Bridge plate
1. Bridge plating principles
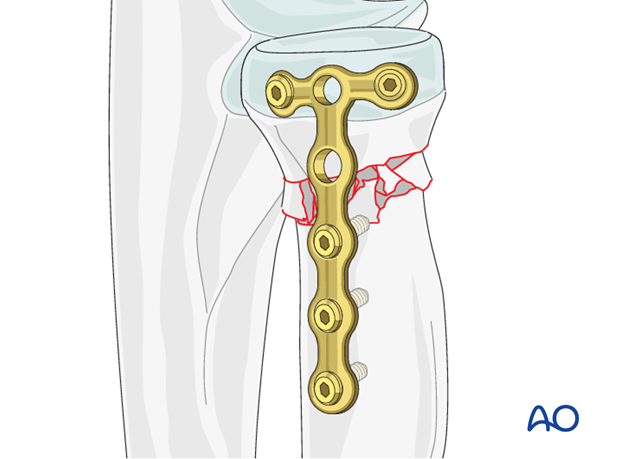
In multifragmentary fractures of the radial neck, fixation of the radial head to the diaphysis is achieved by bridge plating.
Bridge plating uses the plate as an extramedullary splint, fixed to the two main fragments, while the intermediate fracture zone is left untouched.
Anatomical reduction of the intermediate fragments is not necessary but alignment, rotation and length of the radius must be restored.
2. Plate positioning
The radial head is completely covered by articular cartilage. The implant is applied to the radial head in a location that causes the least compromise of full pronation and supination.
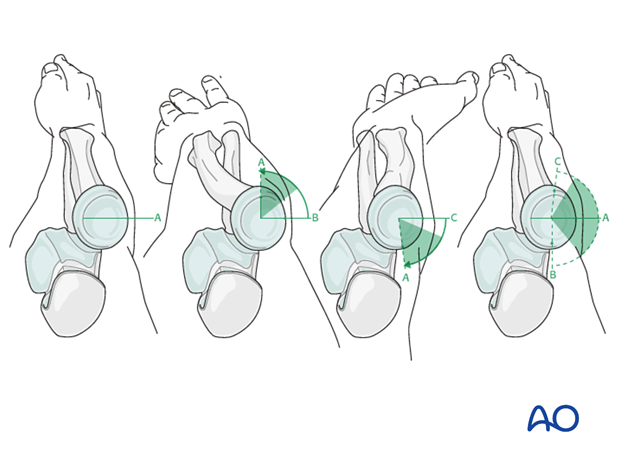
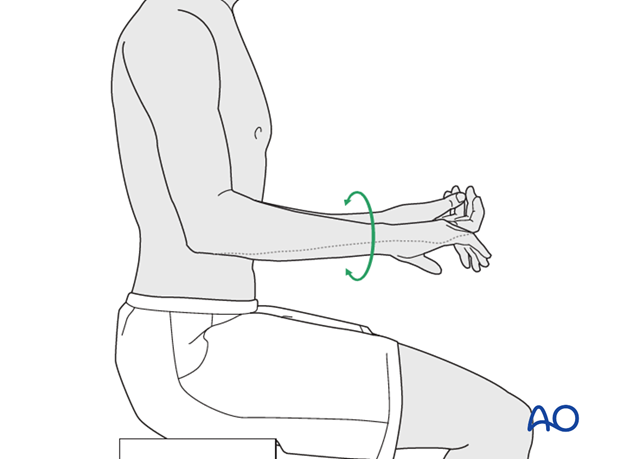
Safe zone for plate and screw insertion
To determine the location of the “safe zone”, reference marks are made along the radial head and neck, to mark the midpoint of the visible bone surface. Three such marks are made with the forearm in neutral rotation, full pronation, and full supination as shown in the illustration.
The posterior limit of the safe zone lies halfway between the reference marks made with the forearm in neutral rotation and full pronation. The anterior limit lays nearly two thirds of the distance between the neutral mark and the mark made in full supination.
Note: The non-articulating portion of the safe zone for the application of implants to the radial head (or safe zone for prominent fixation) consistently encompasses a 90 degrees angle localized by palpation of the radial styloid and Lister’s tubercle.
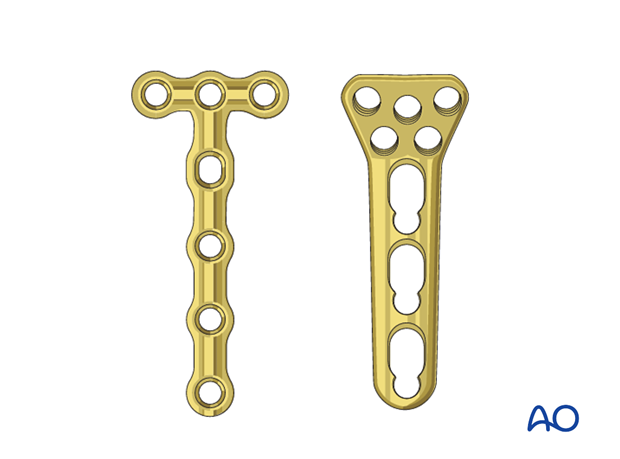
3. Choice of implant
As the radial head is a small fragment, a 1.5 or 2.0 T-plate, or a locking proximal radius plate is used to allow purchase of two or three screws in the proximal fragment.
The plate length depends on the fracture fragmentation. With a larger fracture zone, a longer plate has to be chosen.
Prebend the plate according to the surface anatomy of the proximal radius.
4. Positioning and approach
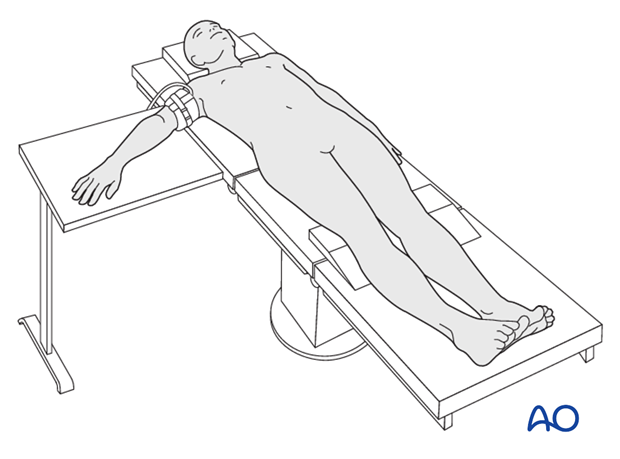
Positioning
This procedure is normally performed with the patient in a supine position for lateral access.
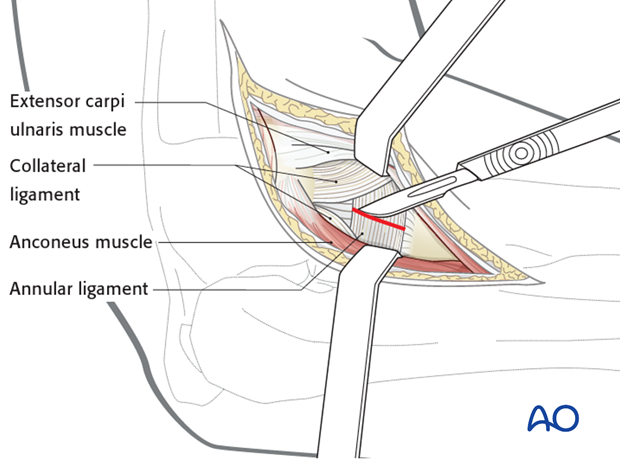
Approach
For this procedure a lateral approach is normally used.
5. Reduction and fixation
Indirect reduction
In multifragmentary radial neck fractures, indirect reduction is performed. Apply a contoured plate with two or three screws to the radial head.
With the help of reduction forceps, adjust the plate to the diaphysis correcting length, rotation, and alignment.
Use intraoperative C-arm evaluation to check for adequate length and restoration based on contra and ipsilateral wrist.
If reduction is difficult to achieve without subluxation, rule out ulnar malreduction as the cause.
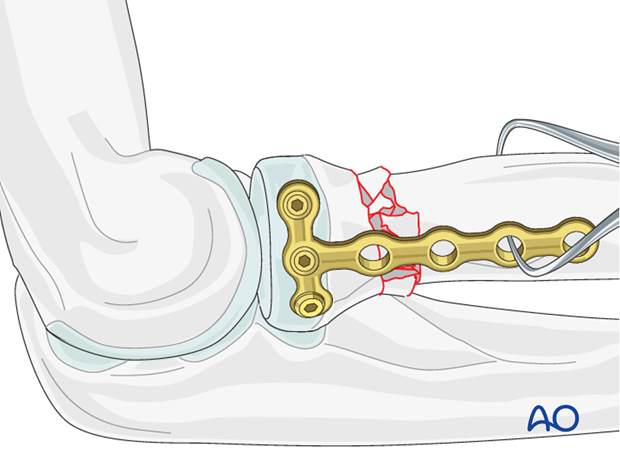
Distal fixation
Fix the plate with two or three bicortical 1.5 or 2.0 mm screws to the distal fragment.

6. Final assessment
Check supination and pronation. Fixation should be stable. Crepitus or restricted motion should be absent. Check fractures and fixation with image intensifier or x-ray.
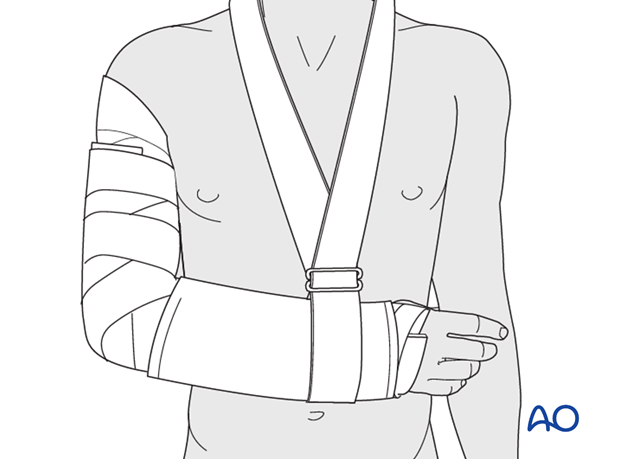
7. Postoperative treatment following ORIF
Postoperatively, the elbow may be placed for a few days in a posterior splint for pain relief and to allow early soft tissue healing, but this is not essential. To help avoid a flexion contracture, some surgeons prefer to splint the elbow in extension.
If drains are used, they are removed after 12–24 hours.
Mobilization
Active assisted motion is encouraged within the first few days including gravity-assisted elbow flexion and extension. Encourage the patient to move the elbow actively in flexion, extension, pronation and supination as soon as possible. Delay exercises against resistance until healing is secure.
Use of the elbow for low intensity activities is encouraged, but should not be painful.
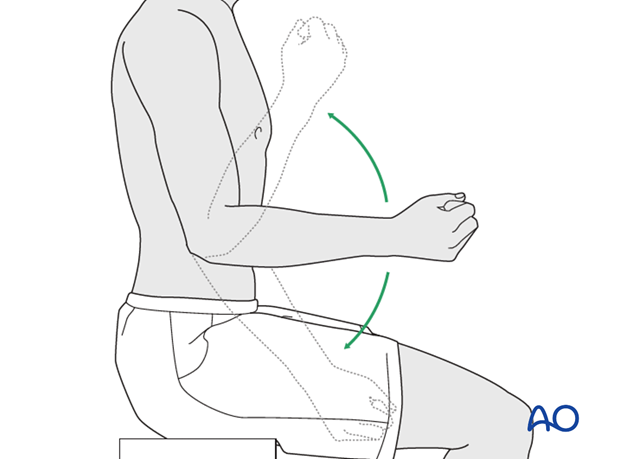
Range of motion must be monitored to prevent soft tissue contracture.
Prevent loading of the elbow for 6–8 weeks.
Monitor the patient to assess and encourage range of motion, and return of strength, endurance, and function, once healing is secure.
Follow up
The patient is seen at regular intervals (every 10–20 days at first) until the fracture has healed and rehabilitation is complete.
Implant removal
As the proximal ulna is subcutaneous, bulky plates and other hardware may cause discomfort and irritation. If so, they may be removed once the bone is well healed, 12–18 months after surgery, but this is not essential.













