ORIF - Compression plating
1. Principles
Wedge fractures can also be treated with compression plating. Although this provides absolute stability, it requires direct reduction methods which carry an increased risk of wound-healing complications.
Compression plating
The objective of compression plating is to produce absolute fracture stability, prohibiting interfragmentary motion.
Compression plating is mainly useful in two-part fracture patterns, where the bone fragments can be compressed. In wedge fractures, where there are large enough fragments, one or two lag screws should be used to add additional stability to the fracture, either through or outside the plate.
The plate length has to be long enough so that on both sides of the fracture six cortices of purchase will be obtained.
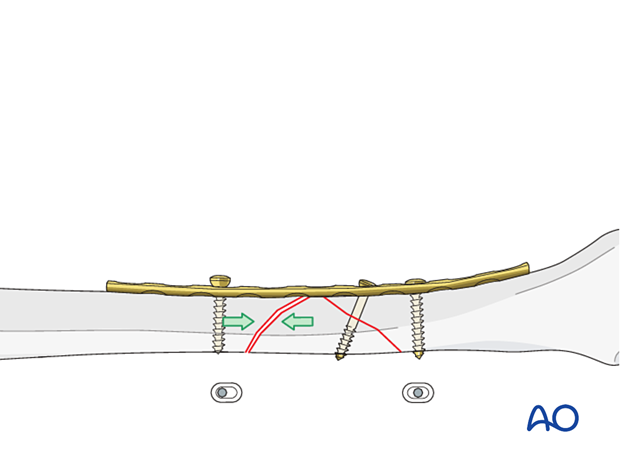
Dynamic compression principle
Compression of the fracture is usually obtained by eccentric screw placement at one or more of the dynamic compression plate holes. These holes are shaped like an inclined and transverse cylinder. The screw head slides down the inclined cylinder as it is tightened, forcing the plate to move along the bone, thereby compressing the fracture.
Before dynamic compression can be applied, the intact wedge must be fixed to one of the main fragments with a lag screw. Thus, an axilla is created which allows compression by eccentric screw insertion.
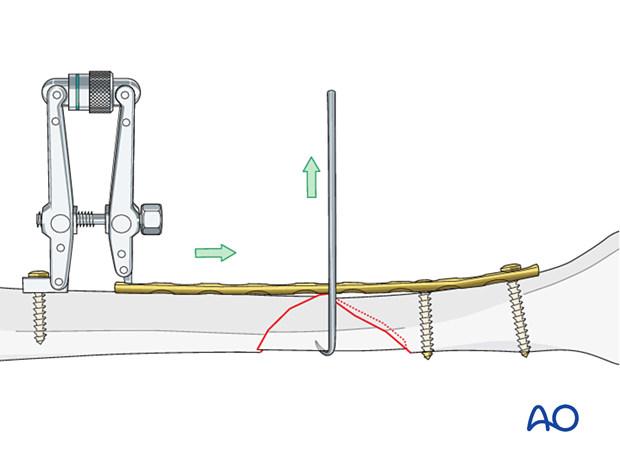
Using an articulated tension device
In wedge fractures, an articulated tension device (ATD) is more often used to gain length than for compression because of the limited compressibility of these fractures. If a push-pull screw is used, the same hole can be used to place the tensioning device.
2. Patient preparation and approaches
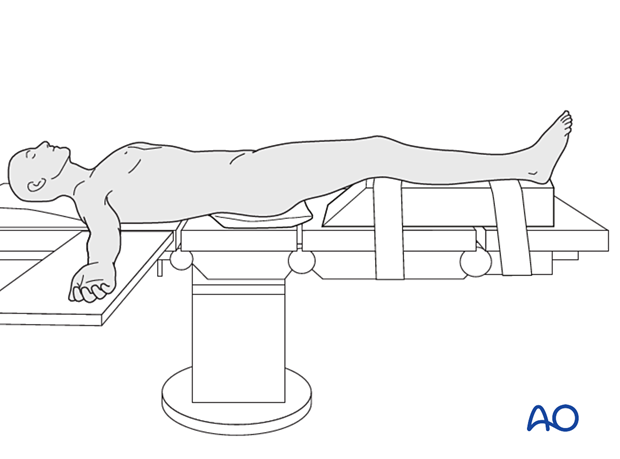
Patient preparation
This procedure is normally performed with the patient placed in a supine position on a radiolucent table or a standard operating table with a radiolucent extension. A pad is placed underneath the buttock to prevent external rotation.
A large foam bolster or cushion is placed under the affected leg to raise it above the opposite leg and facilitate lateral C-arm images.
Anteromedial approach
The anteromedial approach is used most commonly for fractures of the distal third of the tibial shaft. It can be used to expose the entire anteromedial surface.
It is also useful for debridement and irrigation of open fractures when an incision on the injured subcutaneous surface is to be avoided.
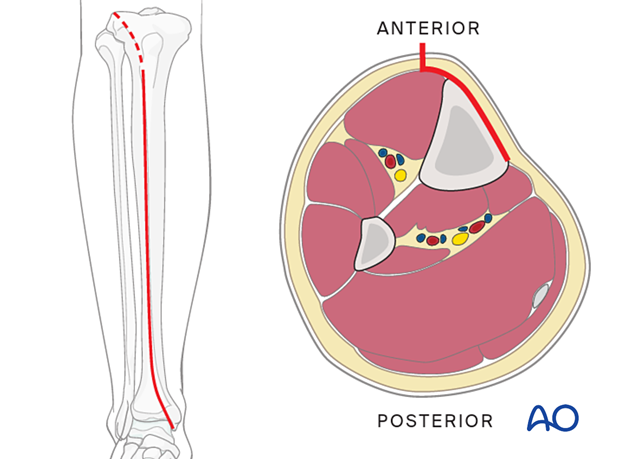
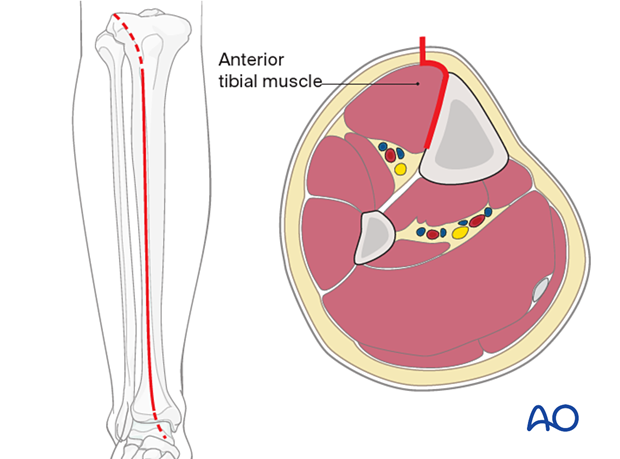
Anterolateral approach
The anterolateral approach is used uncommonly, but may be necessary when the medial soft tissues are compromised.
3. Plate preparation
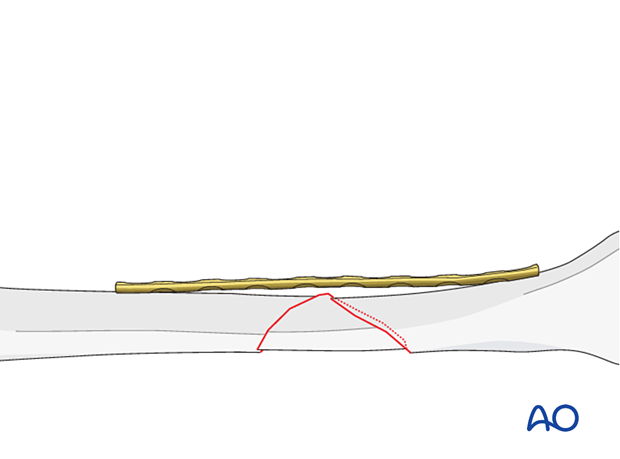
Overbending the plate
The plate should be overbent at the fracture site approximately 1–2 mm to ensure compression of the side opposite the plate.
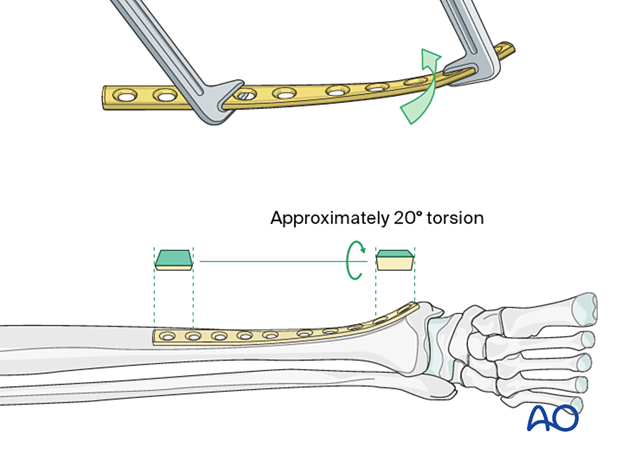
Twisting the plate
The anteromedial surface of the tibial shaft twists internally approximately 20° as it approaches the medial malleolus.
The first step of plate contouring is to twist the plate so it matches the tibial surface upon which it will lie.
If the plate is bent before it is twisted, the process of twisting will alter the bend that has been created.
Matching the curvature
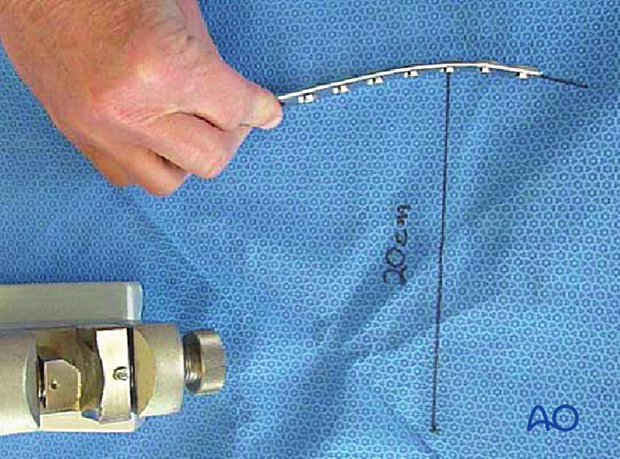
Depending upon the plate location, more or less bending of the plate will be required to match the contour of the intact (or reduced) bone. Much of the medial tibial shaft is quite straight so little bending is required. The distal medial surface has a significant concavity, with a typical radius of curvature of 20 cm, as illustrated.
A 20 cm radius can be drawn on a sterile drape and used as a template for plates to be used in this location.
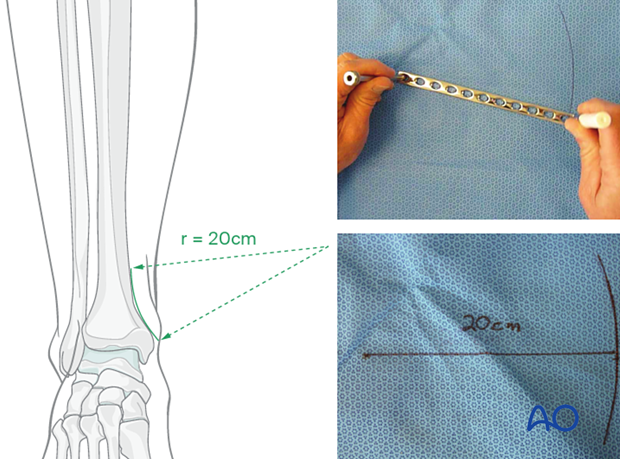
Bending the plate
The plate can be bent with bending irons alone, but bending with a bending press is preferable because it gives more control.
In either case, the bending is done in small steps to produce a smooth contour. Contouring only takes place over the distal 10–12 cm of the plate. When finished, the plate should match the 20 cm radius of curvature.
4. Reduction and fixation
Application of the plate
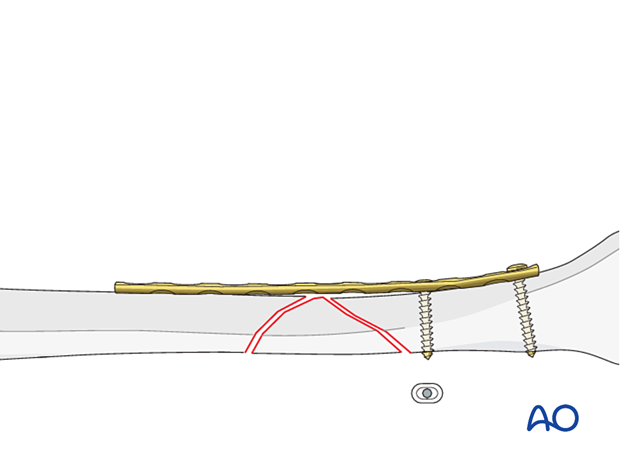
After contouring, the plate is fixed with two screws to the distal main fragment.
Reduction with the plate
If necessary, an ATD is applied proximally, and the fracture is distracted. The wedge fragment is gently reduced with a small hook.
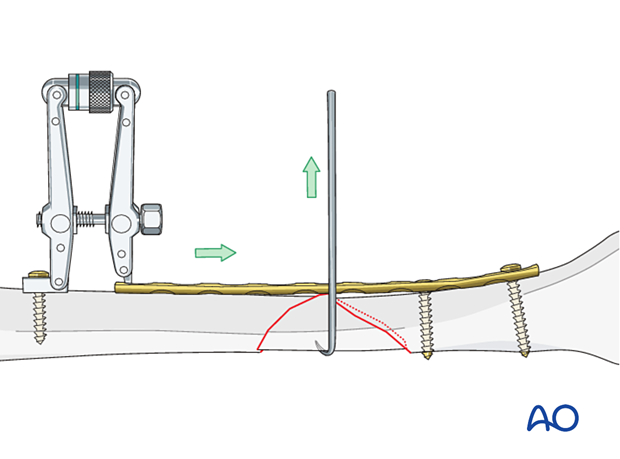
Lag screw
Depending on the fracture configuration, insert one lag screw through or outside the plate. With this lag screw, the wedge fragment is fixed to the distal main fragment.
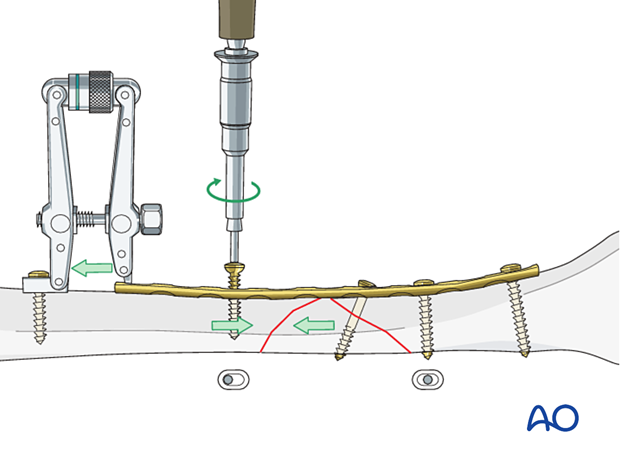
Dynamic compression
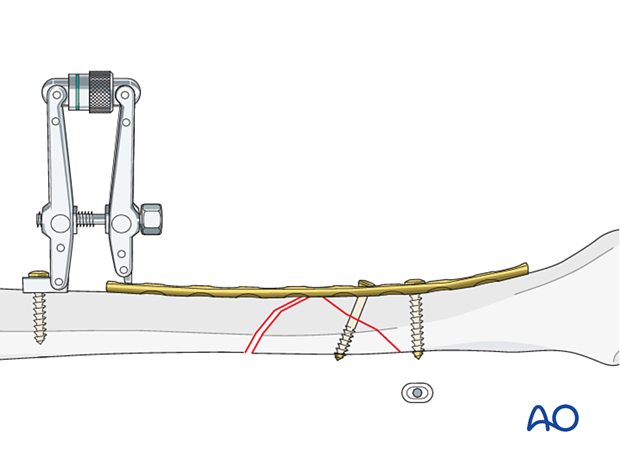
If an ATD has been used for preliminary reduction, compression can now be applied by converting the ATD from distractor to compressor. After compression of the fracture, insert a screw eccentrically into the proximal main fragment next to the fracture.
After reduction without an ATD, compression is achieved by inserting a screw in a maximally eccentric position (drilling without a protection sleeve).
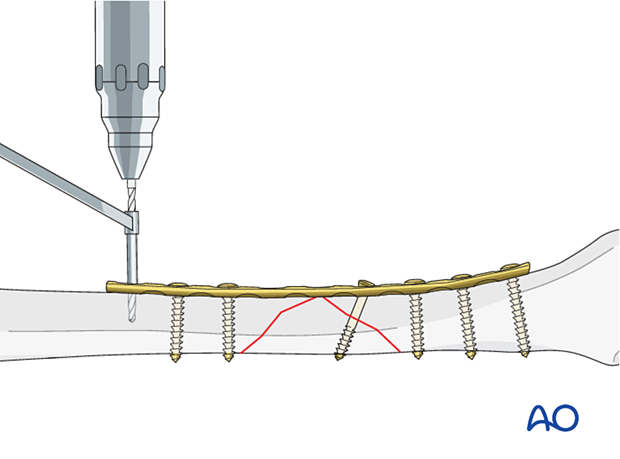
Screw insertion
The remaining screws are then inserted. Screws closest to the fracture site are placed first.
5. Aftercare
Perioperative antibiotics may be discontinued before 24 hours.
Attention is given to:
- Pain control
- Mobilization without early weight bearing
- Leg elevation in the presence of swelling
- Thromboembolic prophylaxis
- Early recognition of complications
Soft-tissue protection
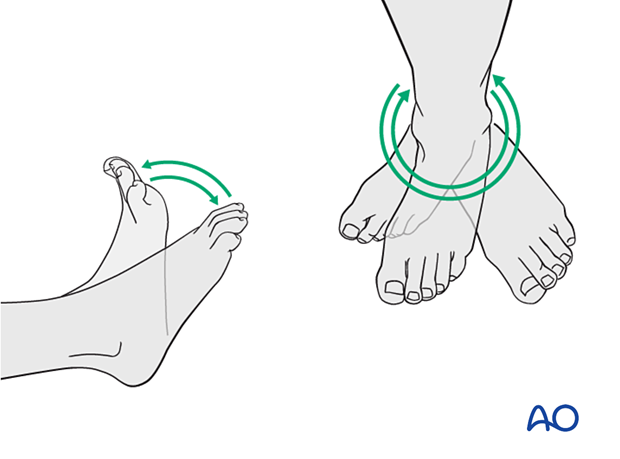
A brief period of splintage may be beneficial for protection of the soft tissues but should last no longer than 1–2 weeks. Thereafter, mobilization of the ankle and subtalar joints should be encouraged.
Mobilization
Active, active assisted, and passive motion of all joints (hip, knee, ankle, toes) may begin as soon as the patient is comfortable. Attempt to preserve passive dorsiflexion range of motion.
Weight bearing
For fractures treated with plating techniques, limited weight bearing (15 kg maximum), with crutches, may begin as tolerated, but full weight bearing should be avoided until fracture healing is more advanced (8–12 weeks).
For fractures treated with intramedullary nailing, weight bearing as tolerated, with crutches, may begin immediately.
Follow-up
Follow-up is recommended after 2, 6, and 12 weeks and every 6–12 weeks thereafter until radiographic healing and function are established. Weight bearing can be progressed after 6–8 weeks when x-rays have indicated that the fracture has shown signs of progressive healing.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation caused by the implants. The best time for implant removal is after complete bone remodeling, usually at least 12 months after surgery. This is to reduce the risk of refracture.













