ORIF - Screw and plate fixation
1. Principles
Simple fractures
Simple osteochondral fractures of the talar body often are subtle and only discovered after a long history of ankle complaints.
CT scanning will uncover these injuries and their definitive treatment is no longer an urgent issue and can be provided as outpatient arthroscopic surgery.
High-energy fractures
The high energy necessary to produce fractures of the body of the talus is responsible for a spectrum of injuries including open fractures and irreducible fracture dislocations of the body.
Fractures of the body of the talus most often fail to be reduced by closed means, in part because the talus has very little soft tissue attached, and one can not use ligamentotaxis as an aid in reduction. Many of these injuries are open and require emergency treatment.

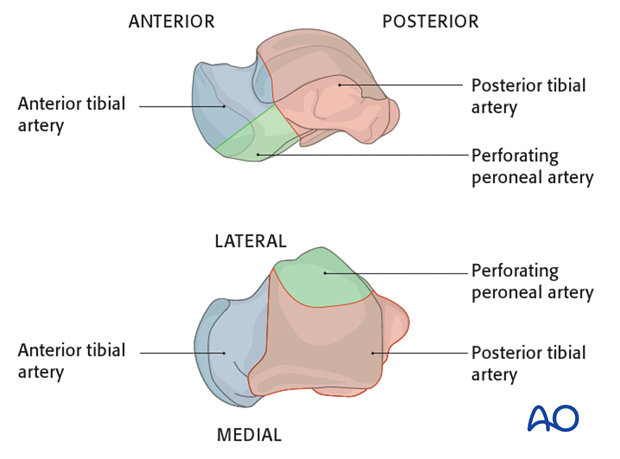
Anatomy
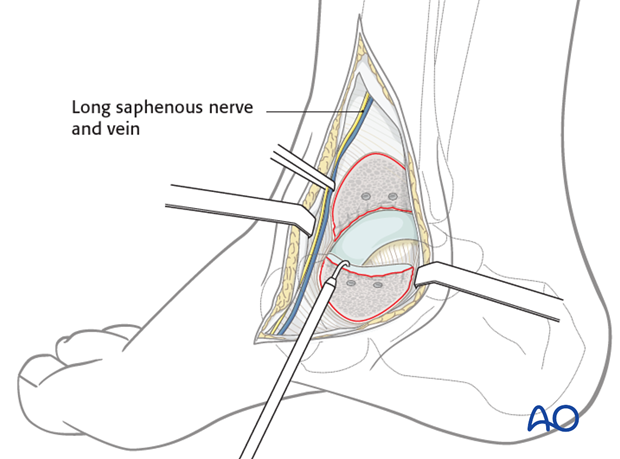
The blood supply to the talus is very compromised with a fracture dislocation scenario. The posterior tibial artery has branches medially. The dorsalis pedis has branches anteriorly. The peroneal artery has branches laterally. They are all connected through a sling of vessels that lie within the sinus tarsi.
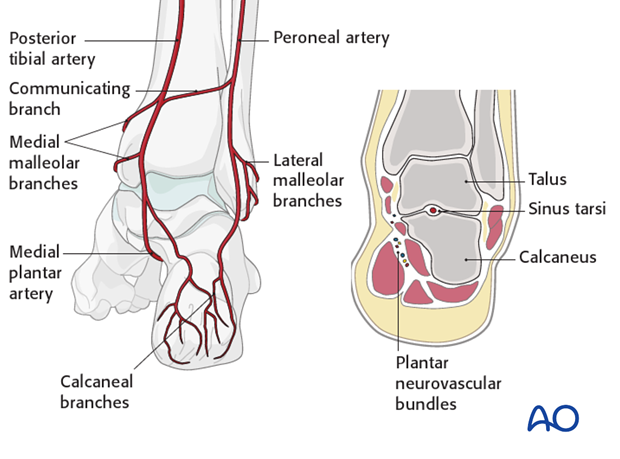
The deltoid branch of the posterior tibial artery must be protected. It is an important point for blood supply entry into the medial talus. This is the reason why a medial malleolar osteotomy is successful as it protects the talar blood supply.
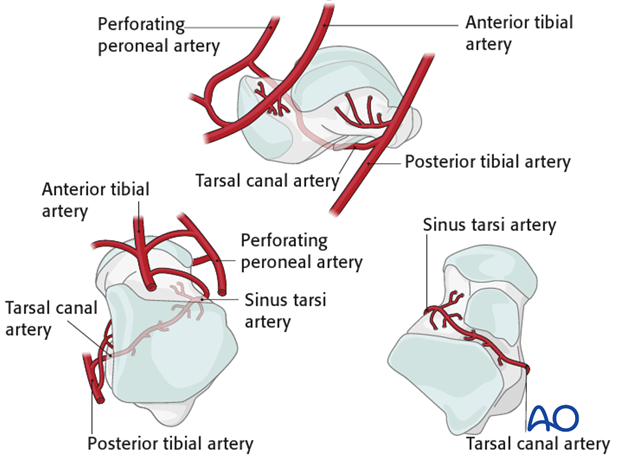
The deltoid branches are important to supply blood to the medial talar neck and talar body. Branches from the dorsalis pedis supply the talar head and most of the dorsal talar neck. The artery of the tarsal canal coming from branches off of the posterior tibial artery supply most of the talar body.
The peroneal artery has the least contribution laterally.
2. Emergency reduction
Emergency actions
The high-energy displaced fractures of the talar neck with, or without, dislocation of the talar body, often present with severe soft-tissue injuries, including open fractures, or both. To prevent further soft-tissue damage, urgent closed reduction is mandatory. Once that has been carried out, even only to the point of improving the position, if not completely reducing the fracture, one can begin preoperative planning of further and definitive care.
If a satisfactory reduction of the fragments can not be achieved, or if one is dealing with an open fracture, then an urgent operative intervention is mandatory.

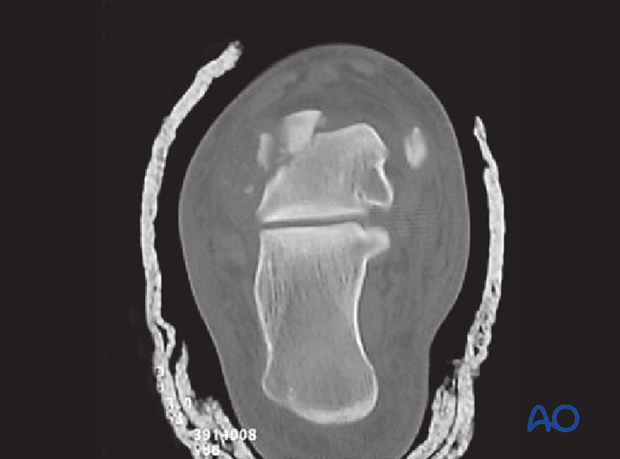
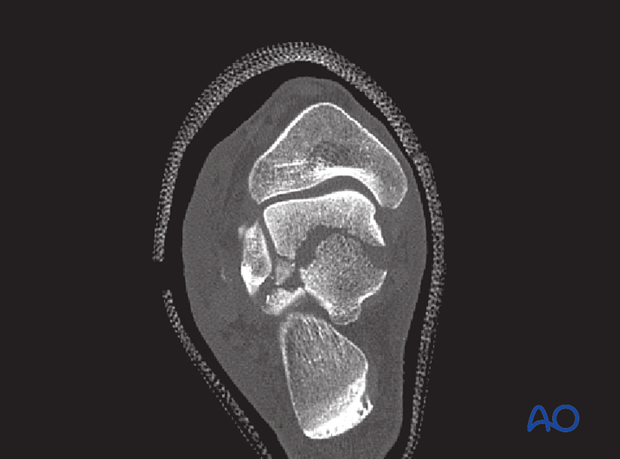
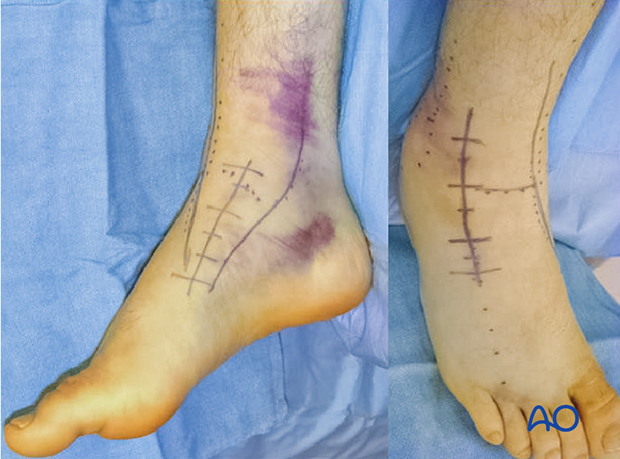
CT examination
This image demonstrates a severe talar body fracture with comminution that has been incompletely reduced.
Closed reduction has markedly helped the soft tissues that have been previously compromised.
CT examination is mandatory for preoperative planning when there is any question about understanding requirements for debridement, or reconstruction, of the subtalar joint. Along the spectrum of injury, increasing displacement presupposes that there is more subtalar and tibiotalar osteochondral injury. This often requires surgical approaches for debridement and fixation of these fracture types.
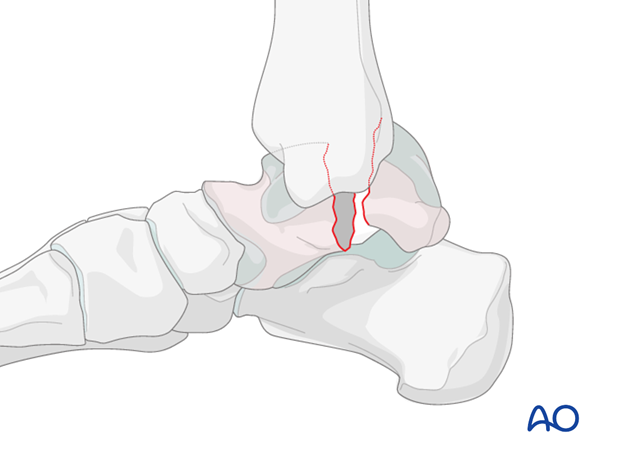
Closed reduction technique
When one looks at the foot it is obviously swollen and deformed. It is useful to look at the patient’s uninjured foot to determine individual anatomy.
The talar neck and a portion of the body will stay with the foot and tibia, yet the displaced fragment (which may be the body of the talus or part of it) will need reduction. This may present in a myriad of ways.
Plantar flexion and dorsiflexion of the ankle with traction may “pop” the displaced talar body back into its desired position.
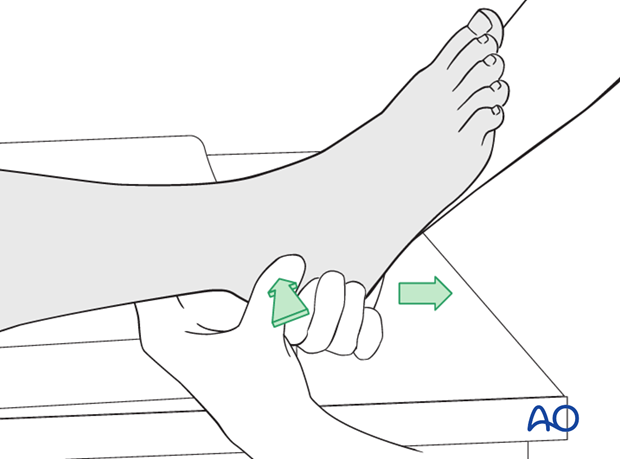
Traction
The reduction maneuver is facilitated by longitudinal traction and reversal of the force and its direction.
If successful, normal anatomy will be restored. The deforming force may have been a medially directed force, or laterally directed force, depending upon whether this is a medially or laterally displaced injury.
Usually, with talar body fractures, a successful reduction is accompanied by reestablishment of normal foot anatomy.
Splintage with follow-up radiology will now determine whether the closed reduction was successful.
Multiple attempts of closed reduction are not advised as they can further injure the soft tissue.
3. Choice of approach
The talar body injuries demonstrate a spectrum from simple two-part fractures to very comminuted multiply fragmented talar body injuries. The choice of approach can be made easier after radiology and CTs are completed. Sometimes, single approaches are appropriate, while other times combined approaches are needed.
As well, by extending the anteromedial or anterolateral approaches, ...
... osteotomies of medial malleolus or lateral malleolus can enhance exposure of the talar body to allow for accurate reduction of this difficult and hidden fracture.
Surgical experience helps in decision making when one is confronted with a difficult choice in selecting the appropriate surgical approach. One should always opt for a more comprehensive approach, rather than one which will limit visualization, or lead to excessive soft-tissue retraction.
4. Open reduction
Introduction
Virtually all fractures of the body of the talus will require open reduction. Careful preoperative planning is necessary. The talus is integral to the normal function of the hindfoot and one must attempt to achieve an anatomic reduction. This means that an open reduction is unavoidable.
After debridement of open wounds, if present, and reducing, or attempting to reduce, dislocations and major displacement, one moves to very early emergency management of these injuries, including open reductions.

Open manipulation
Care should be taken to preserve all soft-tissue attachments (blood supply) to the talar body.
Two approaches should be used.
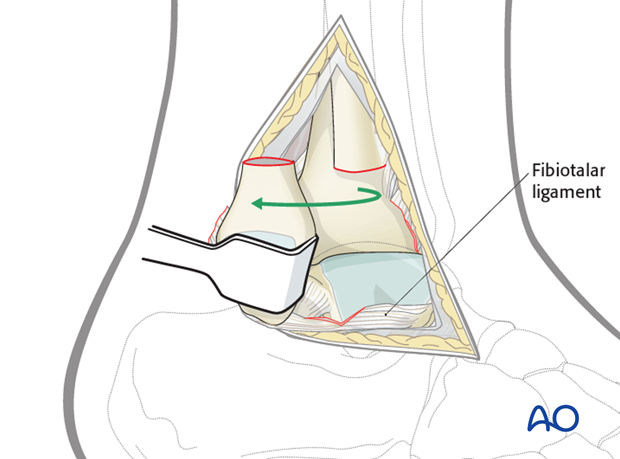
When the combined approaches are used and the reduction can not be obtained, then there is a series of steps for successfully obtaining the reduction.
Firstly, elevators and joysticks are advised, followed by the use of external fixators and distractors.
Lastly, the medial malleolar osteotomy would be performed as the most invasive, yet most definitive, tool.
Image intensification would be used at every step.

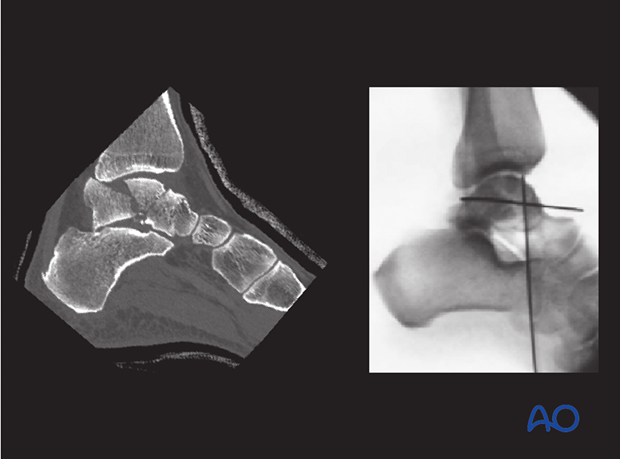
The images demonstrate a talar body fracture preoperatively that was irreducible by closed means. Intraoperatively, medial malleolar osteotomy and joysticks were necessary for successful open reduction.
5. Fixation
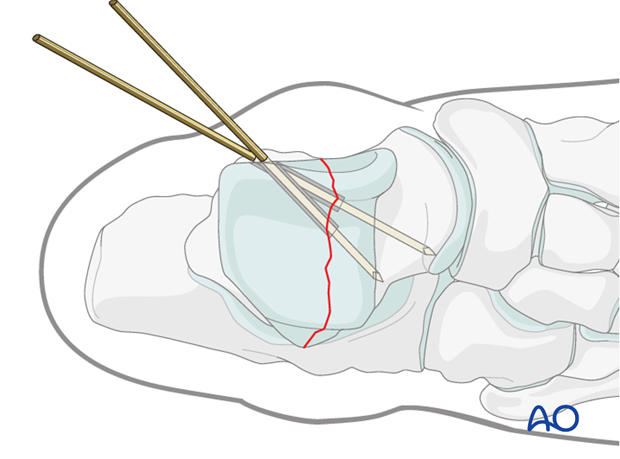
Preliminary fixation
Preliminary fixation is achieved with K-wires. It is advantageous to use the guide wires for cannulated screws and place them in such a way that they can be subsequently used as guides for definitive cannulated screw fixation. Occasionally, lag screws alone, if the fragments are large, will suffice in securing stable fixation of fractures of the body.
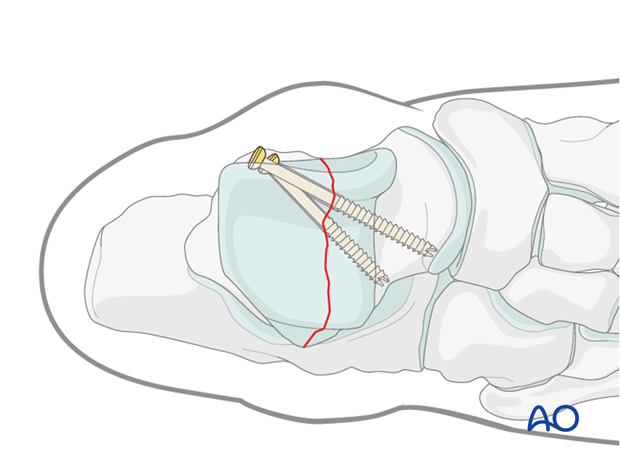
Definitive fixation
Each talar body injury is different and requires individual preoperative planning in order to achieve an open reduction and then stable fixation. Screws alone, or plates and screws, can each be used. The talar body is virtually completely covered by cartilage, such that plate fixation is difficult but possible with careful planning. When screws are used, they must be countersunk beneath the level of weight-bearing articular surfaces. Medial, or lateral, osteotomies allow visualization and access for proximal body, or comminuted talar body, injuries.
Retrieval, or removal, of hardware is not planned.

Pearl
Biomechanical studies have shown that posterior to anterior screws are the strongest construct. With a large posterior body fracture, where possible, posterior to anterior screws are recommended. Two screws of 3.5 mm or 4.0 mm are recommended.
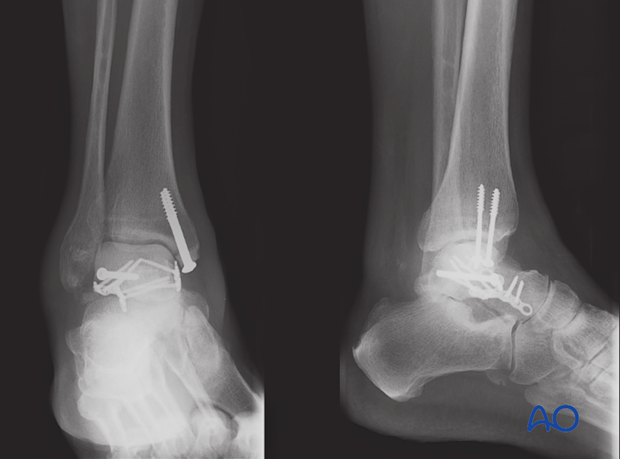
6. Complication: avascular necrosis
This case shows three-month follow-up x-rays with the most common complication of talar body injury, that being avascular necrosis. The talar body is noted to be sclerotic and much more radio-opaque than the surrounding bone at 12 weeks. The medial malleolar osteotomy is healing.
Despite this radiograph, symptomatology was benign and the patient had good range of motion, therefore weight bearing was initiated.
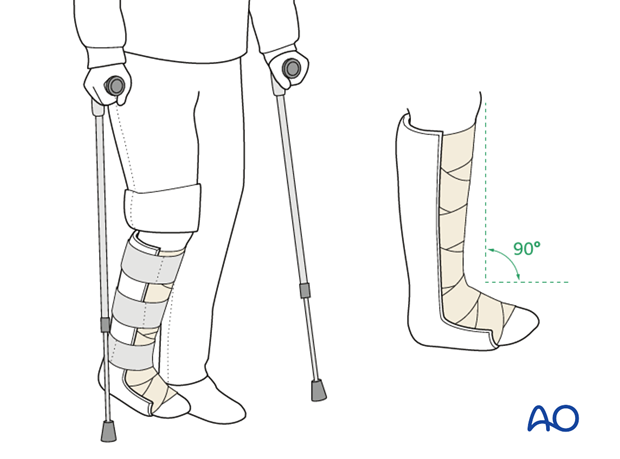
7. Aftertreatment
After surgery, a posterior splint with the foot in neutral position is applied. Early range of motion of the ankle and subtalar joint is advised.
Weight bearing should be restricted for 12 weeks with follow-up occurring at 2, 6, 12 and 24 weeks, and more, if necessary.
Range-of-motion exercises are important to commence as soon as they are tolerated.
Radiography at 12 weeks will confirm healing and will also indicate whether Hawkins’ sign is present (good prognosis), or not.
Once healing has occurred, and if there is no evidence of avascular necrosis, weight bearing and gait training rehabilitation can begin.
Patients with talar body fractures should have no pain and improving range of motion before starting full weight bearing.