Locking compression plate (LCP) fixation
1. Introduction
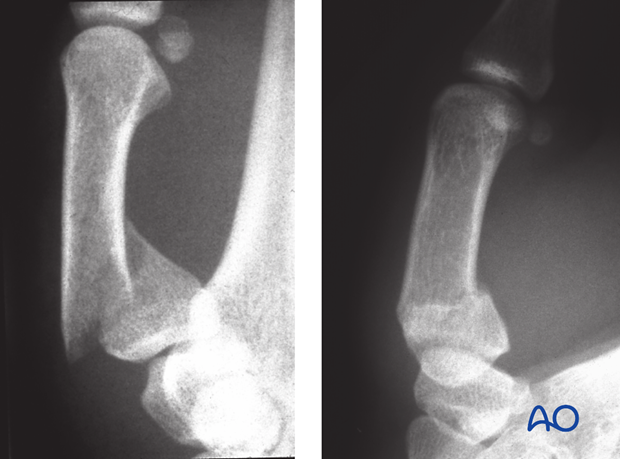
Extraarticular fractures of the base of the thumb metacarpal are often displaced, with a flexion deformity and may show palmar comminution (Winterstein fracture).
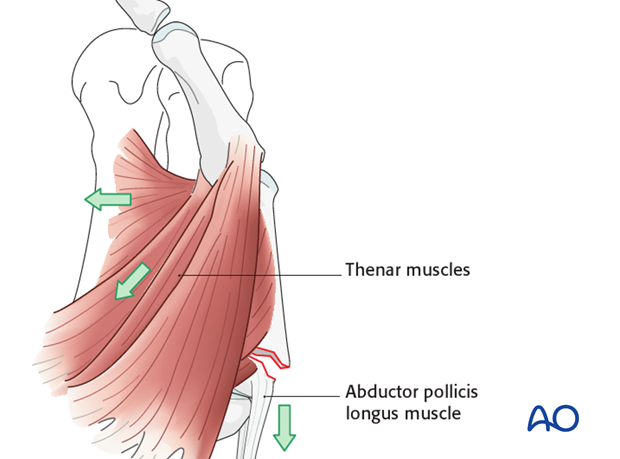
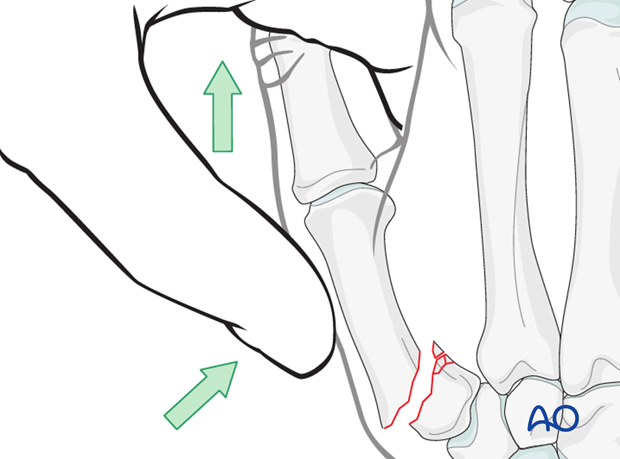
Displacement due to muscle forces
The pull of the thenar muscles results in palmar flexion of the distal fragment.
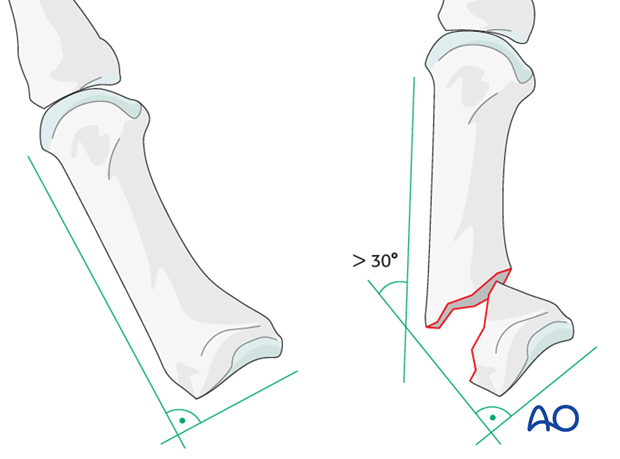
Flexion deformity
If the flexion deformity exceeds 30 degrees, thumb function may be impaired due to muscle imbalance. Internal fixation allows for anatomical reduction.
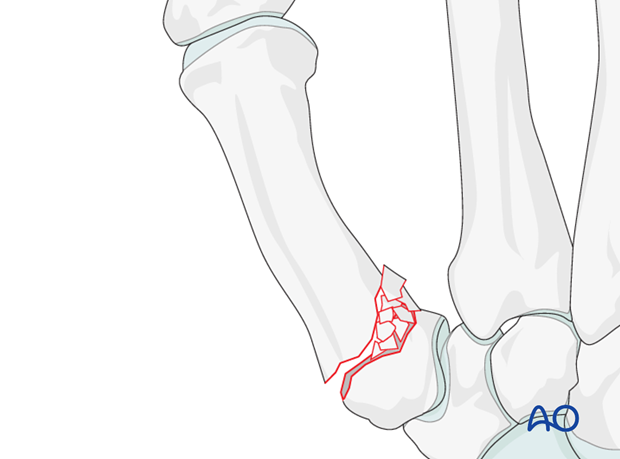
Instability due to palmar comminution
If standard plates are used, bone graft from the distal radius may be necessary to avoid delay in bone healing and consequent secondary displacement, or failure of fixation. Angularly stable plate fixation, using a locking compression plate (LCP), prevents secondary displacement without the need of bone grafting.
2. Approaches
For this procedure the following approaches may be used:
3. Reduction
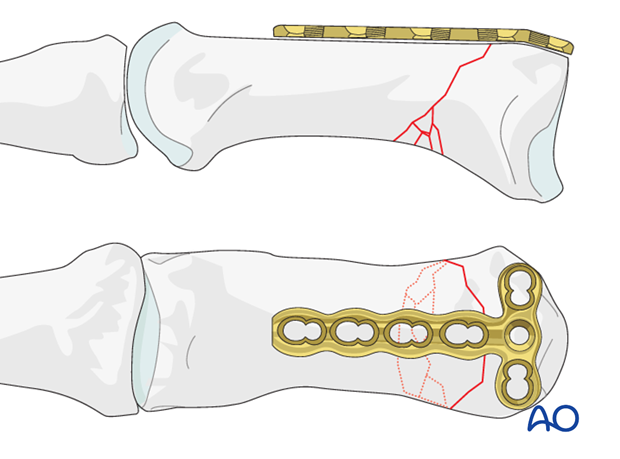
Indirect reduction with the plate
Angularly stable plate fixation in the proximal fragment allows for reduction using the plate as a lever (as described below).
Reduction by traction
Alternatively, and especially when a conventional plate is used, reduction can be performed with axial traction on the thumb, either manually, or with help of a finger trap, and simultaneous pressure on the dorsal aspect of the diaphysis.
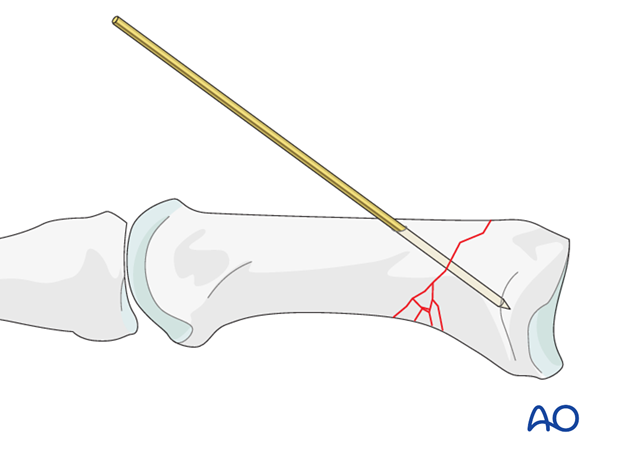
Preliminary stabilization
Preliminary stabilization can be achieved with an obliquely inserted K-wire.
If anatomical reduction is demonstrated using image intensification, a 2 mm LCP T-plate is fixed to the dorsal aspect of the first metacarpal using standard locking techniques.
4. Plate preparation
Plate length
Cut the 2.0 mm LCP to length so that 2 screws can be fixed in the distal diaphyseal fragment.
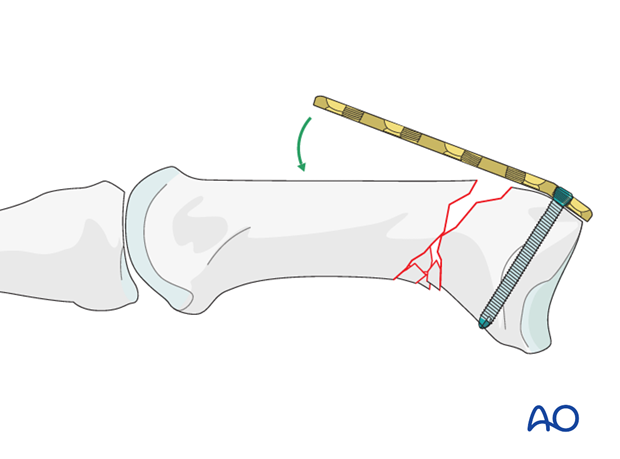
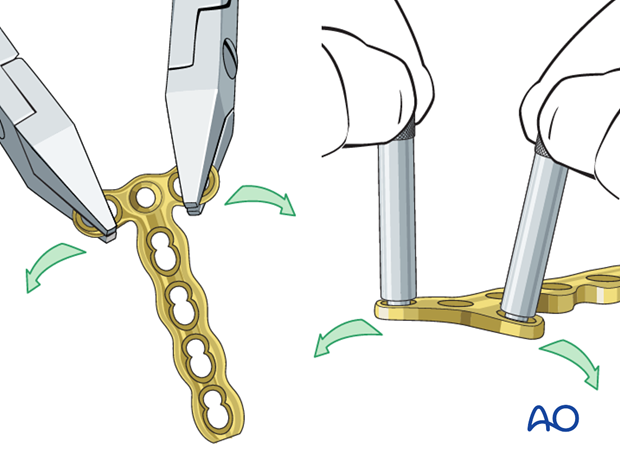
Contouring of the plate
The plate has to be adapted accurately to the contour of the proximal fragment. Use bending pliers to contour the plate. Be careful to bend in between the holes by positioning the pliers over the plate holes. Alternatively, insert the threaded bolt into the plate holes to bend the plate.
The bend should never go through a hole as this may damage the locking mechanism.
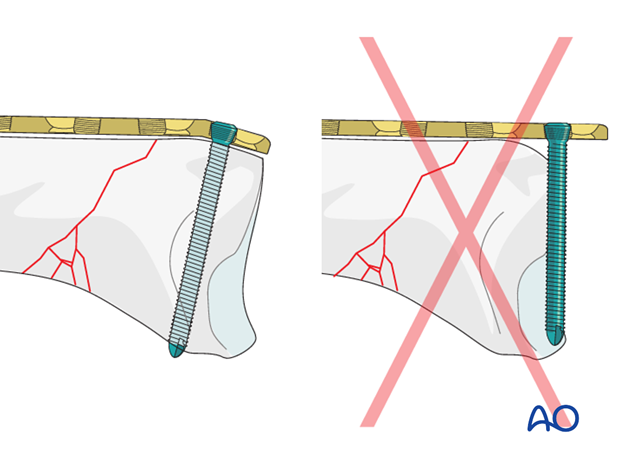
Adding a slight bend
In order to prevent the screw from penetrating the joint, a slight bend is necessary. Be careful not to overbend, as there is a comminuted zone at the opposite cortex, which can not withstand compression.
5. Plate fixation
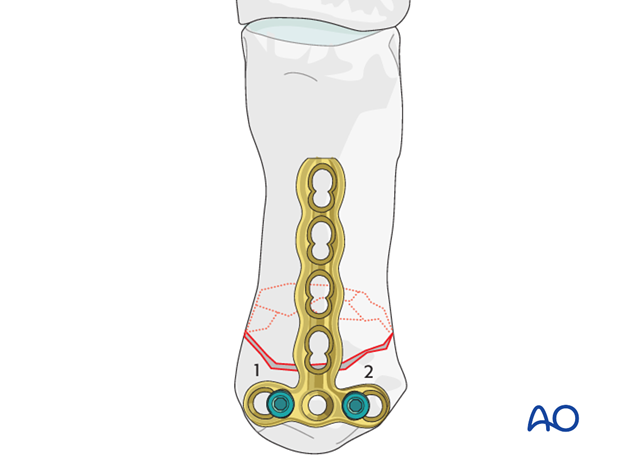
Insertion of first screw
Mark the plane of the first carpo-metacarpal joint with a thin K-wire or a hypodermic needle. Put the plate on the dorsal aspect of the proximal fragment, with a threaded drill guide in one of the outer holes. Drilling must be parallel to the marker wire (or needle) to ensure that the screw will not penetrate the joint. Confirm using image intensification.
Drill through the threaded drill guide. Remove the drill guide and measure the appropriate screw length with a depth gauge.
Insert the locking screw without completely tightening it.
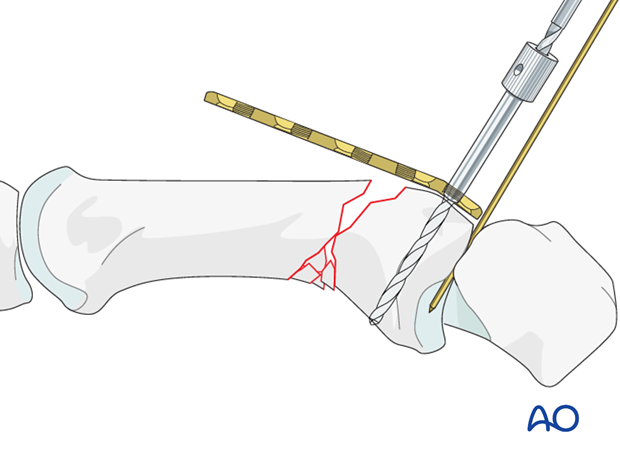
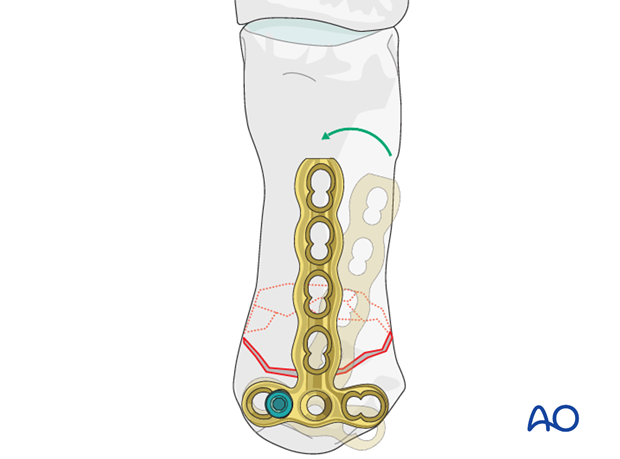
Plate alignment
Align the plate along the axis of the shaft.
Insertion of 2nd screw in the proximal fragment
Insert a second screw using the same technique. Always use a threaded drill guide when preparing for locking screws.
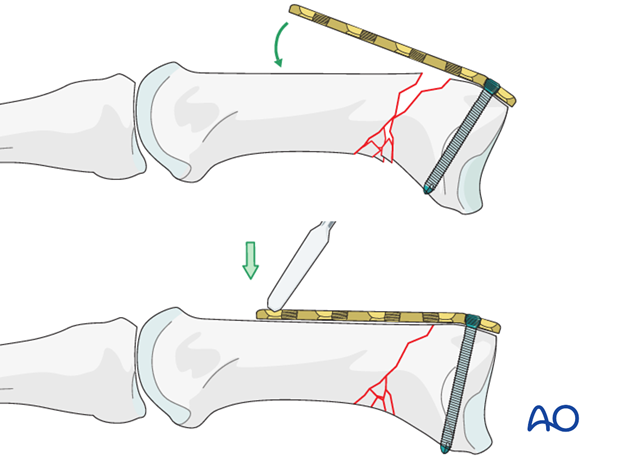
Reduction by using the plate as a lever
Pressing the plate down to the diaphyseal fragment with a periosteal elevator will automatically tilt the articular fragment into its correct position. Check the reduction of the dorsal fracture line.
Confirm using image intensification.
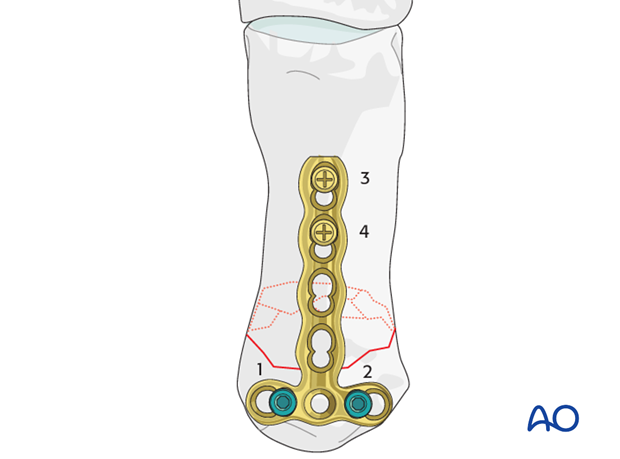
Insertion of distal screws
Insert a screw through the most distal plate hole. This screw would normally be a standard screw, as it engages in thick cortical bone. A locking screw, using a threaded drill guide when drilling, may be inserted in osteoporotic bone, or when otherwise indicated.
The second distal screw is inserted using the same technique.
6. Aftertreatment
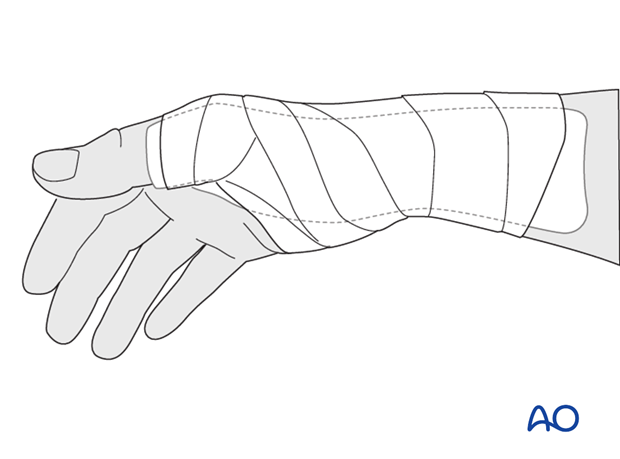
Splintage
Immediately postoperatively, a temporary plaster splint is applied which immobilizes the first MCP joint as well as the wrist. When the pain and swelling have reduced, a custom thermoplastic splint is applied for a period of time depending on patient comfort and fracture stability.The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesions’ restricting finger movement, tenolysis or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.
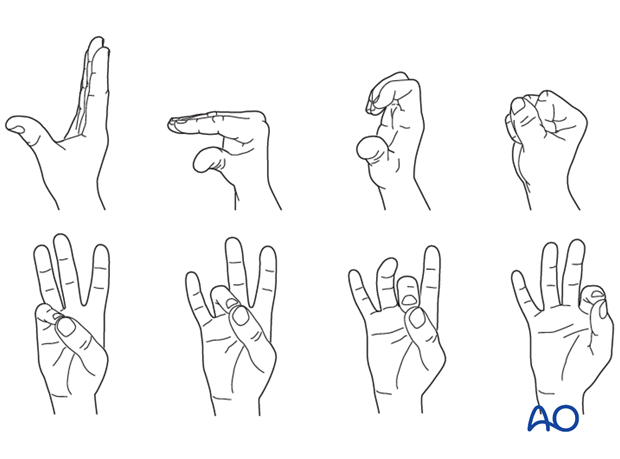
Functional exercises
In compliant patients with stable fixation, the splint can be removed under the supervision of a physical therapist, and early active motion exercises started after a few days.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness, or tendon adhesions’ restricting finger movement, tenolysis or arthrolysis become necessary. In these circumstances, take the opportunity to remove the implants.













