ORIF - Plate or screw fixation
1. Principles
Introduction
Optimal stability for fixation of the anatomic neck in these fracture dislocations is probably provided by angular stable plates which should be considered for patients with better bone quality and limited comminution.
A deltopectoral approach is almost always required for glenohumeral reduction.
Emergency treatment
In these fractures there is a glenohumeral dislocation and a displaced anatomical neck fracture. In some cases, neurovascular compromise results from fracture fragment displacement. If this is the case, emergency treatment is necessary. Definitive reduction and fixation should not be long delayed, particularly if one wishes to salvage the humeral head. Hemiarthroplasty should be considered alternatively for elderly, infirm, and/or severely osteoporotic patients.
Closed reduction of the glenohumeral dislocation might be attempted. It is preferable to do this in the OR to permit conversion to an open reduction, if possible. This may avoid need for an additional anesthetic.
2. Patient preparation and approaches
Patient preparation
This procedure is performed with the patient either in a beach chair or supine position.
The supine position is recommended for open reduction and plate fixation (with the beach chair as alternative).
The beach chair position is recommended for open reduction and screw fixation (with the supine position as alternative).
Approach
A deltopectoral approach is almost always required for glenohumeral reduction.
3. Glenohumeral reduction
Closed
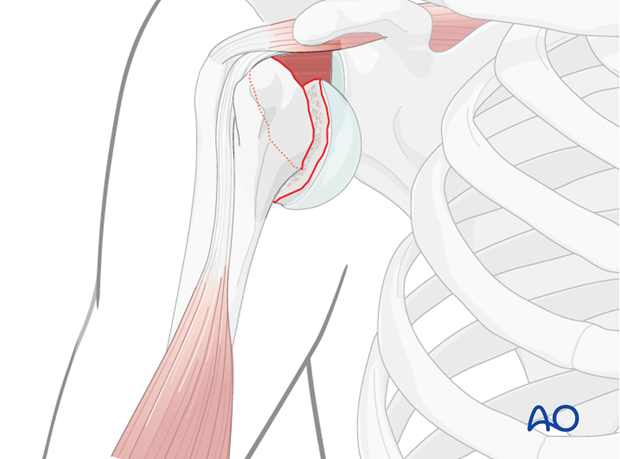
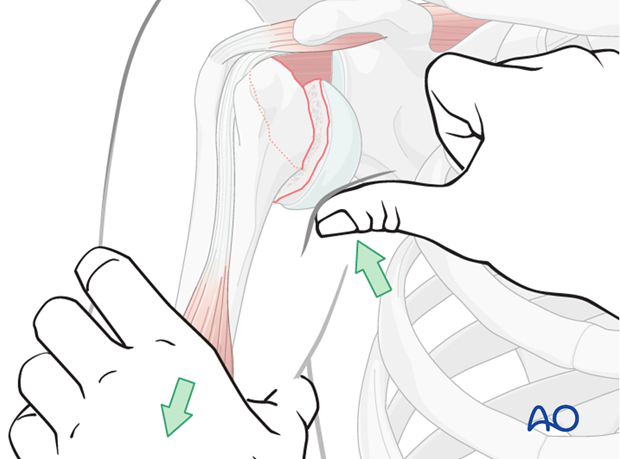
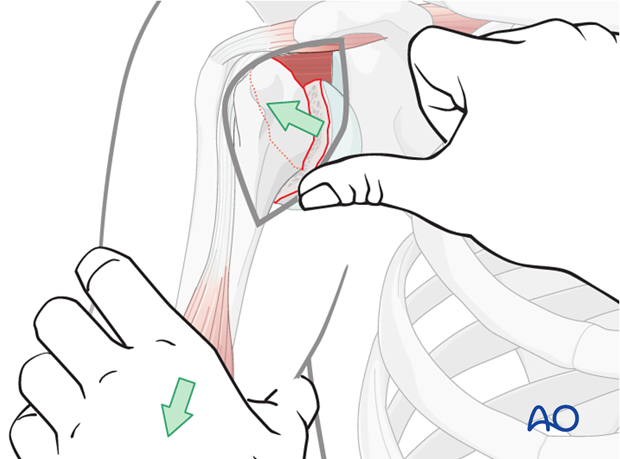
First of all, a reduction of the glenohumeral dislocation should be performed. In cases of undisrupted periosteal sleeves, this might be done in a closed manner (as illustrated). If the periosteal sleeve is disrupted, an open reduction of the glenohumeral dislocation becomes more likely. In these cases, it might become necessary to perform an arthrotomy to the glenohumeral joint via either an osteotomy of the lesser tuberosity or tenotomy of the subscapularis tendon.
Open
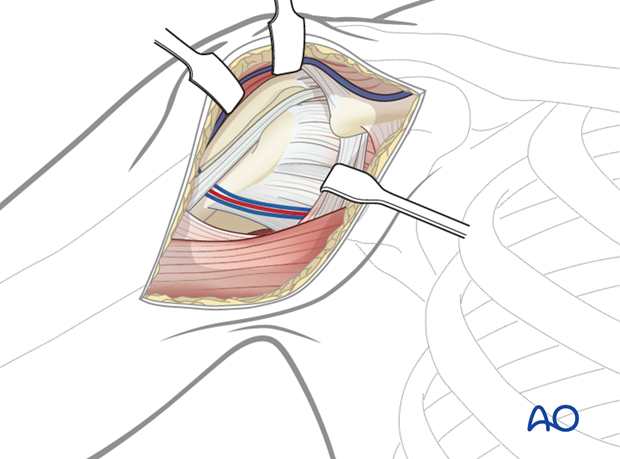
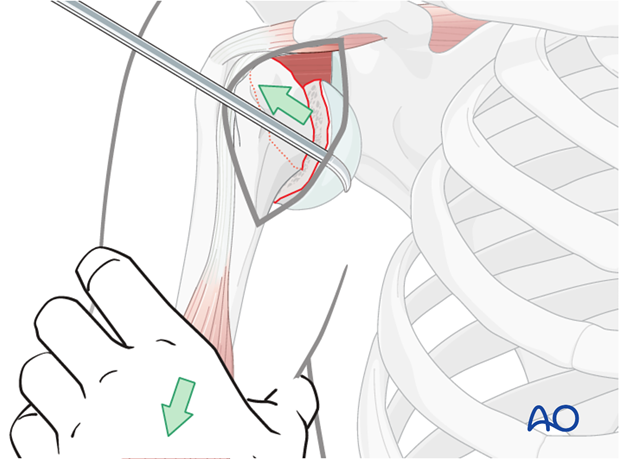
Use a deltopectoral approach.With longitudinal traction applied to the arm, the dislocated humeral head may be reduced using direct digital pressure pushing it back into position.
Option: bone hook
A bone hook can be placed carefully around the calcar avoiding damage to the articular cartilage. The head can then be pulled laterally and guided into position. Note: avoid neurovascular injury.
4. Fracture fixation following glenohumeral reduction
Once the dislocation is reduced the fracture pattern may be reassessed and one can continue with open plating, or open screw fixation, or exceptionally, with hemiarthroplasty, if satisfactory fixation cannot be achieved.
Plate fixation

Screw fixation

5. Overview of rehabilitation
The shoulder is perhaps the most challenging joint to rehabilitate both postoperatively and after conservative treatment. Early passive motion according to pain tolerance can usually be started after the first postoperative day - even following major reconstruction or prosthetic replacement. The program of rehabilitation has to be adjusted to the ability and expectations of the patient and the quality and stability of the repair. Poor purchase of screws in osteoporotic bone, concern about soft-tissue healing (eg tendons or ligaments) or other special conditions (eg percutaneous cannulated screw fixation without tension-absorbing sutures) may enforce delay in beginning passive motion, often performed by a physiotherapist.
The full exercise program progresses to protected active and then self-assisted exercises. The stretching and strengthening phases follow. The ultimate goal is to regain strength and full function.
Postoperative physiotherapy must be carefully supervised. Some surgeons choose to manage their patient’s rehabilitation without a separate therapist, but still recognize the importance of carefully instructing and monitoring their patient’s recovery.
Activities of daily living can generally be resumed while avoiding certain stresses on the shoulder. Mild pain and some restriction of movement should not interfere with this. The more severe the initial displacement of a fracture, and the older the patient, the greater will be the likelihood of some residual loss of motion.
Progress of physiotherapy and callus formation should be monitored regularly. If weakness is greater than expected or fails to improve, the possibility of a nerve injury or a rotator cuff tear must be considered.
With regard to loss of motion, closed manipulation of the joint under anesthesia, may be indicated, once healing is sufficiently advanced. However, the danger of fixation loosening, or of a new fracture, especially in elderly patients, should be kept in mind. Arthroscopic lysis of adhesions or even open release and manipulation may be considered under certain circumstances, especially in younger individuals.
Progressive exercises
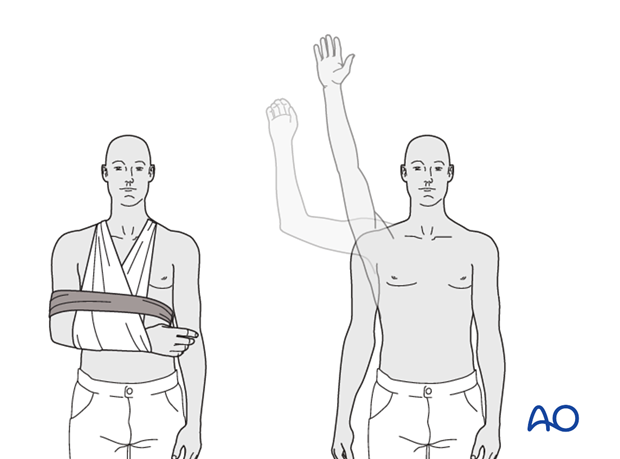
Mechanical support should be provided until the patient is sufficiently comfortable to begin shoulder use, and/or the fracture is sufficiently consolidated that displacement is unlikely.
Once these goals have been achieved, rehabilitative exercises can begin to restore range of motion, strength, and function.
The three phases of nonoperative treatment are thus:
- Immobilization
- Passive/assisted range of motion
- Progressive resistance exercises
Immobilization should be maintained as short as possible and as long as necessary. Usually, immobilization is recommended for 2-3 weeks, followed by gentle range of motion exercises. Resistance exercises can generally be started at 6 weeks. Isometric exercises may begin earlier, depending upon the injury and its repair. If greater or lesser tuberosity fractures have been repaired, it is important not to stress the rotator cuff muscles until the tendon insertions are securely healed.
Special considerations
Glenohumeral dislocation: Use of a sling or sling-and-swath device, at least intermittently, is more comfortable for patients who have had an associated glenohumeral dislocation. Particularly during sleep, this may help avoid a redislocation.
Weight bearing: Neither weight bearing nor heavy lifting are recommended for the injured limb until healing is secure.
Implant removal: Implant removal is generally not necessary unless loosening or impingement occurs. Implant removal can be combined with a shoulder arthrolysis, if necessary.
Shoulder rehabilitation protocol
Generally, shoulder rehabilitation protocols can be divided into three phases. Gentle range of motion can often begin early without stressing fixation or soft-tissue repair. Gentle assisted motion can frequently begin within a few weeks, the exact time and restriction depends on the injury and the patient. Resistance exercises to build strength and endurance should be delayed until bone and soft-tissue healing is secure. The schedule may need to be adjusted for each patient.
Phase 1 (approximately first 3 weeks)
- Immobilization and/or support for 2-3 weeks
- Pendulum exercises
- Gently assisted motion
- Avoid external rotation for first 6 weeks
Phase 2 (approximately weeks 3-9)
If there is clinical evidence of healing and fragments move as a unit, and no displacement is visible on the x-ray, then:
- Active-assisted forward flexion and abduction
- Gentle functional use week 3-6 (no abduction against resistance)
- Gradually reduce assistance during motion from week 6 on
Phase 3 (approximately after week 9)
- Add isotonic, concentric, and eccentric strengthening exercises
- If there is bone healing but joint stiffness, then add passive stretching by physiotherapist













