ORIF - Plate fixation
1. Introduction
Principle
In this procedure it is important to anatomically reconstruct the joint surface, and thereby convert the complete articular fracture type to an extra-articular fracture type.
The joint block is then reduced to the scapular body.
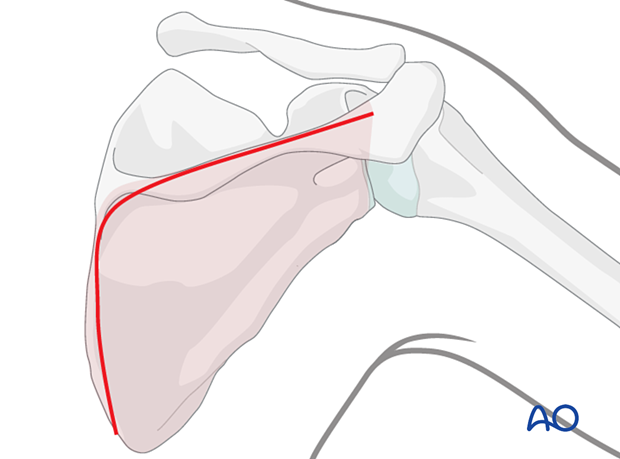
One must restore the correct anatomical angle between the glenoid fossa and the scapular body.
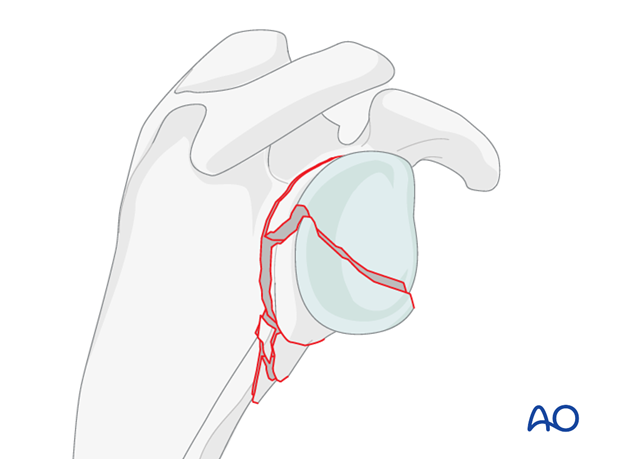
Plate selection
The standard plate for this fixation is the 2.7 or a 3.5 reconstruction plate. The plate will be used to bridge the comminution.
The plate should be long enough to allow placement of 3 screws in the lateral border of the scapula.
2. Patient preparation
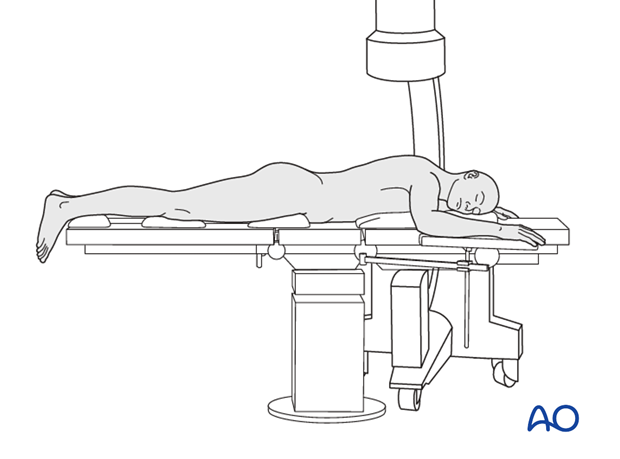
This procedure may be performed with the patient in either a prone position or lateral decubitus position.
3. Approach
Plating of the glenoid neck and scapula are performed through a posterior approach.
In a complete articular fracture with an anterior fragment a posterior arthrotomy is necessary to reduce the fragment. Its fixation is achieved with a lag screw inserted posteriorly.
4. Restoration of articular surface
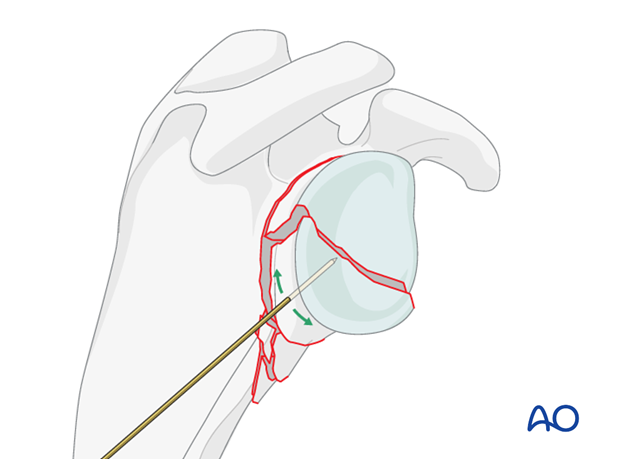
Reduction of the joint surface using K-wires
Reduction of the articular surface may be facilitated by the insertion of a K-wire to be used as joystick. The use of a cannulated system is preferred. Therefore, insert the K-wire for the potential cannulated screw in the planned lag screw trajectory.
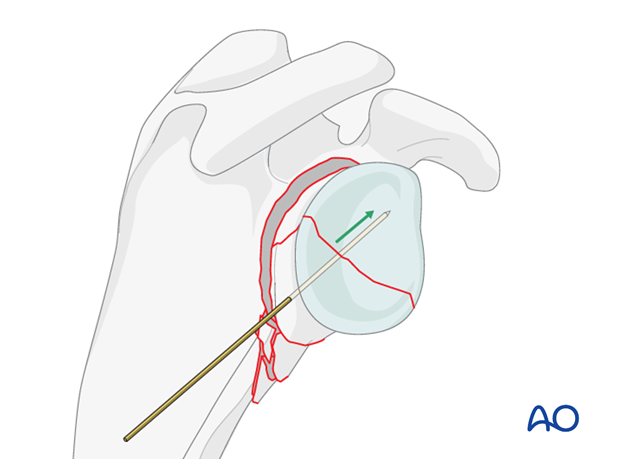
When reduction of the articular surface is completed, insert the K-wire further to temporarily fix the articular fracture.
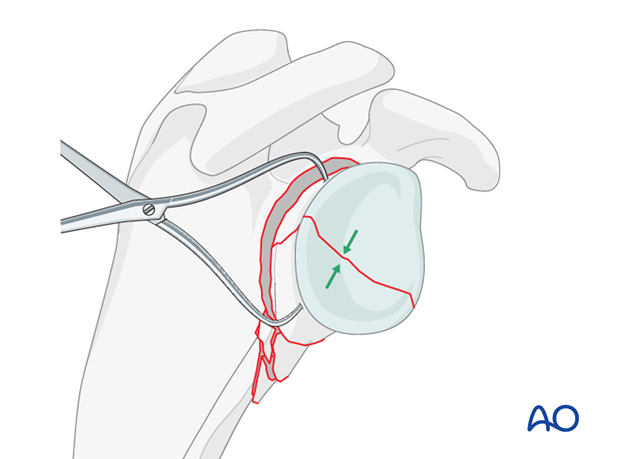
Alternatively, a repositioning clamp can be used to reduce the fragments of the glenoid fossa.
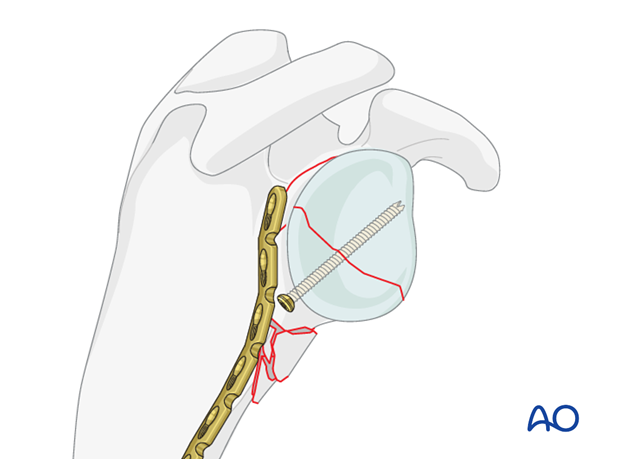
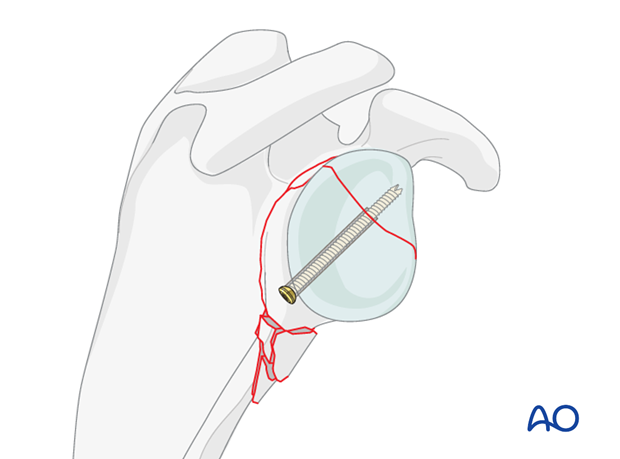
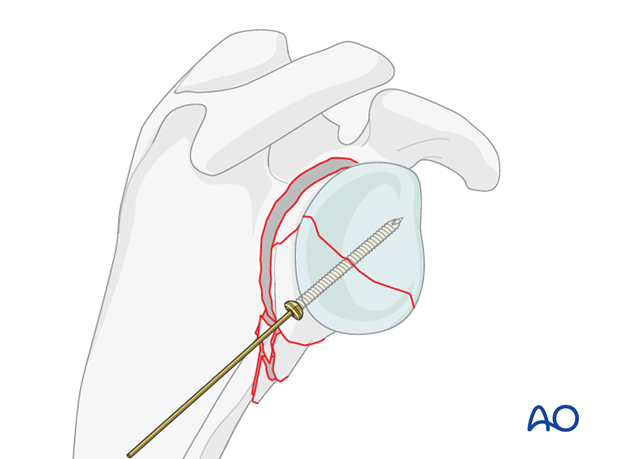
If possible, the fracture of the glenoid fossa should be fixed with a lag screw(s).
Once the articular fracture is fixed, proceed with the fixation of the neck as for multifragmentary extra articular fractures.
5. Reduction and fixation
It is best to use a reconstruction plate designed to take angularly stable screws.
The plate is bent at the right spot to subtend the usual angle between the glenoid and the lateral border of the scapula (130 - 135 degrees).
Up to 10 degrees deviation from the anatomically correct angle can be tolerated.
When angularly stable fixation is used the plate does not have to fit the bone, but must fit the overall contour.
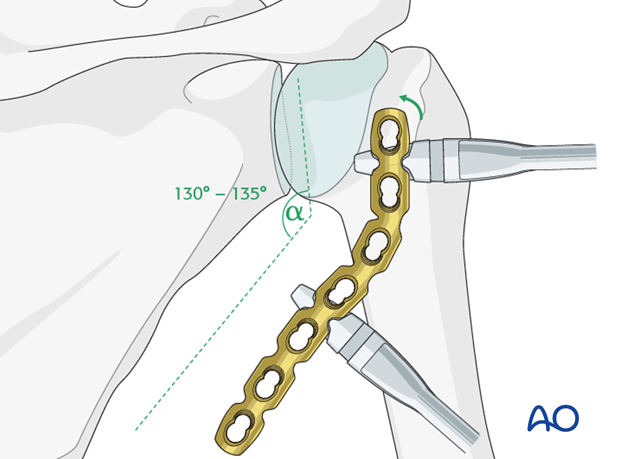
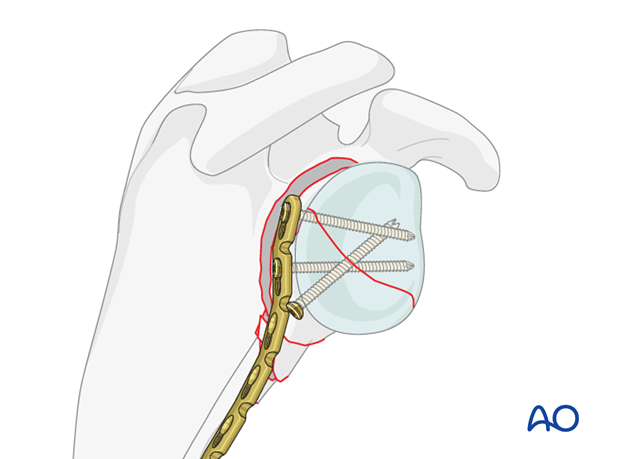
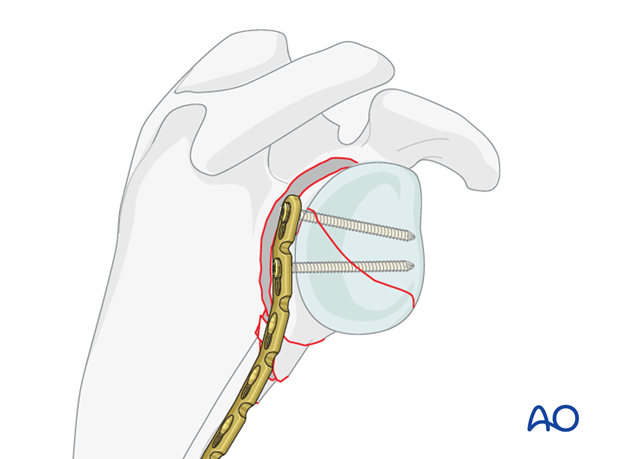
The plate is fixed to the glenoid segment with two bicortical screws.
If locking screws are used, care must be taken regarding their direction so that they do not enter the joint.
In a transverse fracture of the glenoid where lag screw fixation is physically not possible, maintain reduction and compression of the fracture with a clamp, then reduce the neck fracture.
The reduction and compression of the articular fracture is then maintained by the fixation of the plate to the articular segment.
The plate is then used as a reduction aid.
A trasglenoid X-ray is recorded to verify whether the anatomical angle is achieved.
Large deviations of the angle (>20°) will reduce the functional outcome.
When the correct reduction and the correct angle between the glenoid fossa and the lateral border of the scapula have been achieved, screws are inserted along the lateral border of the scapula.
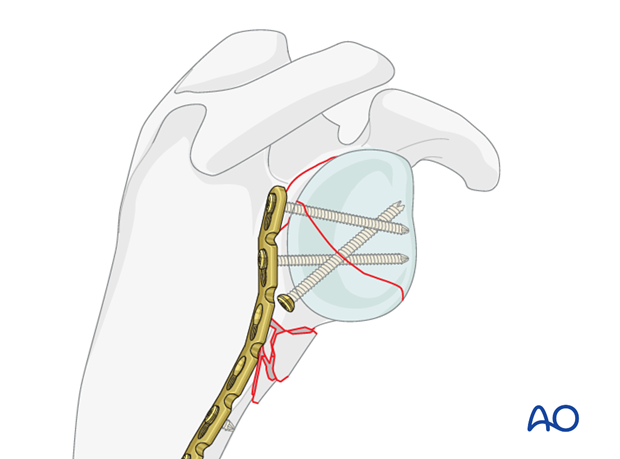
Correct reduction and fixation is verified by image intensification.
6. Aftercare
The aftercare can be divided into 4 phases:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.













