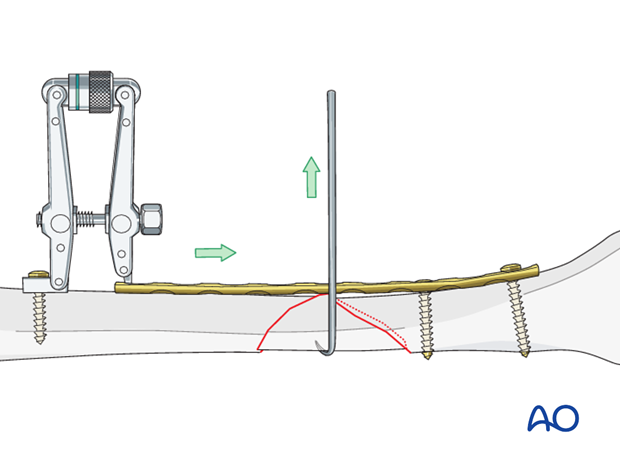
Compression with ATD
In wedge fractures, the articulated tension device (ATD) is more often used to gain length than for compression because of the limited compressibility of these fractures. If a push-pull screw is used the same hole could be used to place the tensioning device.
Note
If too much tension is applied and/or the plate has not been prebent, there is a risk of axial deformity.
2. Patient preparation and approaches
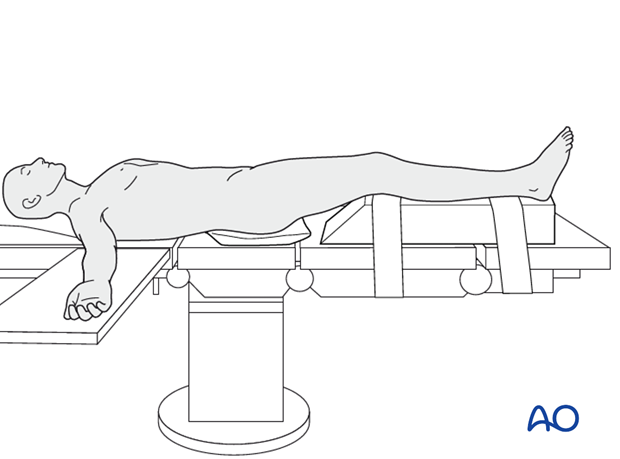
Patient preparation
This procedure is normally performed with the patient in a supine position.
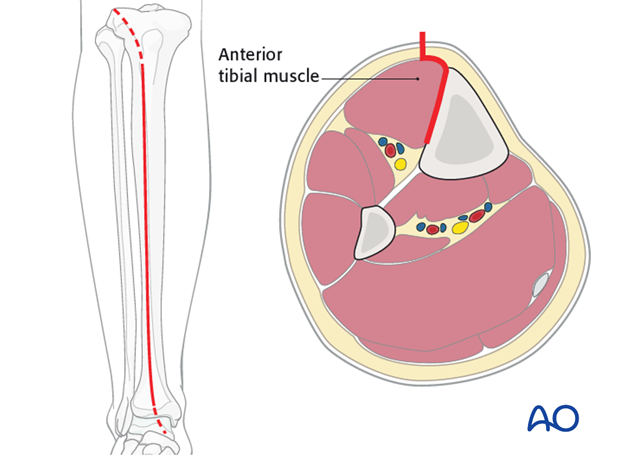
Anteromedial approach
The anteromedial approach is used most commonly for fractures of the distal third tibial shaft. However, it can be used to expose the entire anteromedial surface.
It is also useful for debridement and irrigation of open fractures when an incision on the injured subcutaneous surface is to be avoided.
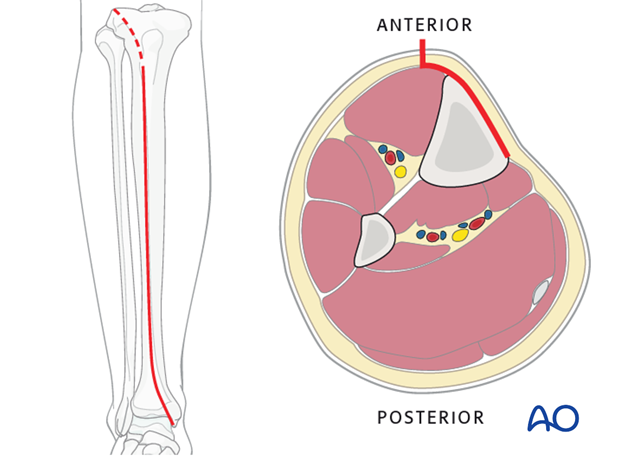
Anterolateral approach
The anterolateral approach is used uncommonly, but may be necessary when the medial soft tissues are compromised.
3. Plate preparation
Overbending the plate
The plate should be overbent at the fracture site approximately 1-2 mm to ensure compressioin of the side opposite the plate.
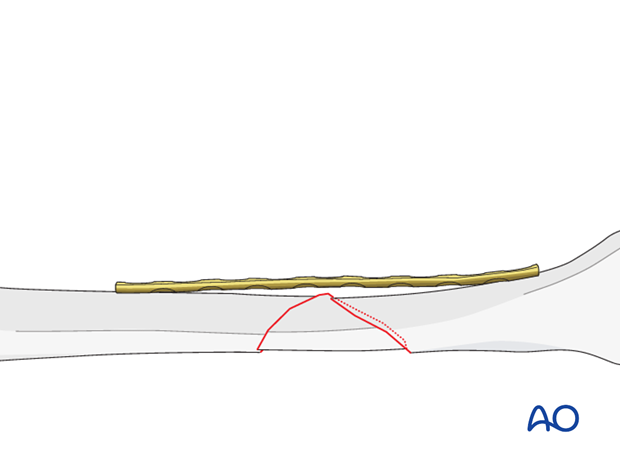
Plate contouring
Twisting the plate
The anteromedial surface of the tibial shaft twists internally approximately 20° as it approaches the medial malleolus.
The first step of plate contouring is to twist the plate so it matches the tibial surface upon which it will lie.
If the plate is bent before it is twisted, the process of twisting will alter the bend that has been created.

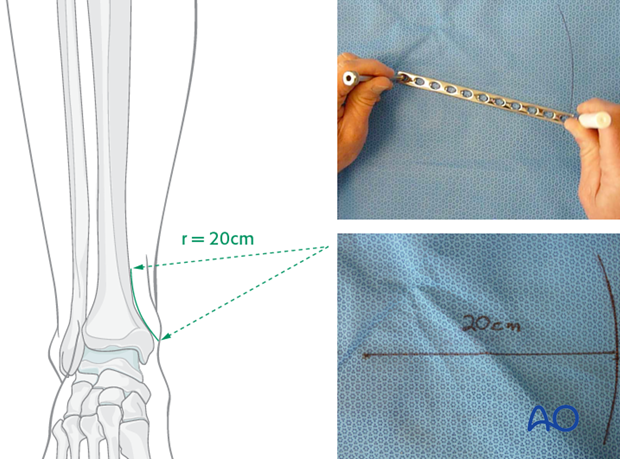
Matching the curvature
Depending upon the plate location, more or less bending of the plate will be required to match the contour of the intact (or reduced) bone. Much of the medial tibial shaft is quite straight, so that little bending is required. However, the distal medial surface has a significant concavity, with a typical radius of curvature of 20 cm as illustrated.
Such a 20 cm radius can be drawn on a sterile drape and used as a template for plates to be used in this location.
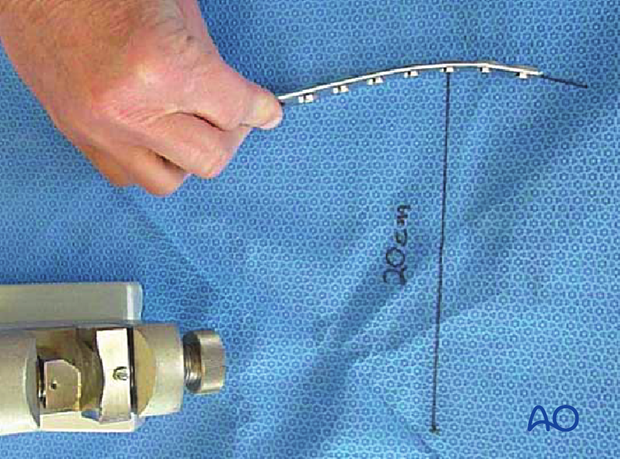
Bending the plate
The plate can be bent with bending irons alone, but it is preferable to bend with a bending press, because the press gives more control.
In either case, the bending is done in small steps to produce a smooth contour. Contouring only takes place over the distal 10-12 cm of the plate. When finished, the plate should match the 20 cm radius of curvature.
4. Reduction and fixation
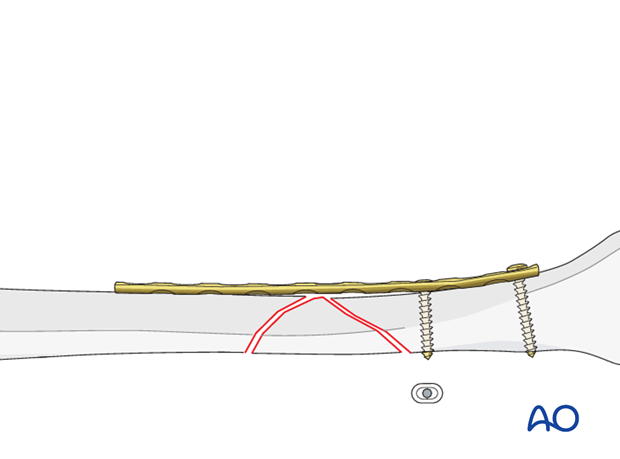
Application of the plate
After contouring, the plate is fixed with two screws to the distal main fragment.
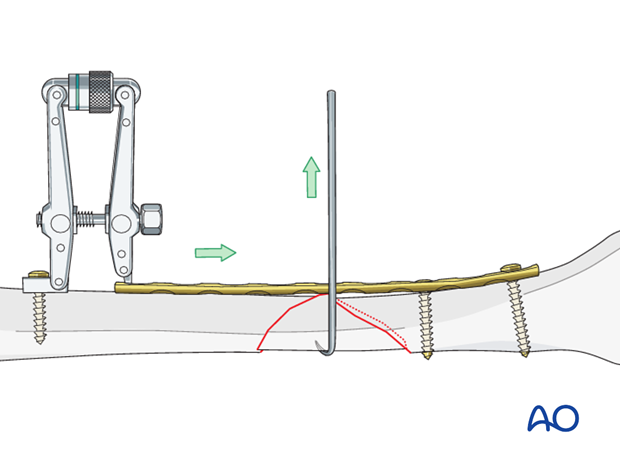
Reduction with the plate
If necessary, the ATD is applied proximally and the fracture is distracted. Gently reduce the wedge fragment with a small hook.
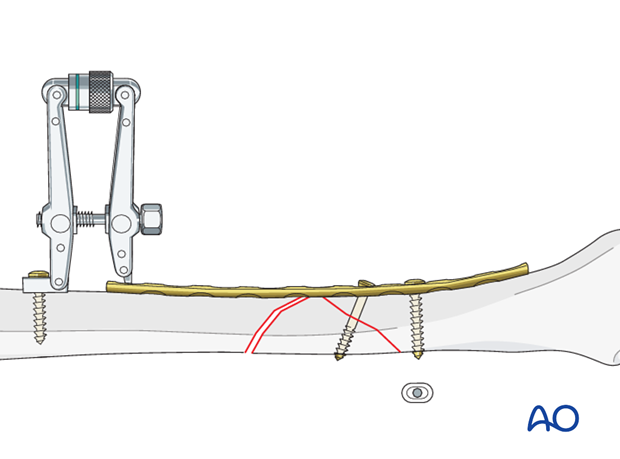
Lag screw
Depending on the fracture configuration, insert one lag screw through or outside the plate. With this lag screw, the wedge fragment is fixed to the distal main fragment.
Dynamic compression
If the ATD has preliminarily been used for reduction, compression can now be applied by converting the ATD from distractor to compressor. After compression of the fracture, insert a screw excentrically next to the fracture into the proximal main fragment.
After reduction without ATD, compression is achieved by inserting a screw in maximally eccentric position (drilling without protection sleeve).
Note
The tension device must be applied in such a way that the spike of the mobile fragment is pressed into the axilla formed by the plate and the other fragments to which it has been fixed.
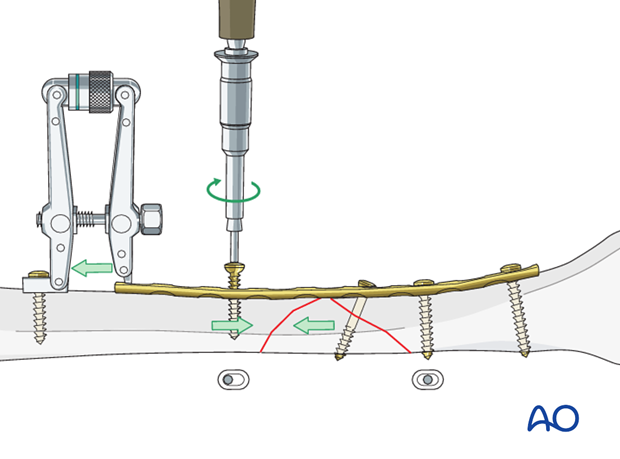
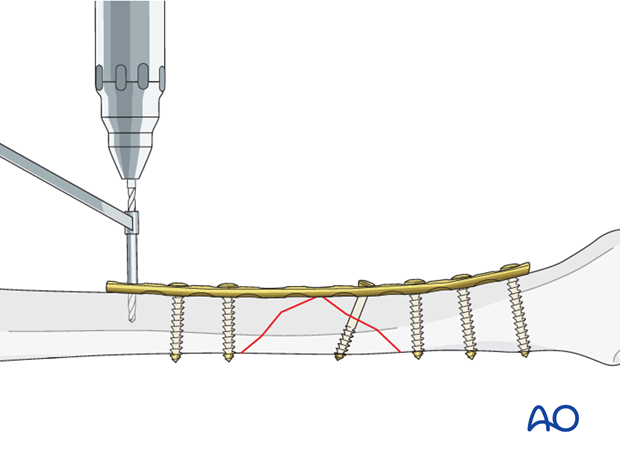
Screw insertion
The remaining screws are then inserted. Screws closest to the fracture site are placed first.
5. Aftercare of tibial shaft fractures
Weight bearing
If weight bearing without plaster is not advisable or possible, a walking cast is a better option than unprotected walking completely without weight bearing.
After intramedullary nailing, weight bearing is allowed in an earlier phase (immediately postoperatively) compared to plate fixation. After the latter, progressive weight-bearing is usually possible after 8-12 weeks.
If external fixation is considered as the definitive device, weight bearing starting at 10–15 kg should be encouraged early, as in plate fixation.
As soon as callus formation is visible and once there are no clinical signs of instability, the patient can start to bear full weight. After removal of the external fixator, it may be prudent to protect the leg temporarily in a splint or brace.
Follow-up
After suture removal 2 weeks after surgery, the patient should be seen every 4-6 weeks in follow-up with examination and x-rays until union is secure, and range of motion and strength have returned.
Inspection of external fixators every two weeks is optional.
Hardware removal
Interlocking screws are always removed.
As far as plates create stress raising, removal is advisable. The earliest time of implant removal being two years postoperatively.













