ORIF - Lag screws with protection plate
1. Principles
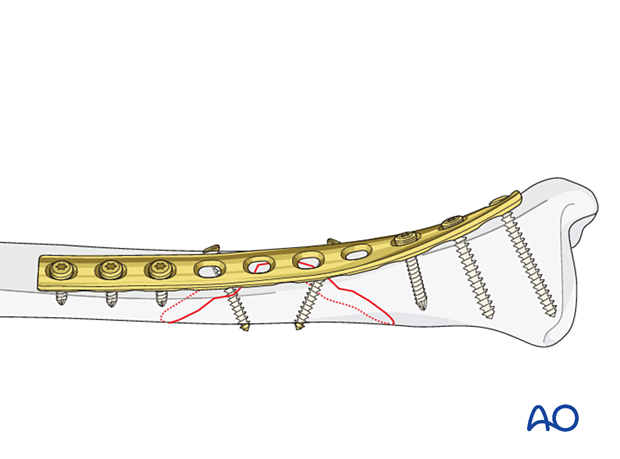
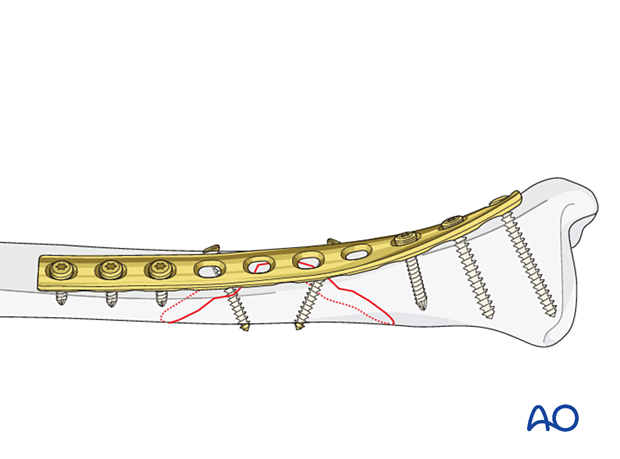
Lag screw and protection plate
If nailing and minimally invasive osteosynthesis (MIO) are contraindicated, open reduction and internal fixation (ORIF) should be performed. If the fracture configuration does not allow axial compression, a lag screw should be used to achieve interfragmentary compression.
Depending on plate position and fracture configuration, the lag screw will be introduced either through a plate hole or outside the plate. Although a lag screw will provide absolute stability, a protection plate must be applied to eliminate shearing and rotational forces.
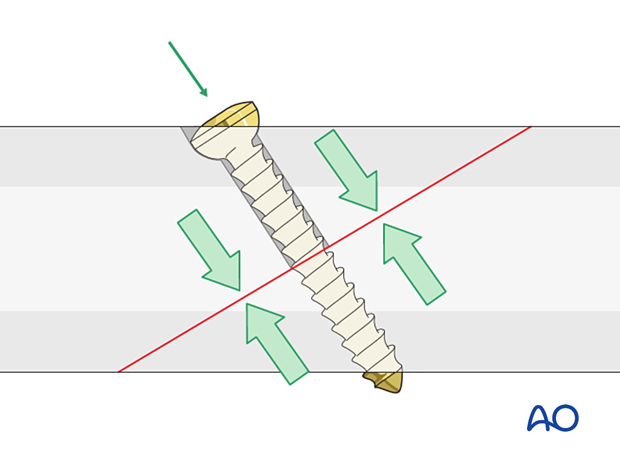
Introduction of a lag screw
Introduce the lag screw as perpendicular as possible to the fracture plane. The lag screw should be placed without soft-tissue stripping and should not interfere with the tibialis anterior tendon or muscle.
If an anterior-to-posterior screw is chosen, it should be sufficiently countersunk. There are two important reasons for countersinking:
- Countersinking ensures that the screw head has the maximal contact area with the bone, so that its compressive forces are widely distributed
- A countersunk screw head is less prominent and leads to less soft tissue irritation
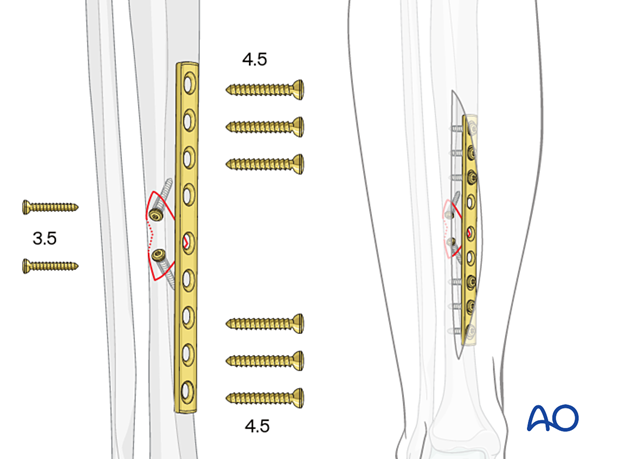
Options for small wedge fragments
Use of 3.5 mm screwsWith small wedge fragments, 4.5 mm screws may be too large. They can be replaced with 3.5 mm or 2.7 mm lag screws. Given the typical size and load for the tibia, a 4.5 mm narrow dynamic compression plate (DCP) or a pre-contoured 3.5 mm locking compression plate (LCP) can be used as a protection plate.
2. Patient preparation and approaches
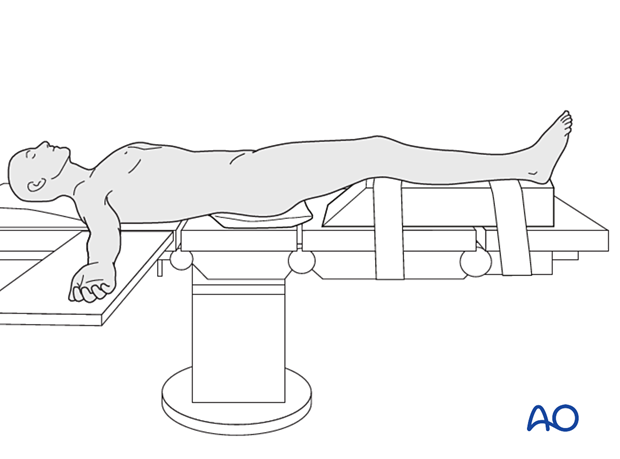
Patient preparation
This procedure is normally performed with the patient placed in a supine position.
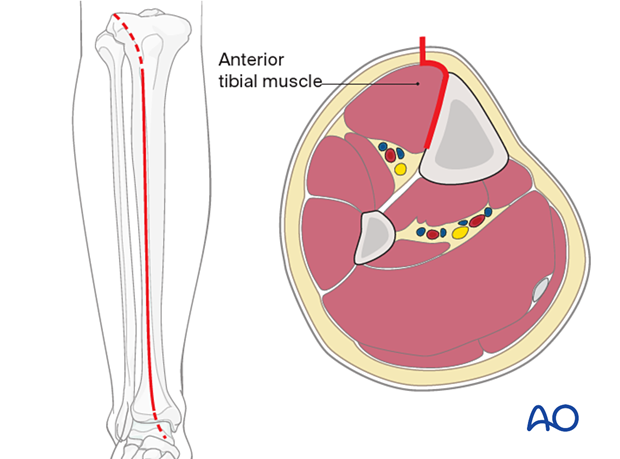
Anteromedial approach
An anteromedial approach can be used if the soft-tissue envelope allows. The advantage of this approach is that it does not remove muscle from the fracture fragments. Also, the medial surface of the tibia is normally flat, and conventional plates can be contoured to fit it or pre-contoured plates used with minimal or no modification.
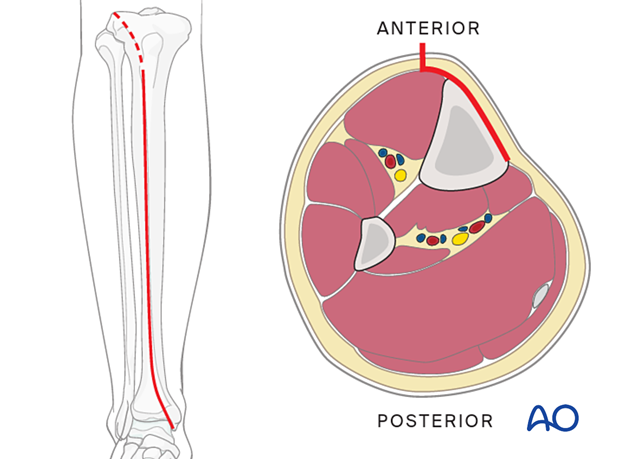
Anterolateral approach
The anterolateral approach can also be used if the plate is best placed on the lateral surface of the tibia. It can also be used when the medial soft tissues are compromised.
3. Reduction
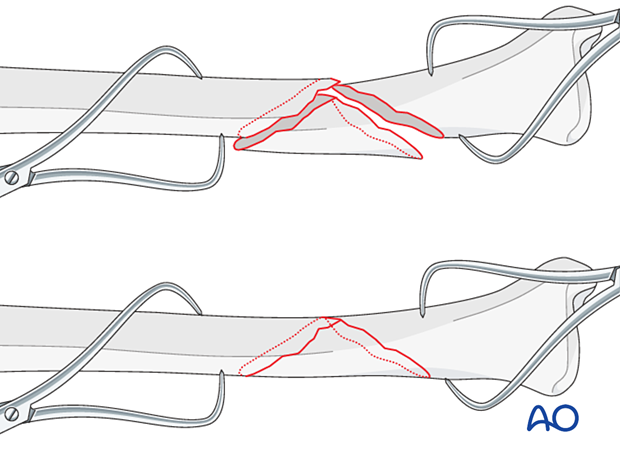
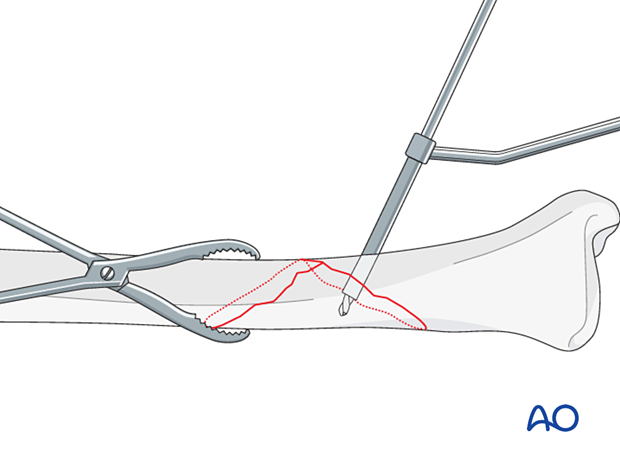
As the fracture is reduced with pointed reduction forceps it is also rotated into its anatomic position.
Pointed reduction forceps are best used in long oblique or spiral fractures where the reduction can be visualized over a longer length of the tibia. In short oblique fractures where only part of the reduction is visible, the axial alignment must be double-checked.
4. Lag screw insertion
Gliding hole
Use a 4.5 mm, 3.5 mm, or 2.7 mm drill (according to the chosen screw size) to create a gliding hole, located centrally across the fracture plane, away from the fracture line, and angled perpendicular to the fracture plane at the chosen location.
Drill the near cortex only, using an appropriate drill sleeve.
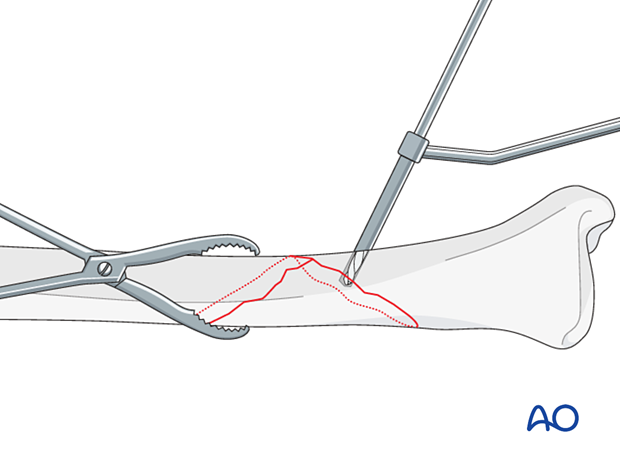
Pilot hole for the thread
Insert an appropriately sized drill sleeve through the gliding hole to contact the far cortex.
Drill through the sleeve with the appropriate drill for the pilot hole, 3.2 mm for large fragment screws, 2.5 mm or 2.0 mm for small fragment screws.
Screw insertion
Measure the length of the screw and prepare the far cortex with the appropriate tap. Insert the chosen screw, tightening it carefully.
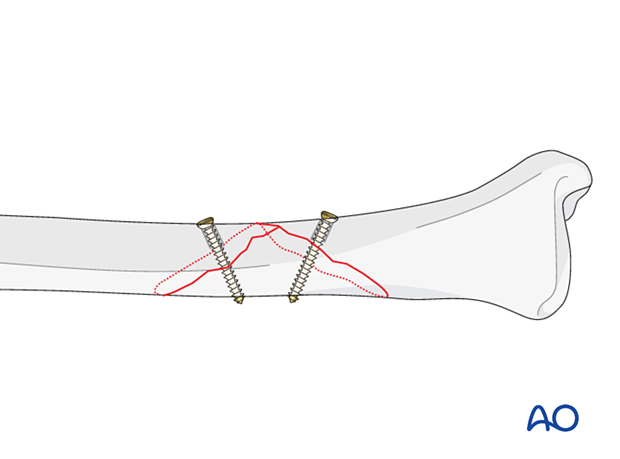
For longer spiral fractures, a second screw is inserted, using a similar technique. Both screws should be placed as perpendicular to the fracture plane as possible at the site where they are inserted.
Avoid placing screws at the end of the fracture segments as this may fracture the end of these segments, making the simple fracture pattern a complex, multifragmentary pattern where this technique is contraindicated.
5. Plate preparation
Determining length of plate (narrow 4.5 mm plate)
The plate length is determined by the fracture pattern and the fracture location. Choose a plate which is long enough to allow placement of three screws proximal and three screws distal to the fracture zone.
Traditionally a 4.5 mm plate has been advised for the tibial shaft. Advantages include increased plate thickness and larger screw size for added strength. These plates are difficult to contour and may be too prominent, however.
A 3.5 mm plate offers improved contourability and multiple screw options in metaphyseal (end-segment) zones. As these plates are thinner, they are less stiff than the large fragment plates.
Another consideration is the choice between an anatomically pre-contoured plate or one which the surgeon contours. For plates that need to be contoured, the following steps must be employed.
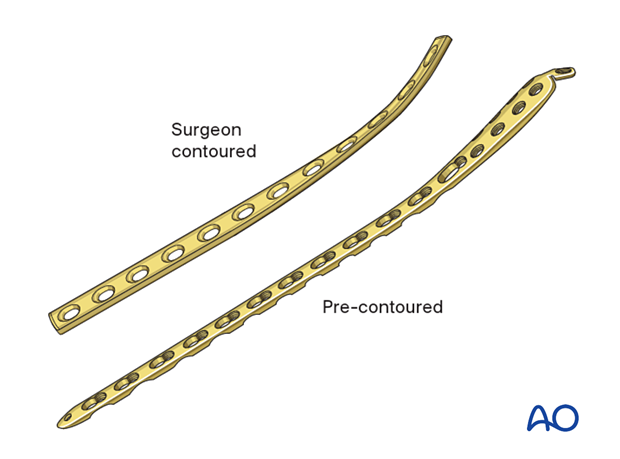
Plate contouring
Twisting the plateThe anteromedial surface of the tibial shaft twists internally approximately 20° as it approaches the medial malleolus.
The first step of plate contouring is to twist the plate so it matches the tibial surface upon which it will lie.
If the plate is bent before it is twisted, the process of twisting will alter the bend that has been created.
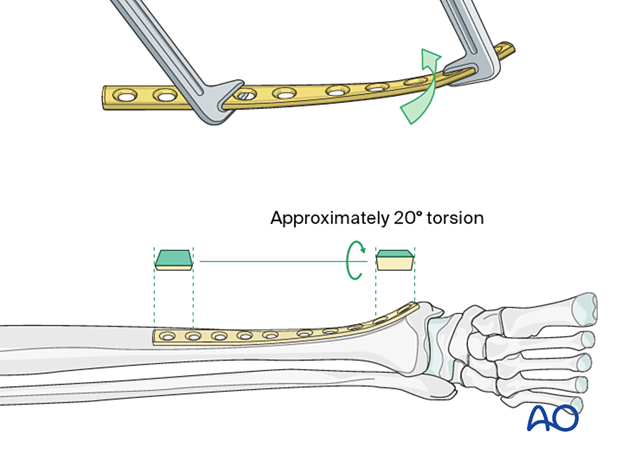
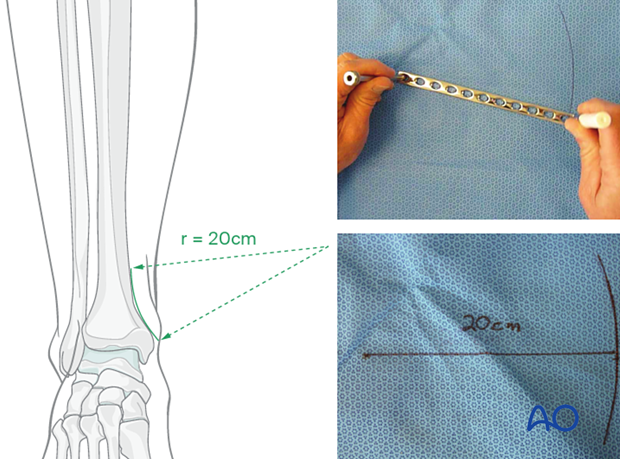
Depending upon the plate location, more or less bending of the plate will be required to match the contour of the intact (or reduced) bone. Much of the medial tibial shaft is quite straight so that little bending is required. The distal medial surface has a significant concavity, with a typical radius of curvature of 20 cm as illustrated.
A 20 cm radius can be drawn on a sterile drape and used as a template for plates to be used in this location.
The plate can be bent with bending irons alone, but bending with a bending press is preferable because it gives more control.
In either case, the bending is done in small steps to produce a smooth contour. Contouring only takes place over the distal 10–12 cm of the plate. When finished, the plate should match the 20 cm radius of curvature.
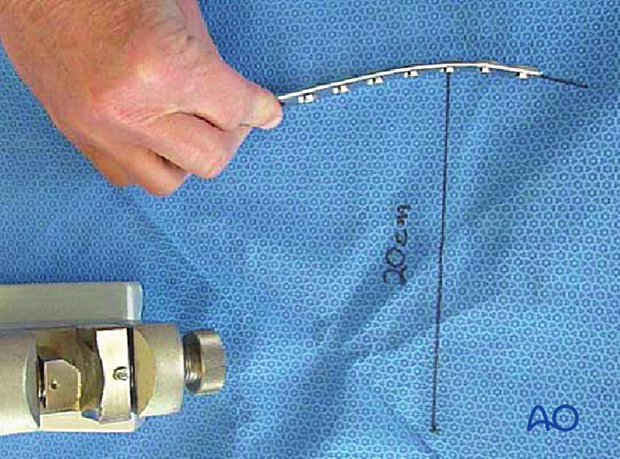
An aluminum template is contoured to the anatomically reduced fracture in the position where the plate is to be applied. The plate is then shaped to match the template.
6. Plate fixation
Application of the plate
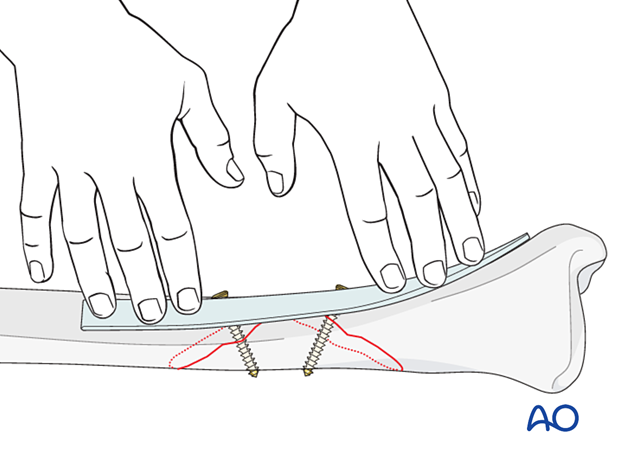
No periosteal stripping should be done, either for plate fixation or screw placement, but there must be enough soft tissue exposure to provide an area for the plate.
Rather than clamping the plate to the bone, it is often helpful to hold the plate to the bone with one well-placed screw in order to confirm that it is contoured correctly.
Be careful not to displace the fracture, as initial lag screws may lack strength. If possible, leave a reduction clamp across the fracture during plate application.
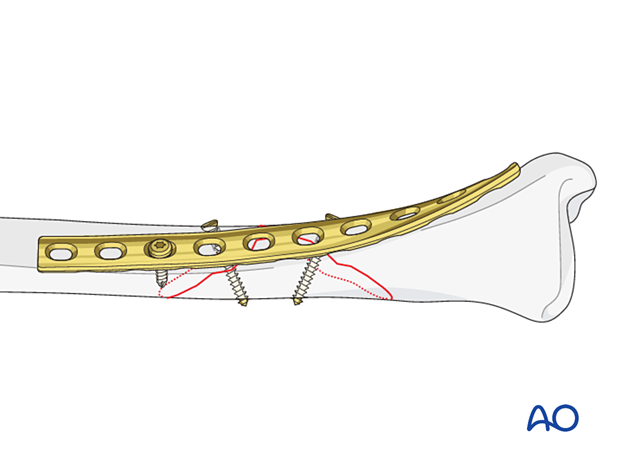
Insert remaining screws
Then insert the rest of the screws in neutral mode.
Screws closest to the fracture site are placed first.
7. Aftercare
Perioperative antibiotics may be discontinued before 24 hours.
Attention is given to:
- Pain control
- Mobilization without early weight bearing
- Leg elevation in the presence of swelling
- Thromboembolic prophylaxis
- Early recognition of complications
Soft-tissue protection
A brief period of splintage may be beneficial for protection of the soft tissues but should last no longer than 1–2 weeks. Thereafter, mobilization of the ankle and subtalar joints should be encouraged.
Mobilization
Active, active assisted, and passive motion of all joints (hip, knee, ankle, toes) may begin as soon as the patient is comfortable. Attempt to preserve passive dorsiflexion range of motion.
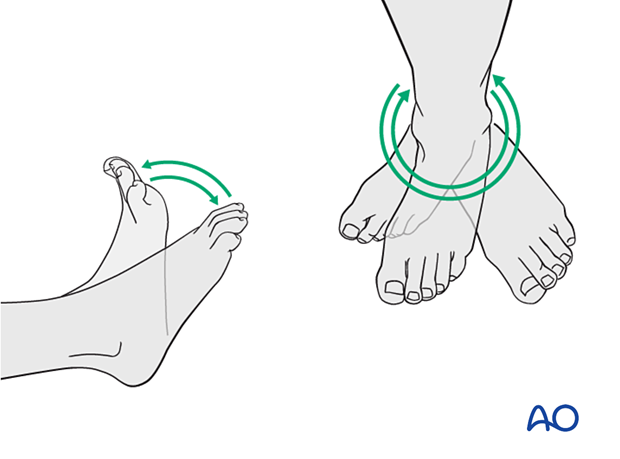
Weight bearing
For fractures treated with plating techniques, limited weight bearing (15 kg maximum), with crutches, may begin as tolerated, but full weight bearing should be avoided until fracture healing is more advanced (8–12 weeks).
For fractures treated with intramedullary nailing, weight bearing as tolerated, with crutches, may begin immediately.
Follow-up
Follow-up is recommended after 2, 6, and 12 weeks and every 6–12 weeks thereafter until radiographic healing and function are established. Weight bearing can be progressed after 6–8 weeks when x-rays have indicated that the fracture has shown signs of progressive healing.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation caused by the implants. The best time for implant removal is after complete bone remodeling, usually at least 12 months after surgery. This is to reduce the risk of refracture.













