Assessment of reduction quality (trochanteric fractures)
1. General considerations
It is important to assess the reduction quality correctly and repeatedly (to recognize and correct intraoperative redisplacement).
The following displacement patterns should be identified:
- Discontinuing cortical lines (eg, gaps and step-offs)
- Overlapping fragments
- Translation and sagging
- Angulation (especially varus)
For C-arm positioning to acquire optimal AP, lateral, and axial views, read the additional material on:
2. Reading the fracture lines
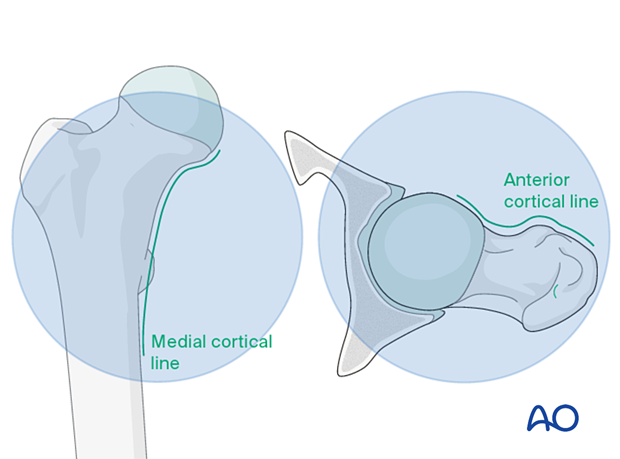
Read the fracture line on the image intensifier views. Identify gaps or increased density due to overlapping of fragments.
Follow the medial cortical line on the AP view and the anterior cortical line on the axial view. Identify any translational or angular malalignment.
3. Acceptable reduction
Acceptable reduction quality shows the following patterns:
- No gap or increased density visible along the fracture line
In the AP view:
- Continuous medial cortical line
- No varus angulation
In the lateral view:
- Anteversion approximately 15°
- Continuous anterior cortical line
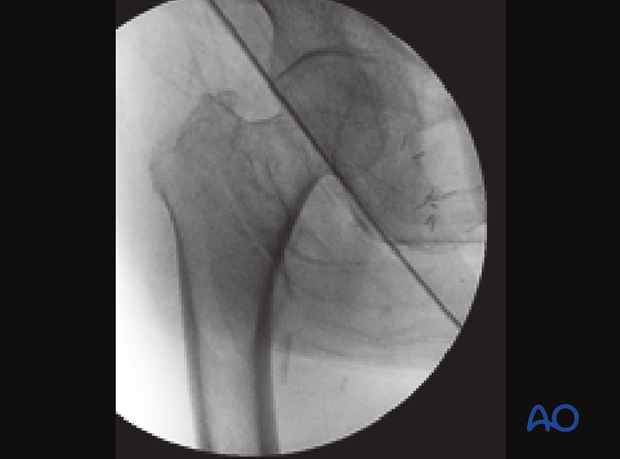
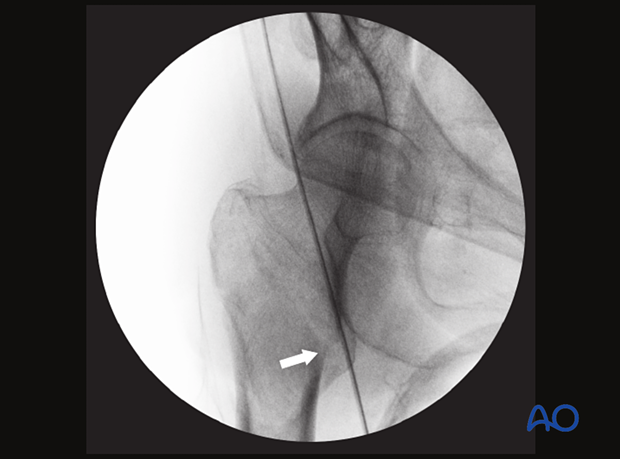
This case shows anatomical reduction in the AP view with continuous medial cortical line and physiological coxa vara.
4. Displacement patterns (cases)
Angulation
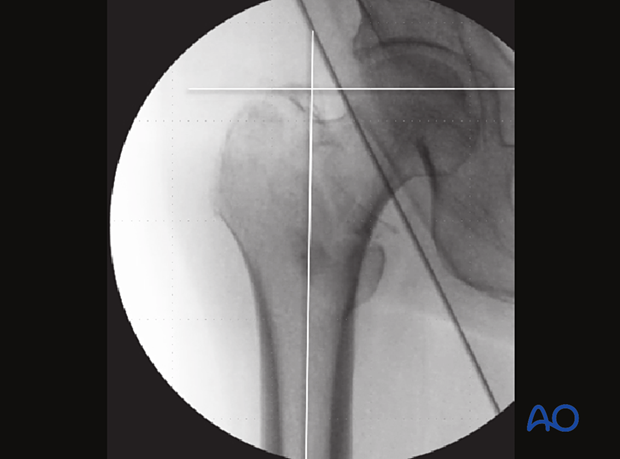
Varus angulationTo identify a varus angulation, compare the AP image with the one of the contralateral side, if available.
Alternatively, on the AP image, draw a line along the axis of the proximal femur and a perpendicular line on the level of the tip of the greater trochanter. This line should run through the center of the femoral head.
If it runs above, varus angulation should be suspected.
This case shows anatomical reduction with physiological coxa vara (common in Asian females), requiring 125° implant angulation instead of 130°.
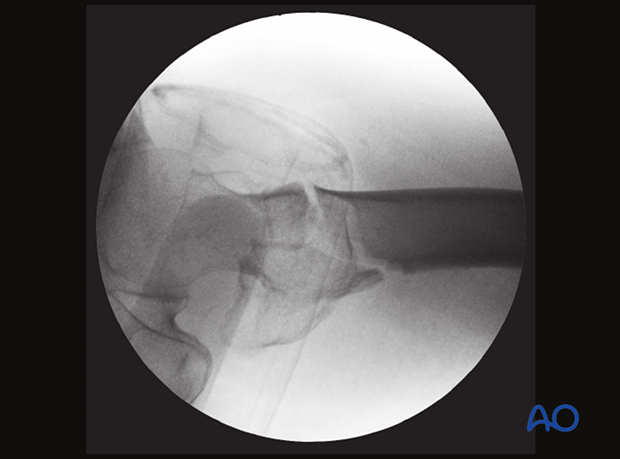
AP view with a medial opening (medial cortical line disruption; arrow) and valgus deformity
Axial view showing an opening of the anterior cortical line with slight anterior angulation
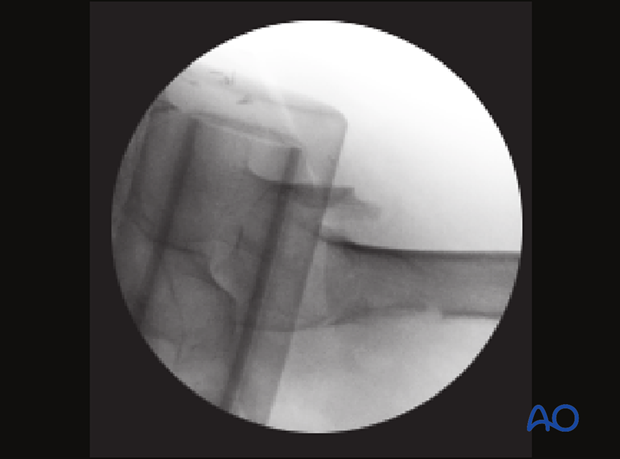
Translation
Axial view with a posterior translation of the shaft, sagging and slight anterior angulation of the proximal fragment
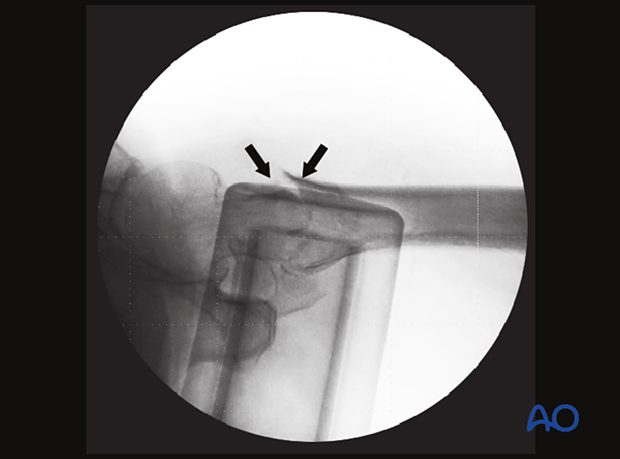
Step-off
In this case of a minimally displaced fracture, there is a step-off (arrows) of the medial cortical line. This can easily be missed and needs to be reduced to prevent excessive fracture collapse into the medullary canal.
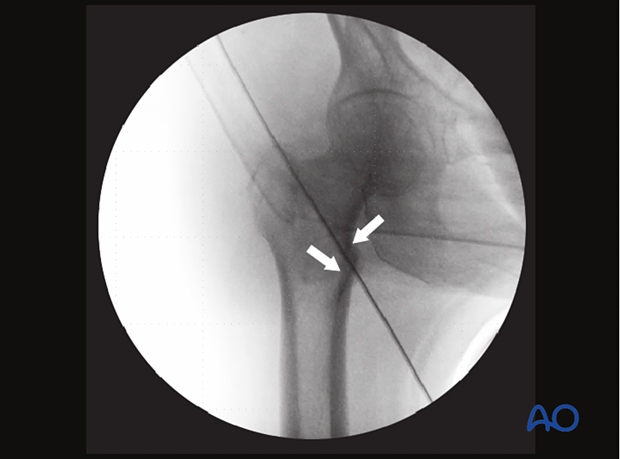
In the axial view, the displacement into the medullary canal is obvious.