Sliding hip screw with trochanter stabilization plate
1. General considerations
Introduction
To support the lateral wall, the dynamic hip screw (DHS) is coupled with the trochanter stabilization plate (TSP), which augments the fragile lateral wall and prevents excessive fracture collapse.
Optionally, the antirotation wire can be replaced by a cannulated screw parallel to the DHS lag screw.
The sliding hip screw is designed to allow controlled collapse. The collapse is limited as the base of the neck comes to rest on the greater trochanter. If the greater trochanter is very comminuted and the lateral wall is involved, control of the collapse is lost. A trochanteric supporting plate (TSP) may be used to restore the supporting effect of these structures.

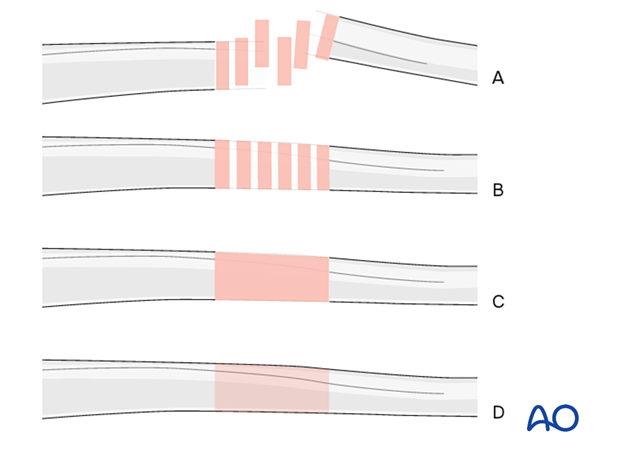
Throughout this treatment option illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fracture
B) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
Closed vs open reduction
Fracture reduction should start with a closed attempt.
If manipulation does not lead to a satisfactory reduction, a percutaneous reduction technique should be performed.
The definitive decision for the treatment will be made after positioning the patient and an initial closed reduction. Since emergency department x-rays are often of suboptimal quality, verifying the preoperative diagnosis using image intensification is necessary.
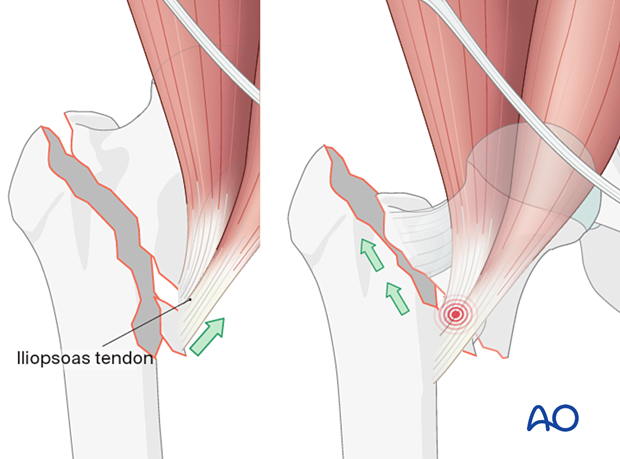
The pull of the iliopsoas muscle may flex and externally rotate the proximal fragment, and traction will not correct this displacement. In these cases, open reduction is often necessary.
Superolateral displacement of the shaft (right illustration) after high-energy trauma is a sign of an irreducible intertrochanteric fracture and requires open reduction.
The displacement of the medial neck spike causes button-holing anteromedially through the iliofemoral ligament, anterior capsule, and iliopsoas.
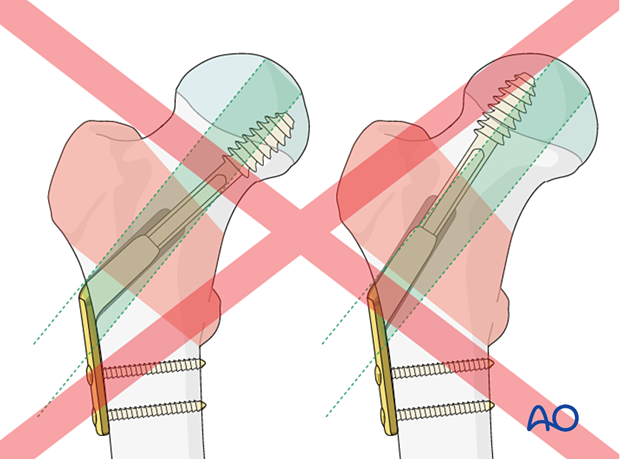
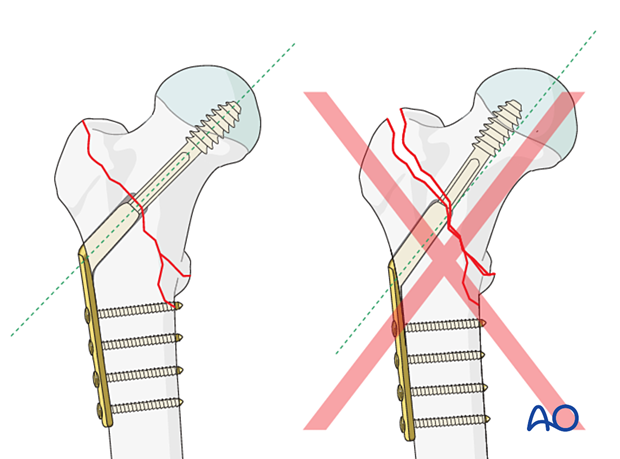
Correct position of lag screw or blade
The thread of the lag screw (or tip of the spiral blade) needs to end in the trabecular bone structures to gain enough purchase. Therefore, it is important that the lag screw comes to lie in the center of the head-neck axis or slightly inferior to it. This allows for increased depth of the screw.
Imaging
If the trauma plain films show a potentially unstable fracture but do not give enough detail about the fracture morphology, 3-D CT is a powerful tool for better diagnosis and planning a strategy for a successful surgery.
Implant selection and preoperative planning
Spiral blade vs lag screwThere is not yet a clear indication of when to use a spiral blade and when a lag screw. It is, therefore, often surgeon’s preference.
In a young patient with hard bone, a blade is relatively contraindicated, and a screw should be used instead (with tapping).
In elderly patients, the use of a blade does compact the bone.
Generally, a four-hole DHS plate with the preoperatively determined neck-shaft angle will be chosen in combination with a TSP.
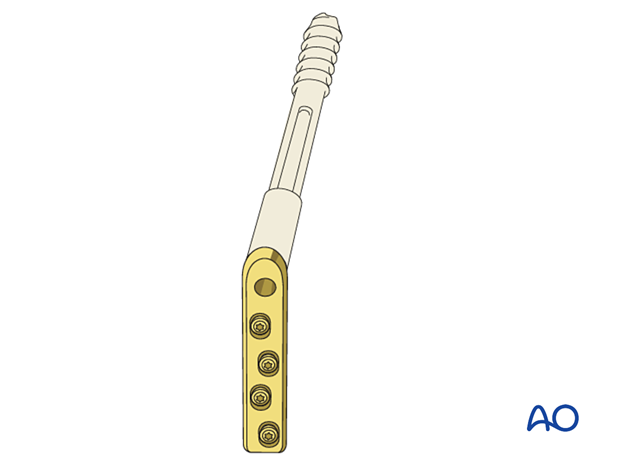
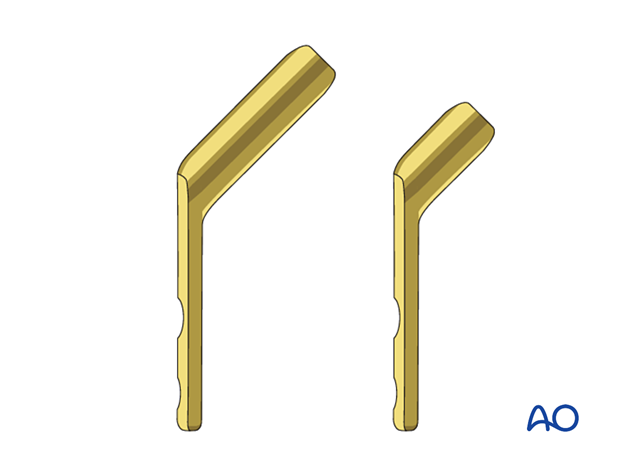
A plate with a short barrel (illustration on the right) may be used if the lag screw length is ≤ 75 mm to allow for sliding.
A short barrel should only be considered if its end would impinge dense cancellous bone in the head.
For proper insertion of the implant, determine the optimal neck-shaft angle on the basis of the contralateral intact proximal femur. This is usually 130° or 135° depending on the patient.
If this is not available due to previous hip-joint replacement or improper AP view with external rotation of the proximal femur, provisionally reduce the fracture before draping under traction and assess the reduction quality. If acceptable, measure the angle from the AP view after reduction.
AO teaching video
Femur, Proximal – Trochanteric Fractures – Stabilization Using the Dynamic Hip Screw (DHS) and a Demonstration Exercise Using DHS in Combination with the Universal Locking Trochanter Stabilizing Plate (ULTSP)
(26 minutes)
2. Patient preparation
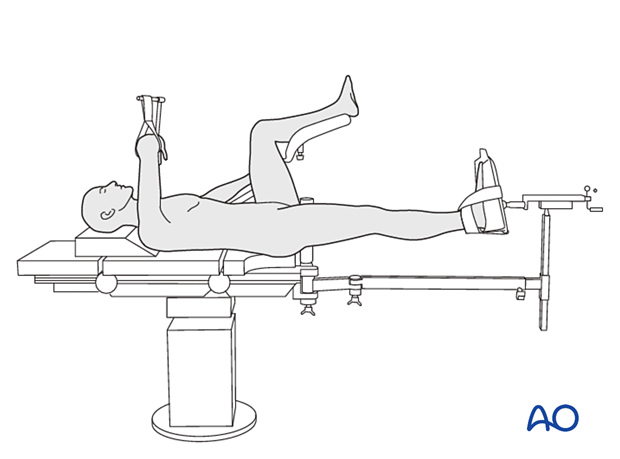
Position the patient supine on a fracture table either with the contralateral uninjured leg placed on a leg holder or in a scissors configuration.
For C-arm positioning to acquire optimal AP, lateral, and axial views, read the additional material on:
3. Reduction
Closed reduction
Closed reduction is usually achieved by:
- Pulling in the direction of the long axis of the leg to distract the fragments and regain length
- Adjustment of internal rotation of the femoral shaft ...
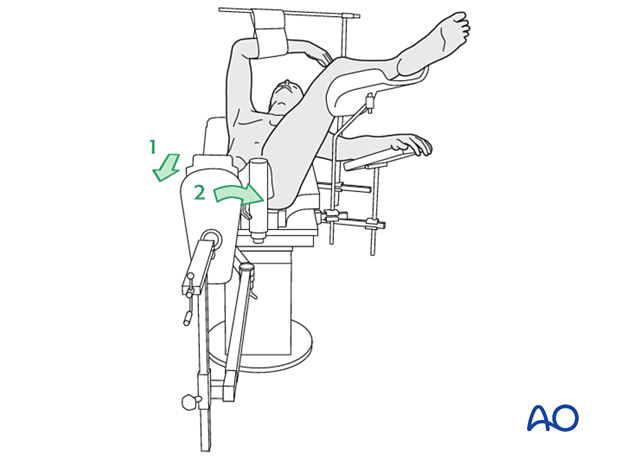
... until the patella is facing forward on an AP view of the knee joint
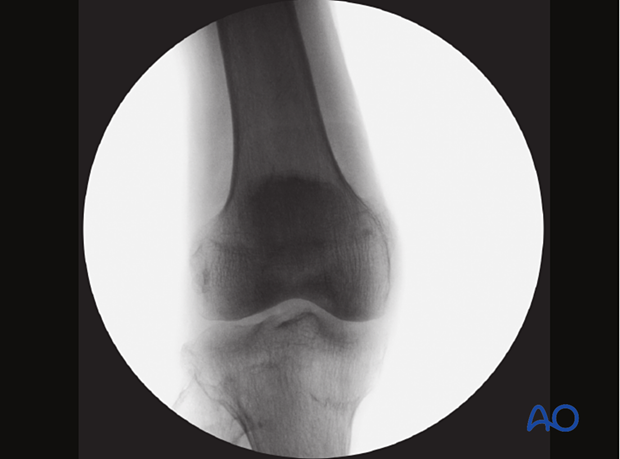
Check the reduction in both the AP and lateral view with an image intensifier.

Assessment of reduction quality
Read the fracture line on the image intensifier views. Identify gaps or increased density due to overlapping of fragments.
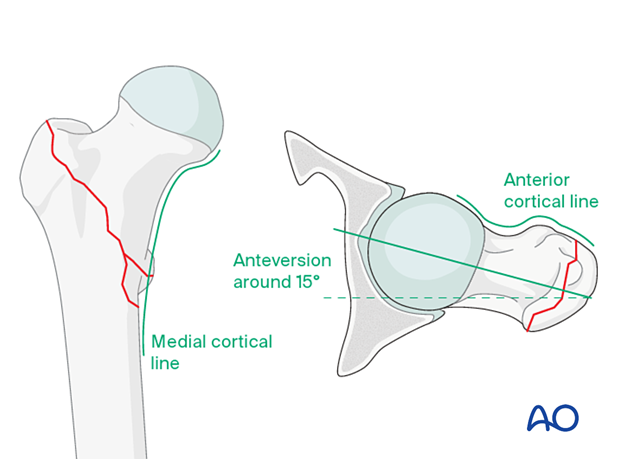
Follow the medial cortical line on the AP view and the anterior cortical line on the axial view. Identify any translational or angular malalignment.
Acceptable reduction quality shows the following patterns:
- No gap or increased density visible along the fracture line
In the AP view:
- Continuous medial cortical line
- No varus angulation
In the lateral view:
- Anteversion approximately 15°
- Continuous anterior cortical line
For more details, see the additional material on assessment of reduction quality.
Percutaneous reduction
If closed reduction is not satisfactory, carry out a percutaneous reduction technique.
Open reduction
If closed reduction fails, carry out an open reduction through a lateral approach.
Enlarge the lateral incision as necessary by increasing its length and retracting the vastus lateralis anteriorly and medially. Direct visualization of the fracture site is usually unnecessary.
Clear the fracture site of interposed soft tissue all along the fracture line as needed.
Then restore gross length and rotation with the fracture table.
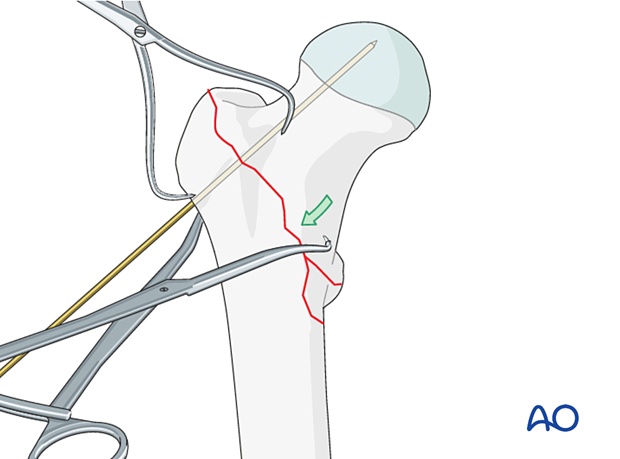
Place pointed reduction forceps so that one point catches the medial cortex proximal to the lesser trochanter.
Reduction is achieved by closing the forceps. Temporarily maintain the alignment with a 2.0 mm K-wire perpendicular to the fracture line.
Confirm the reduction with the image intensifier.
4. Approach for implant insertion
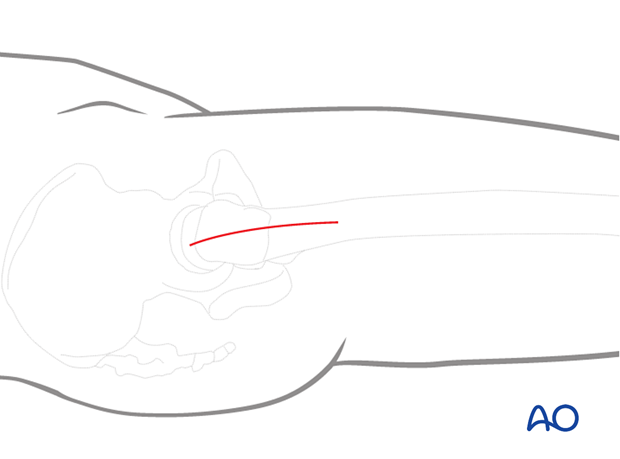
If the reduction has been performed closed or percutaneous, perform a limited lateral approach with an incision large enough to insert the implant and cortical screws.
5. Guide-wire insertion
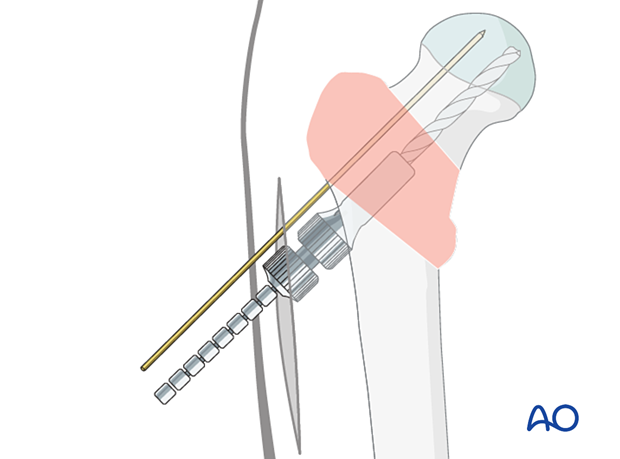
Insertion of antirotation wire
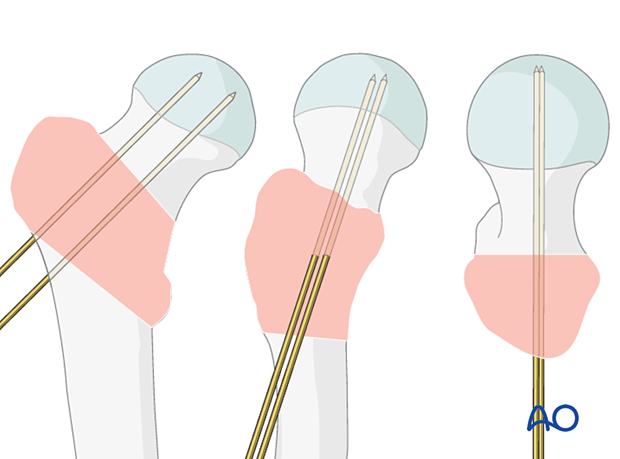
To avoid rotational displacement during screw insertion, place an antirotation wire parallel and proximal to the head-neck axis.
If a K-wire used for temporary fixation is in an appropriate position, this can be used instead.

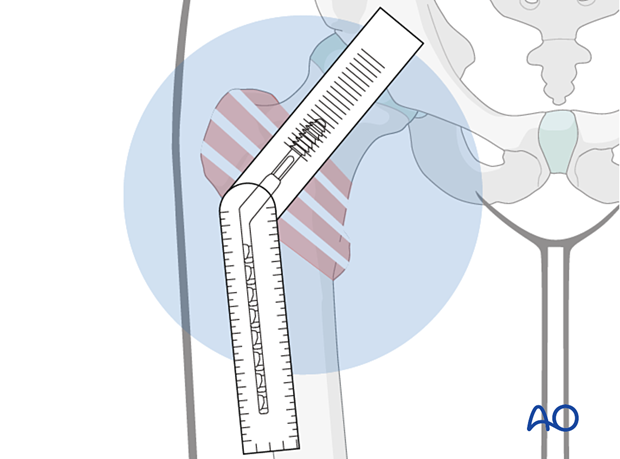
Application of the aiming device
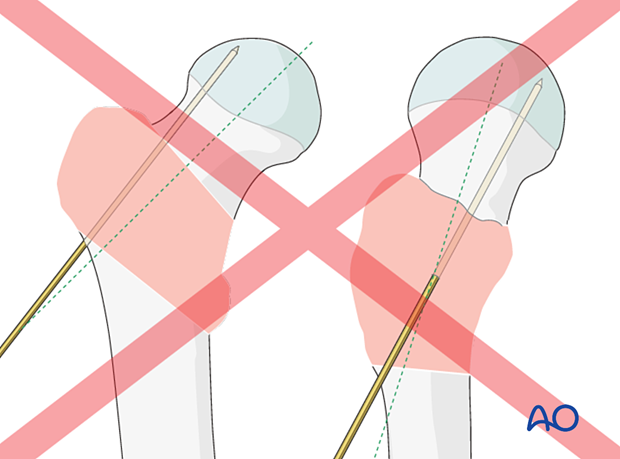
Place the appropriate aiming device so that the screw trajectory runs through the head-neck axis or parallel and slightly inferior to that on an AP view.
This ensures that the tip of the blade or lag-screw thread ends in the trabecular bone structures.
Check its position with the image intensifier in AP, lateral, and axial views. In all views, the trajectory should be in line with the head-neck axis.

Insertion of a guide wire for the screw
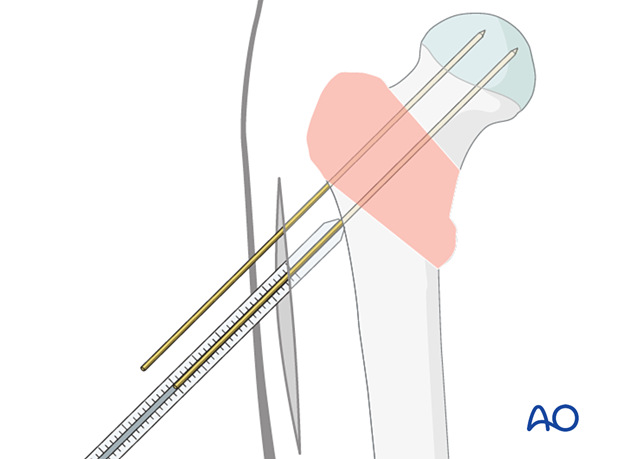
Insert the guide wire through the aiming device and advance it into the subchondral bone of the head. Stop the insertion only 5 mm short of the joint. This helps prevent guide-wire pullout during reaming.
Position it so that in the AP view, it is through the center or slightly inferior to the neck and in the lateral and axial view in the center of the neck.
6. Screw insertion
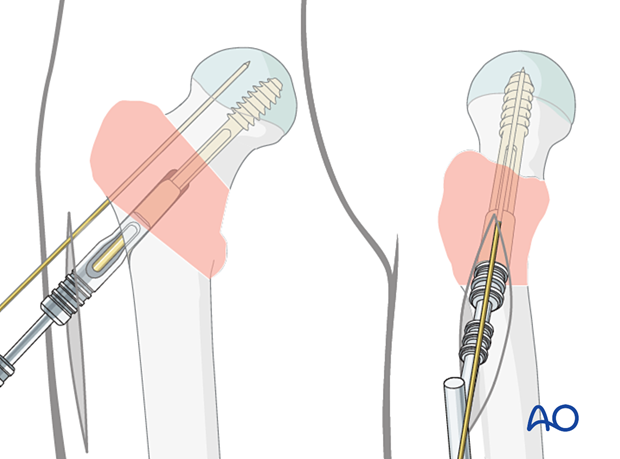
Determination of lag-screw length
Determine the length of the lag screw with the help of the measuring device. Select a screw that is 5–7 mm shorter than the measured length.
Reaming
Adjust the cannulated triple reamer to the chosen length of the screw.
Slide the reamer over the guide wire and simultaneously drill for the lag screw, ream for the plate barrel, and countersink for the plate-barrel junction.
Insertion of the femoral neck screw
In patients with hard bone, it is best to tap for the screw. Otherwise, the screw may not advance, and you may displace the fracture by twisting the proximal fragment as you attempt to insert the screw.
Mount the correct screw on the handle and insert it through the centering sleeve over the guide wire. By turning the handle, it is advanced into the bone. Do not push forcefully to avoid distraction of the fracture.
The antirotation wire may help to avoid rotational displacement.
When the screw has reached its final position – 5–7 mm short of the subchondral bone in the AP and lateral view – the T-handle of the insertion piece should be parallel to the axis of the proximal femur to ensure the correct position of the plate.
7. Fixation of the DHS plate
Application of the DHS plate
Take the plate with the previously chosen neck-shaft angle, slide it over the guide wire, and mate it correctly with the screw.
Push it in over the screw and seat it home with the impactor.

Plate fixation
Fix the plate to the femoral shaft with one cortical screw in the second shaft screw hole to maintain the DHS position while applying the TSP.
Remove the antirotation wire.
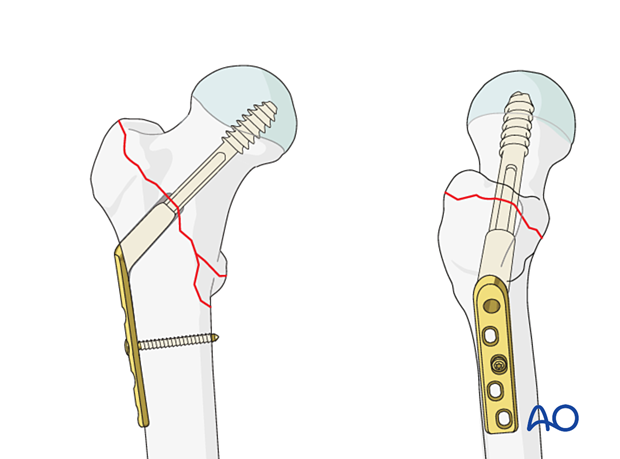
8. Application of trochanter stabilization plate (TSP)
Plate preparation
If necessary, contour the spoon-shaped end of the trochanter stabilization plate (TSP) to fit the mass of the greater trochanter. Position the TSP over the DHS plate so that it is securely seated and that the screw holes line up.
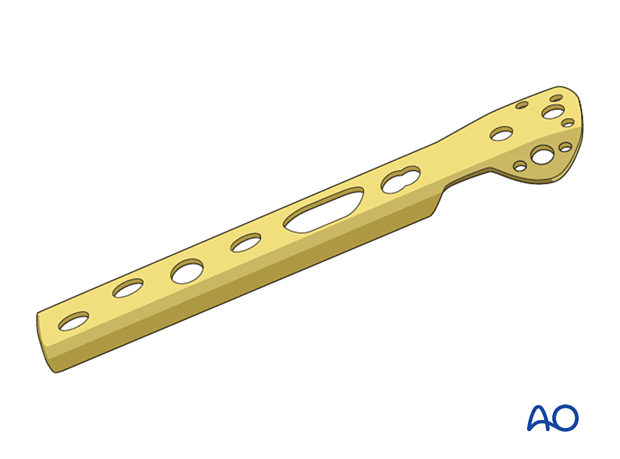
Plate application
Slide the TSP over the DHS plate through the existing incision.
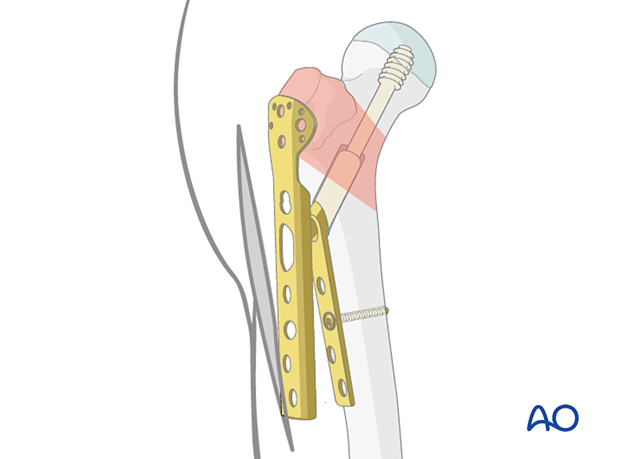
Fix the plate using the holding cortical screws which connect the plate to the shaft.
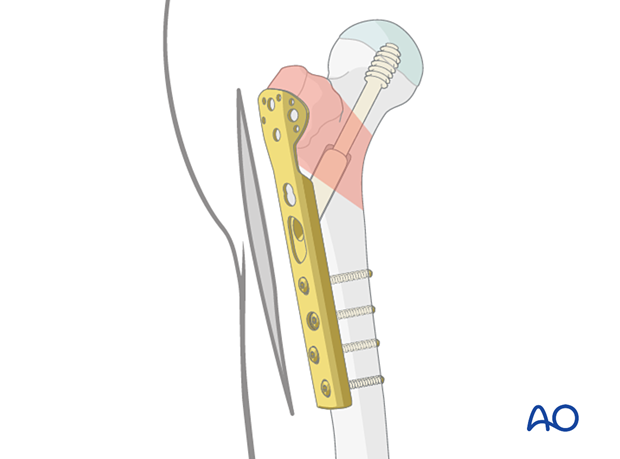
Depending on the fracture pattern, if the TSP does not capture the greater trochanter, tension band wiring may be added to hold the abductor muscle insertion reduced and securely fixed.
A screw may also be added through the plate into the neck to prevent rotation of the head and neck fragment.

9. Final assessment
Confirm fracture stabilization and implant position on AP, lateral, and axial views.
10. Aftercare
Postoperative mobilization
The elderly patient may start with weight bearing as tolerated with walking aids the day after surgery.
Unrestricted range-of-motion exercises of the hip joint are allowed.

Pain control
To facilitate rehabilitation and prevent delirium, it is important to control the postoperative pain properly, eg, with a specific nerve block.
VTE prophylaxis
Patients with lower extremity fractures requiring treatment require deep vein prophylaxis.
The type and duration depend on VTE risk stratification.
Follow-up
Follow-up assessment for wound healing, neurologic status, function, and patient education should occur within 10–14 days.
At 3–6 weeks, check the position of the fracture with appropriate x-rays.
Recheck 6 weeks later for progressive fracture union.
Implant removal
Only if necessary (eg, painful irritation), and not before union of the fracture. There is a high risk of a femoral neck fracture.
Prognosis of proximal femoral fractures in elderly patients
For prognosis in elderly patients, see the corresponding additional material.













