Postoperative treatment of scapula fractures
1. Phase 1: injury to the end of week 3 after injury (inflammatory phase)
Phase 1 principle: protection of the injured (operated) limb to facilitate uneventful healing.
Phase 1 aim: healing without complications while facilitating early movement.
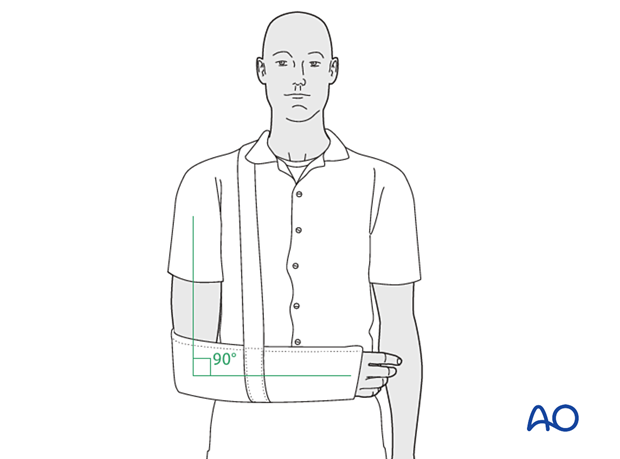
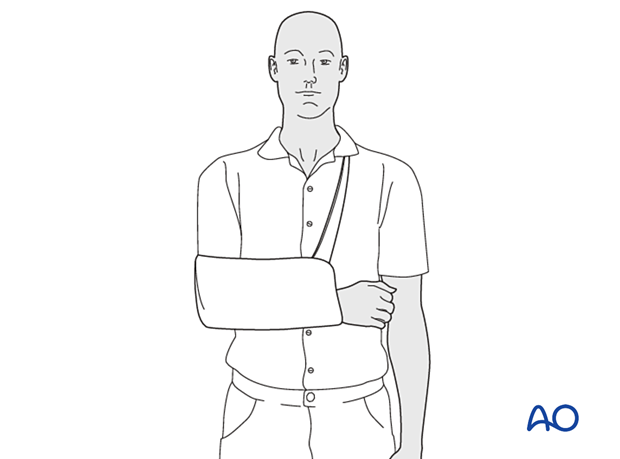
External support - full time
Optimal shoulder immobilization is achieved when the upper arm and forearm are secured to the chest. Traditionally, this has been done with a sling that supports the elbow and forearm and counteracts the arm's weight. The simplest sling is a triangular bandage tied behind the neck.
Additional support is provided by a swath that wraps around the humerus and the chest to restrict further shoulder motion and keep the arm securely in the sling.
Commercially available devices provide similar immobilization, with or without the circumferential support of a swath.
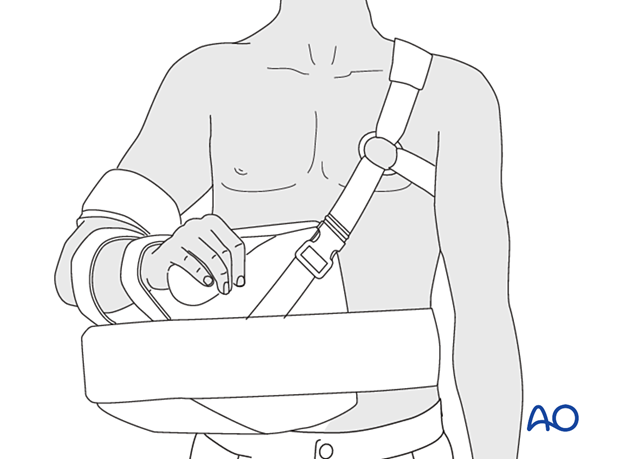
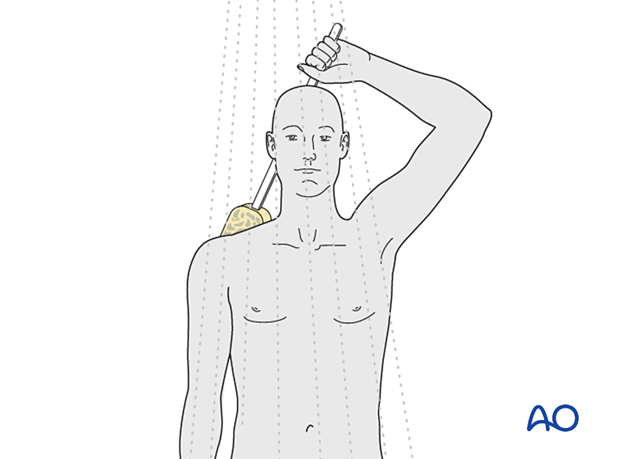
Abduction brace
In the case of coracoid fractures or acromial fractures and rotator cuff surgery, one attempts to relieve tension by elevation and abduction of the extremity. This can be achieved with the aid of a so-called airplane splint or an abduction cushion, as shown in this diagram.
Mobilization of the upper extremity for general indications
It is essential to maintain optimal mobility of the unaffected joints to reduce arm swelling by encouraging venous return and lymphatic drainage. Active mobilization of the unaffected joints promotes the preservation of the proprioception and therefore promotes optimal joint motion.
The following exercises are recommended.
- Opening and closure of the hand
- Squeezing of a soft ball
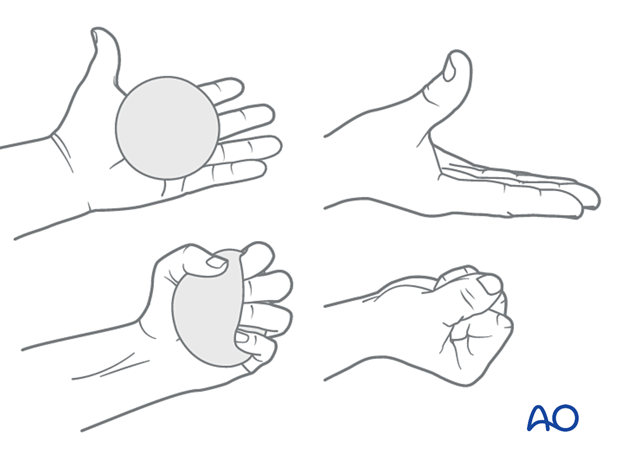
- Bending of the wrist forward, backwards and in a circular motion.
- Movement of an open hand from side to side

- Straightening and bending of the elbow
- Squeezing the shoulder blades together while the shoulders remain relaxed
- Gentle side-to-side, forward-and-backward, and rotational movements of the neck

Mobilization of ipsilateral limb kinetic chain with no active motion of clavicle-scapula
Physical therapy instruction and supervision may be helpful for optimal rehabilitation or if the patient is not progressing satisfactorily.
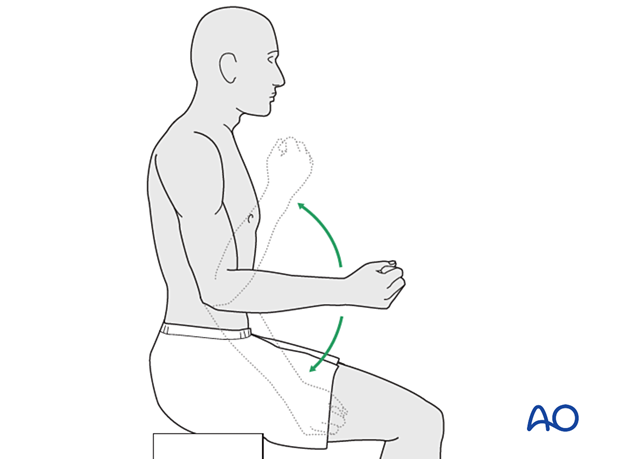
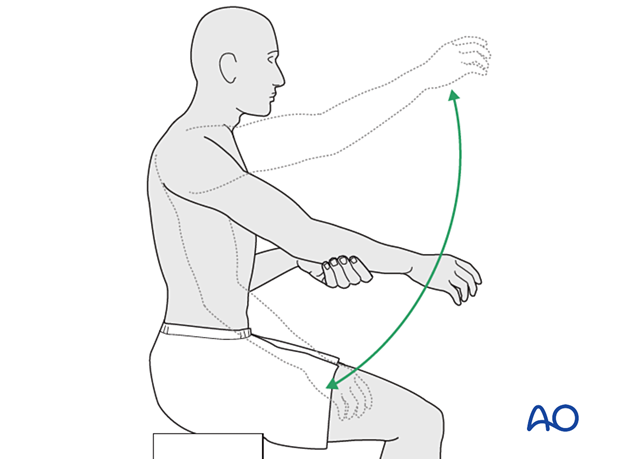
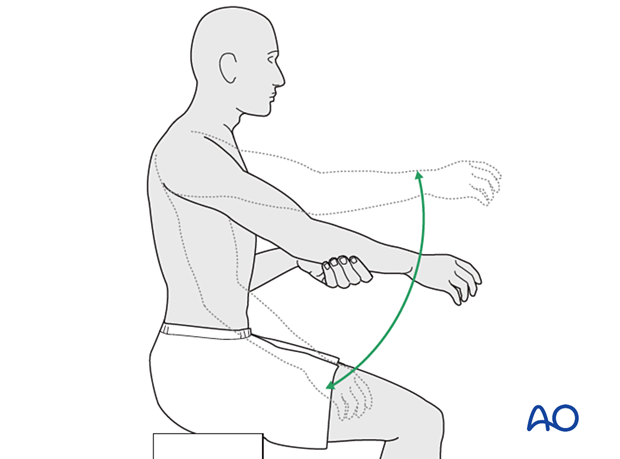
Active assisted range of motion exercises are started with gravity eliminated and as comfort permits:
- External rotation at waist level
- Internal rotation at waist level
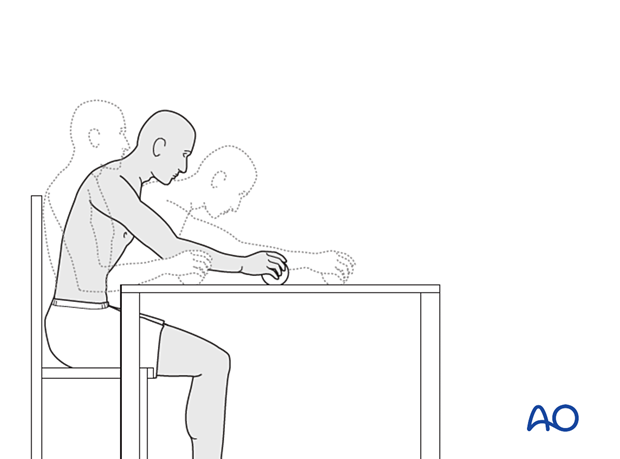
- Forward flexion without scapular protraction with the forearm supported by the table (illustrated)
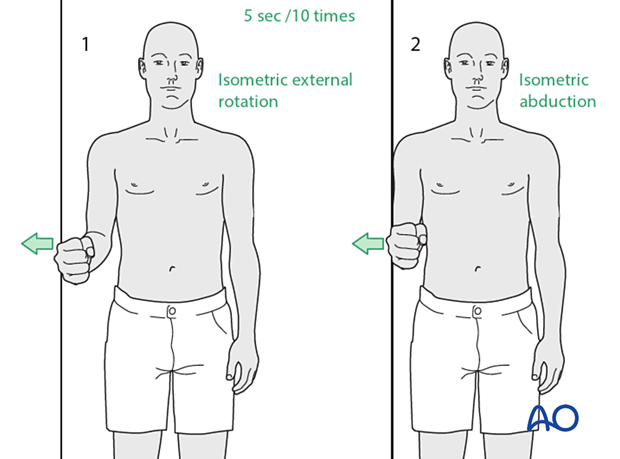
- Isometric strengthening of the rotator cuff and deltoid as comfort permits
X-rays should be checked to rule out secondary fracture displacement if unexpected pain occurs.
Activities of daily living
At this stage, activities of daily living are limited to those needed to do personal care.
The patient is encouraged to use the ipsilateral hand for midline personal care activities (eg eating and toileting).
Care should be taken when motions approach extremes of range, and taking the hand behind the back may not be safe until fracture union has been confirmed (by radiographs and the absence of fracture-site pain).

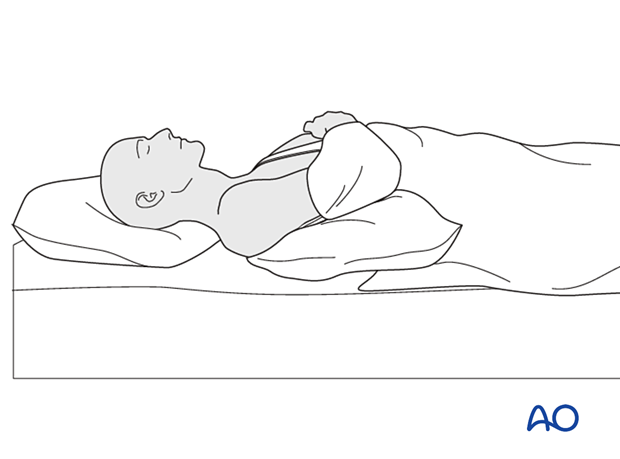
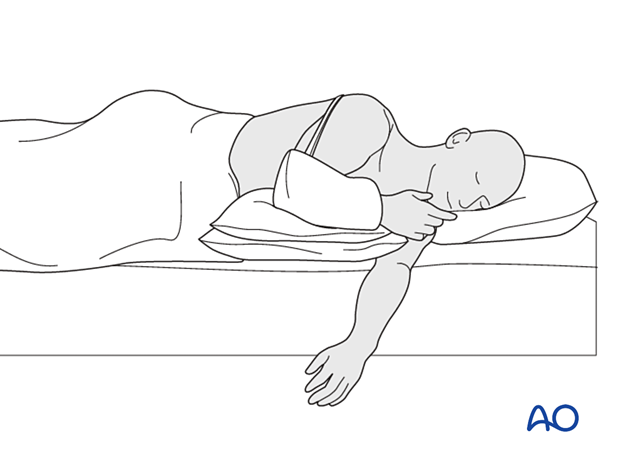
The patient should sleep wearing the sling and lie either on his back or on the non-injured side.
When sleeping on the back, the injured side should be supported by placing a pillow underneath the arm and shoulder.
Some patients may find it more comfortable to sleep in a sitting or semireclined position.
A pillow can be placed across the chest to support the injured side when sleeping on the side.
A non-slip mat in the shower/bathtub will improve safety. The arm can hang gently at the patient's side while showering. Axillary hygiene is important. If assistance is not available, a long-handled sponge can be used to wash the back and legs.
2. Phase 2: Beginning of week 4 to end of week 6 after injury (early repair phase)
Phase 2 principle: continued protection of the injured (operated) limb with the promotion of directed tissue repair.
Phase 2 aim: established healing of injured tissues with antigravity strength
External support - full time weaning to part-time or no support
Simple sling and abduction brace are used at night and for all activities when gravity is applied, both indoors and outdoors.
Pillows may support the limb while seated at rest or when performing exercises.
Mobilization for general indications
Phase 1 exercises are continued.
Mobilization of ipsilateral limb kinetic chain with active motion of clavicle-scapula
All the exercises from Phase 1 can be continued.
Actively assisted elevation to shoulder level can be introduced.
Note: Avoid hand behind back and extreme across body adduction at this stage. This avoids adverse rotation of the clavicle and scapula.
Activities of daily living
All activities permitted in phase 1 are continued.
Activities for domestic purposes at the tabletop level are encouraged (eg short lever arm reaching and food preparation)

Radiographic control
Radiographic evidence of fracture union is expected at this time. Confirmation of union with a concurrent reduction in symptoms permits progression to phase 3.
3. Phase 3: Beginning of week 7 to end of week 12 after injury (late repair and early tissue remodeling phase)
Phase 3 principle: reestablishment of proprioception in the limb.
Phase 3 aim: encourage normal tissue structure and reinnervation through daily activities without secondary injury.
External support – weaning from full time to no support
A sling may be preferred for support at night and outdoor activities.
Mobilization for general indications
Phase 2 exercises are continued.
Mobilization of ipsilateral limb kinetic chain with motion of the clavicle-scapula
All the exercises from Phase 1 can be continued.
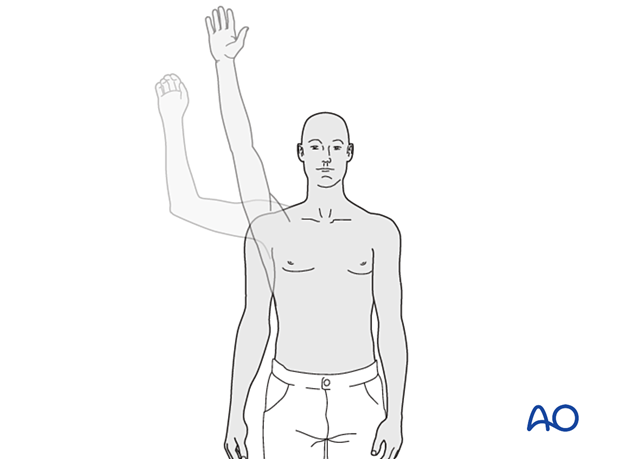
Actively assisted elevation above shoulder level can be introduced.
Note: Hand behind the back and across body adduction is permitted at this stage. This facilitates rotation of the clavicle and scapula.
Isometric and isokinetic strengthening of the rotator cuff, deltoid, and periscapular muscles are permitted.
A "shoulder therapy set" might be helpful. Typically included devices are:
An exercise bar lets the patient use the uninjured left shoulder to passively move the affected right side.
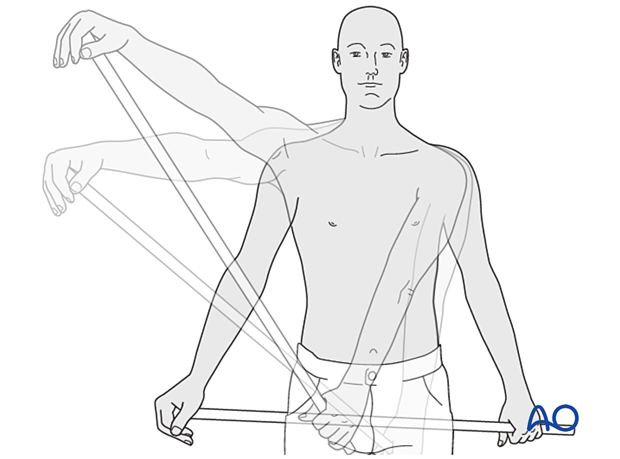
Rope and pulley assembly. With the pulley placed above the patient, the unaffected left arm can be used to provide full passive forward flexion of the injured right shoulder.

As passive motion improves and active assisted exercises progress satisfactorily and the fracture becomes fully consolidated, one can begin strengthening. The first one strengthens by active motion against gravity. To increase muscle strength, one must increase the resistance against which the muscles work. Endurance training follows.
Elastic devices (therabands) are helpful in providing varying degrees of resistance. Ultimately the athletic patient can progress to resistance machines and free weights.
Activities of daily living
All activities permitted in phase 2 are continued with the addition of social activities, active elevation, and abduction of the injured limb as comfort permits.
Radiographic control
Radiographic evidence of fracture consolidation is expected at this time. Confirmation of consolidation without adverse features (eg displacement, fixation failure, or heterotopic bone) in the absence of symptoms permits progression to phase 4.
4. Phase 4: Beginning of week 13 after injury (remodeling and reintegration phase)
Phase 4 principle: normalization of the proprioceptive function with optimal biomechanics
Phase 4 aim: to establish normal tissue structure and reinnervation through training and practice for optimal endurance.
Mobilization of ipsilateral limb kinetic chain with no limits of movement
Sport or occupational work hardening exercises are introduced under supervision.
Activities of daily living
All activities, including sport and occupational activities requiring resisted elevation and abduction, is encouraged.













