Radiopalmar approach to the base of the thumb
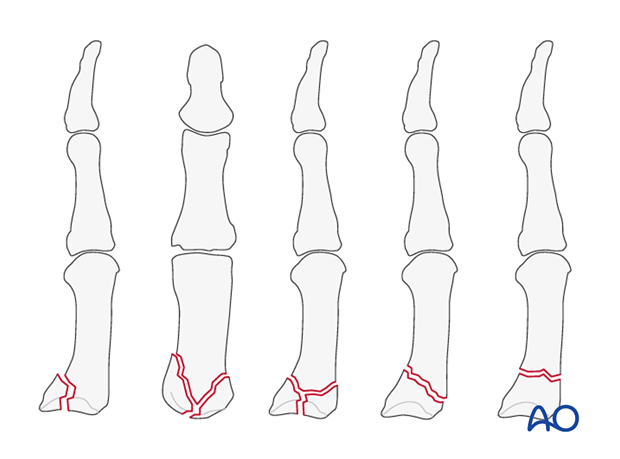
1. Indications
This approach is indicated for intraarticular fractures of the first carpo-metacarpal joint, such as the Bennett, or Rolando, injuries. It is also indicated for basal metacarpal, or trapezial fractures.
2. Surgical anatomy
The joint surfaces of the trapezium and thumb metacarpal resemble two reciprocally interlocking saddles.
This articular geometry, the ligamentous support system and the thumb muscles all work synergistically to enable opposition of the thumb to the fingers.
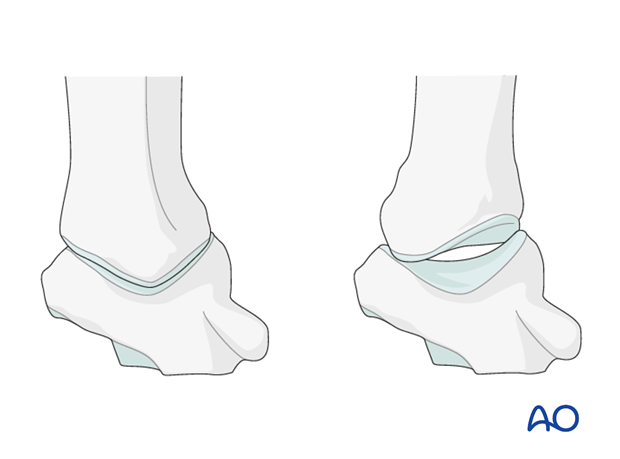
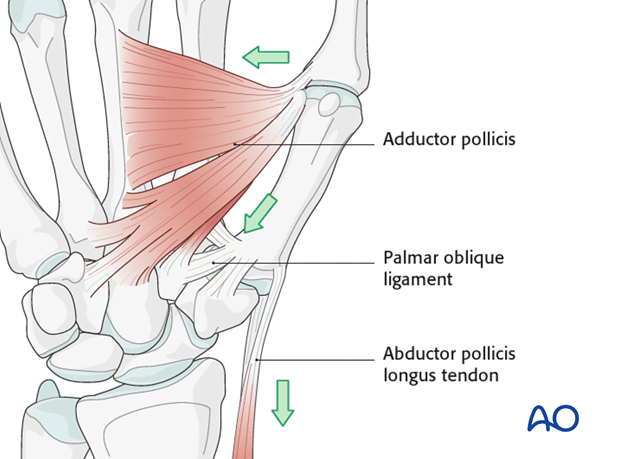
The strong volar oblique ligament is essential as a stabilizing unit of the base of the thumb metacarpal: it inserts into the articular margin of the volar beak on the ulnar aspect of the first metacarpal base.
On the radial side of the metacarpal base is the insertion of the abductor pollicis longus (APL) tendon.
The adductor pollicis exerts a force which pulls the thumb in a palmar and ulnar direction.
These opposing muscle forces create the typical deformity at the base of the thumb in Bennett’s fractures.
3. Skin incision
Two different skin incisions can be used:
The straight radiopalmar incision, and the curved incision, described by Wagner.
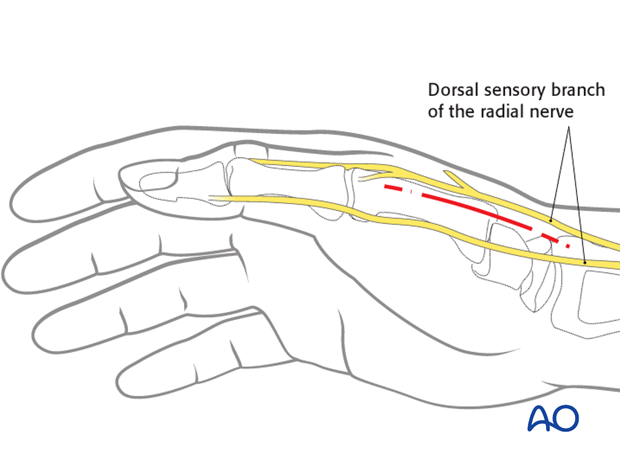
The straight incision is made in the dorsopalmar aspect of the thenar eminence at the transition between the dorsal and palmar skin. It starts about 1 cm distal to the tip of the radial styloid, extending distally for 4-5 cm.
The dorsal sensory branch of the radial nerve divides into several branches in this area. Identify and protect these branches to avoid troublesome neuroma formation.
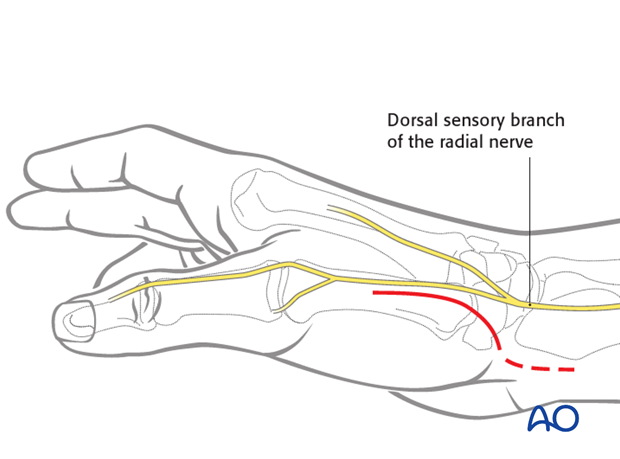
The Wagner incision follows the thenar eminence in a gentle curve towards its palmar aspect.
The disadvantage of this incision is the risk of scar formation across the wrist crease.
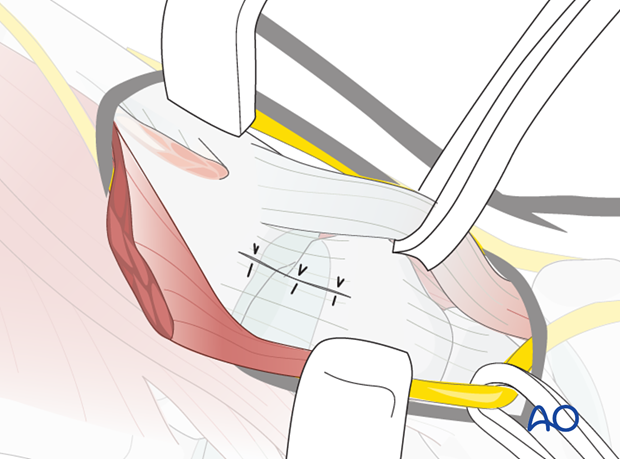
4. Elevate the flap
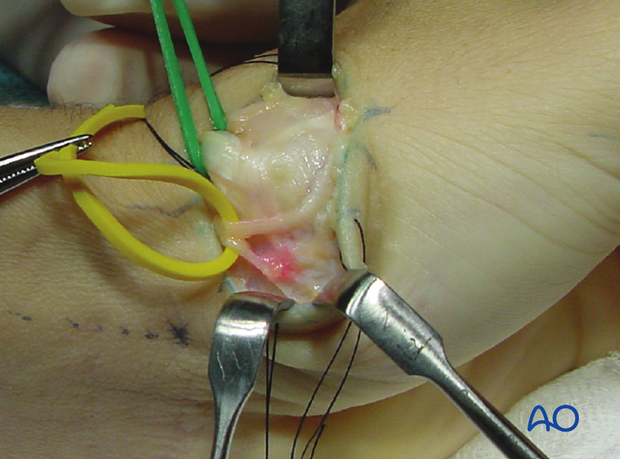
Elevate the flaps of skin and subcutaneous tissue by blunt dissection, identifying and protecting the divisions of the dorsal sensory branch of the radial nerve, and the APL tendon. Gentle retraction with elastic vessel loops aids the exposure.
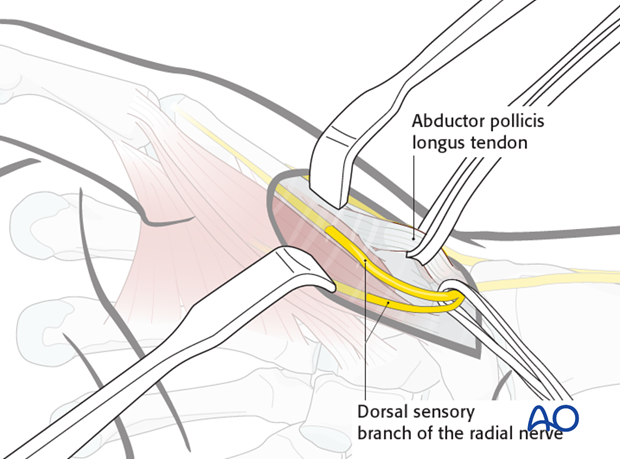
However, their excessive retraction can impair vascularity of the tissues.
5. Detach thenar muscles
After retracting these structures, the thenar muscles come into view. They are then detached from their origins at the base of the first metacarpal, and reflected in a palmar direction.
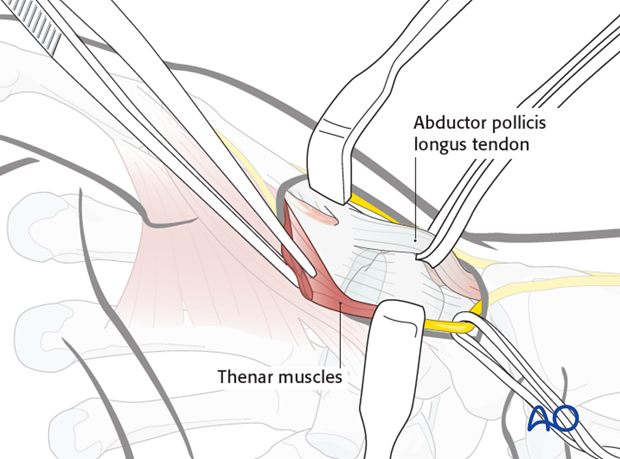
Preserving a small part of the insertion will later help with reattachment of the thenar muscles.
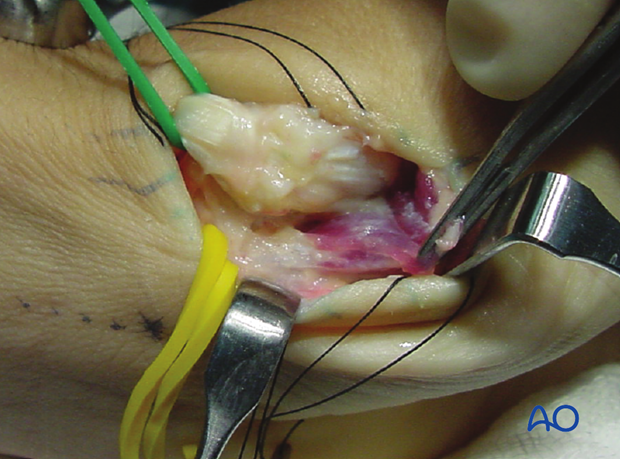
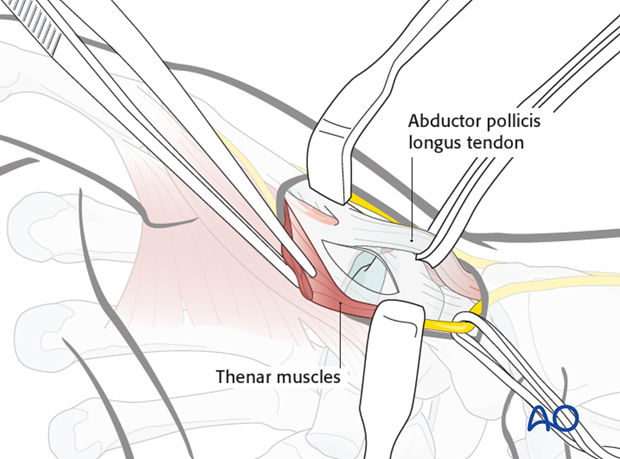
6. Capsulotomy
Perform a transverse or longitudinal capsulotomy in order to expose the joint.
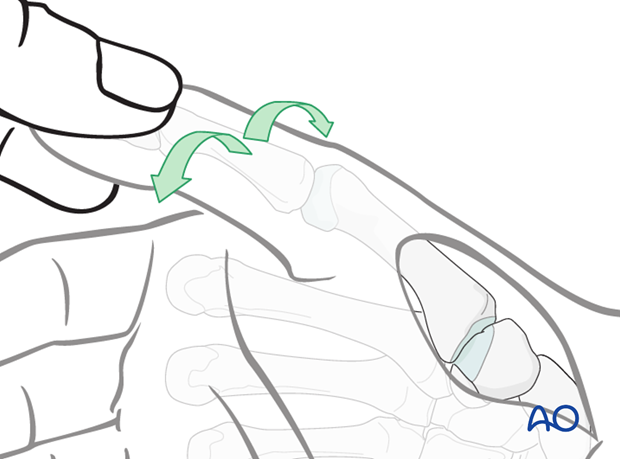
7. Inspect the joint
Inspect the joint by rotating the thumb into pronation and supination, whilst exerting longitudinal traction. This maneuver also helps to assess the fracture geometry, and to reduce Bennett’s fractures.
8. Wound closure
Close the capsule with interrupted sutures.
Reattach the thenar muscles to the base of the first metacarpal using interrupted sutures.