Cannulated screws
1. General considerations
Principles of cancellous screw fixation
Use three cancellous screws.
Washers for the superior screws may be used to stop the screw heads from penetrating the lateral cortex of the greater trochanter. One is not needed for the inferior screw.
These screws can be inserted through a small open or percutaneous incisions.
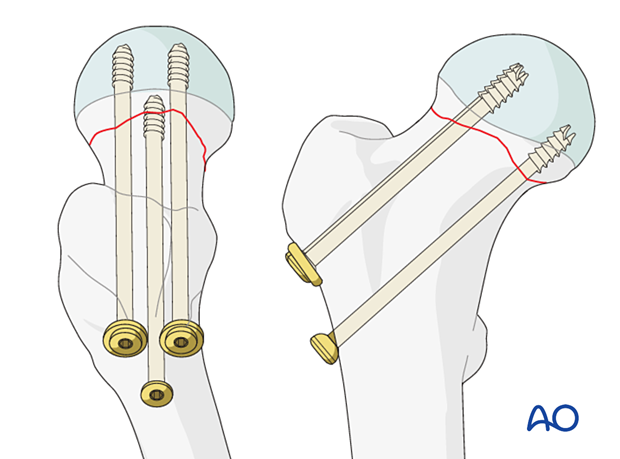
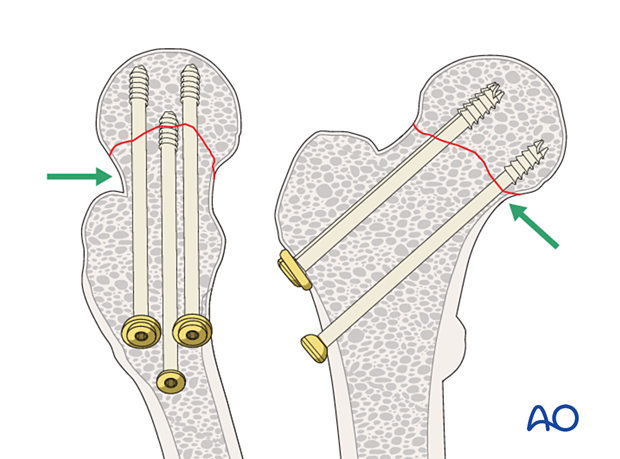
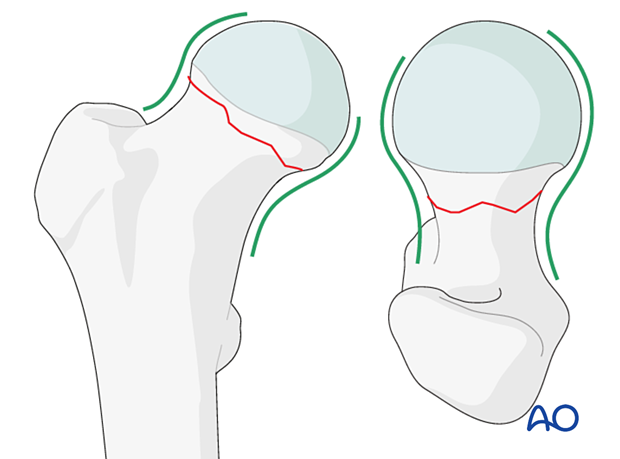
Since cancellous bone in the femoral neck in elderly patients is either absent or too osteoporotic to resist shearing forces screws must rest on the cortical endosteum to achieve three-point fixation.
The shaft of the inferior screw should rest on the endosteum of the proximal medial femoral neck. This cortical support of the screw provides a fulcrum to resist varus collapse.
The posterior screw should be within 3 mm of the endosteum of the posterior neck. This cortical support will effectively resist retroversion collapse.
Treatment principles of neck fractures in combination with hip dislocation
Most of these combined injuries result from high-impact trauma in young patients. The treatment goal is to reduce the hip and achieve anatomical reduction and stabilization of the femoral neck fracture.
If there is late complication with AVN, revision surgery with total hip arthroplasty should be considered.
Closed vs open reduction
Fracture reduction should start with a closed attempt.
If manipulation does not lead to a satisfactory reduction, a percutaneous reduction technique should be performed.
The definitive decision for the treatment will be made after positioning the patient and an initial closed reduction. Since emergency department x-rays are often of suboptimal quality, verifying the preoperative diagnosis using image intensification is necessary.
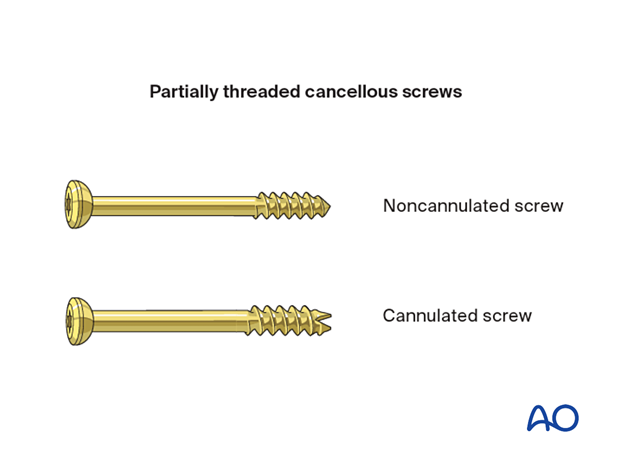
Screw selection
Cannulated (7.0 or 7.3 mm) or noncannulated (6.5 mm) cancellous screws may be used.
Cannulated screws are easier to insert but not available in some hospitals.
Insertion of cannulated screws is shown in this procedure.
2. Patient preparation
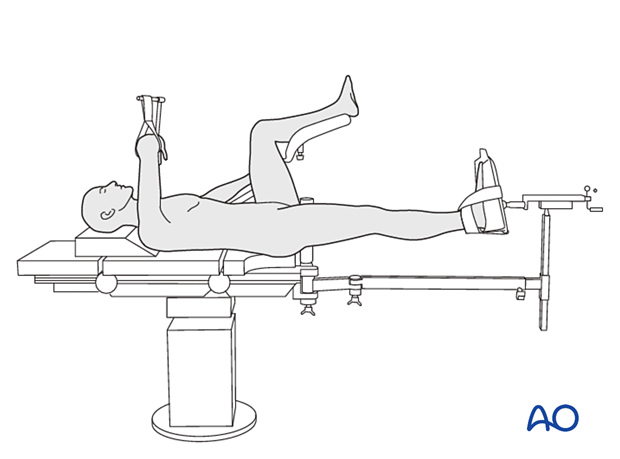
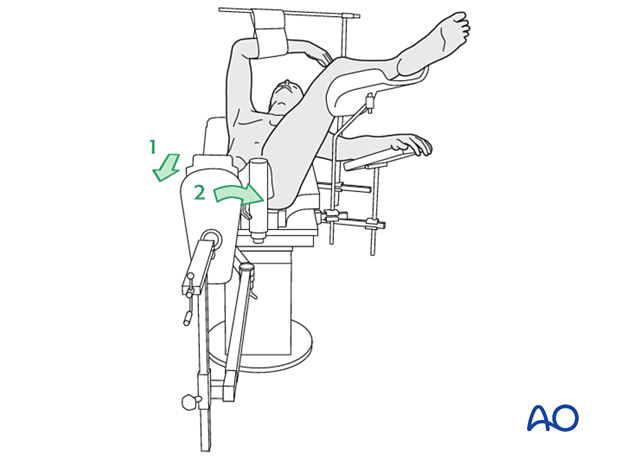
If the surgeon wishes to freely move the leg for reduction, the patient can be positioned supine on a radiolucent operating table. A fracture table can be used if the surgeon thinks that reduction can be obtained through the traction device on a fracture table.
C-arm image intensifier control during surgery is a must.
To obtain appropriate lateral views of the hip and proximal femur, the contralateral leg is best placed in a leg holder in flexion but can be scissored into hip extension.
For C-arm positioning to acquire optimal AP, lateral, and axial views, read the additional material on:
3. Reduction
Closed reduction
Closed reduction is usually achieved by:
- Pulling in the direction of the long axis of the leg to distract the fragments and regain length
- Adjustment of internal rotation of the femoral shaft ...
... until the patella is facing forward on an AP view of the knee joint
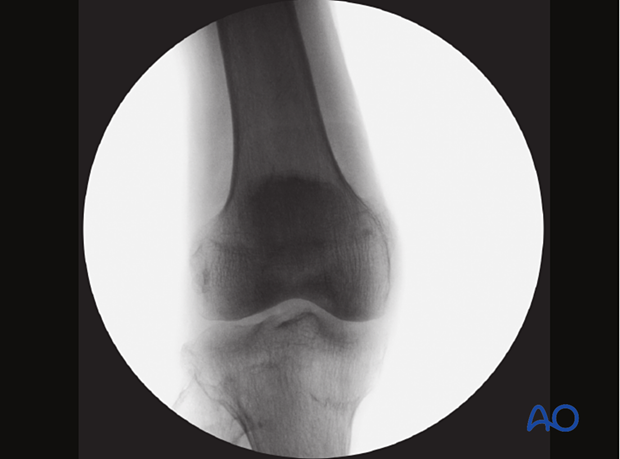
Check the reduction in both the AP and lateral view with an image intensifier.

Assessment of reduction quality
Read the fracture line on the image intensifier views. Identify gaps or increased density due to overlapping of fragments.
Follow the medial and lateral cortical lines on the AP view and the anterior and posterior cortical lines on the axial view. Identify any translational or angular malalignment.
Acceptable reduction quality shows the following patterns:
In the AP view:
- Continuous medial and lateral cortical lines
- No varus angulation
In the lateral view:
- Normal anteversion
- No retroversion
- Continuous anterior and posterior cortical lines
The cortical lines should show intact Lowell’s S-patterns (“lazy S”) in both views.
For more details, see the additional material on assessment of reduction quality.
Percutaneous reduction
If closed reduction is not satisfactory, carry out a percutaneous reduction technique.
Open reduction
If closed reduction fails, carry out an open reduction.
A two-window approach is most commonly used: reduction and preliminary fixation with reduction forceps through a Smith-Petersen approach and a separate lateral approach for implant insertion.
Alternatively, reduce and stabilize the fracture through an anterolateral (Watson-Jones) approach. Reduction maneuvers and visualization can be more difficult through this approach.
After the capsulotomy is performed, apply traction on the limb and manipulate the head and neck with hooks or K-wires, which can be inserted to act as joysticks until an anatomical reduction is achieved.
Confirm the reduction with the image intensifier.
Temporarily stabilize the fracture with K-wires.
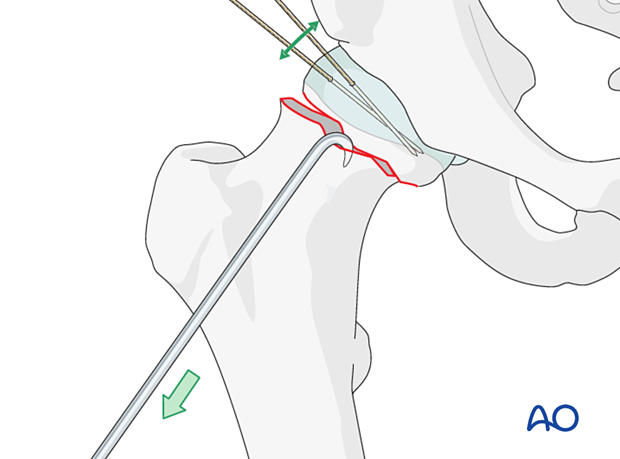
Alternatively, insert a Schanz screw through the lower part of the greater trochanter. This allows for traction and rotation of the distal fragment.
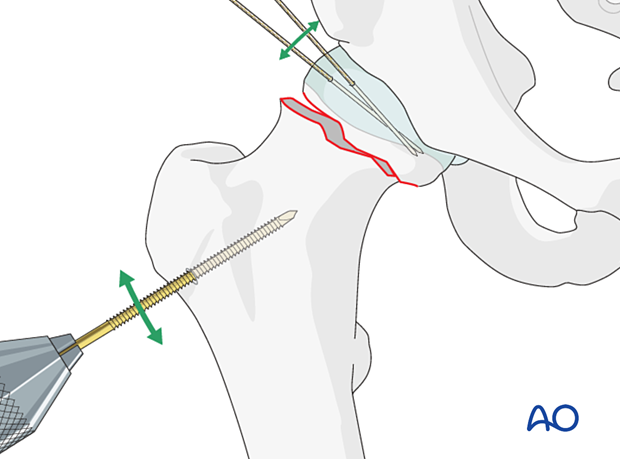
Insert two to three K-wires parallel to the head-neck axis for preliminary stabilization.
4. Approach for implant insertion
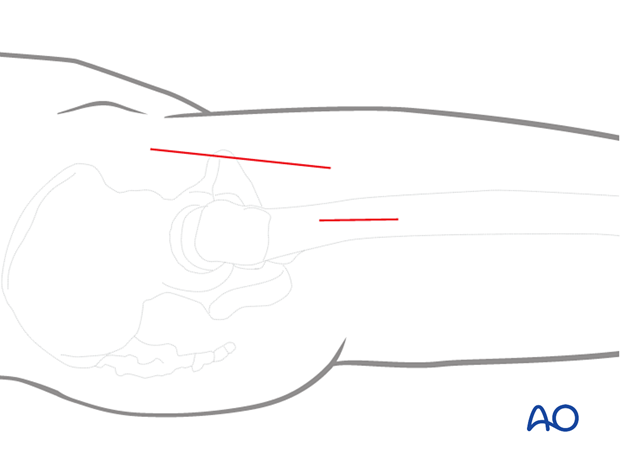
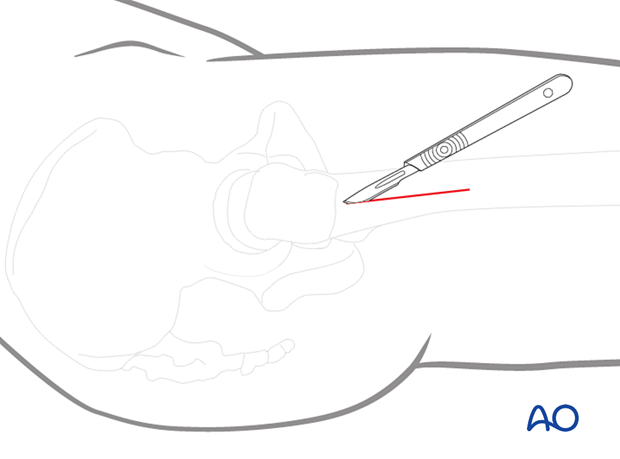
If the reduction has been performed in a closed or percutaneous manner, perform a limited lateral approach with an incision large enough for screw insertion. It should start at the vastus ridge extending about 5 cm distally.
5. Fixation
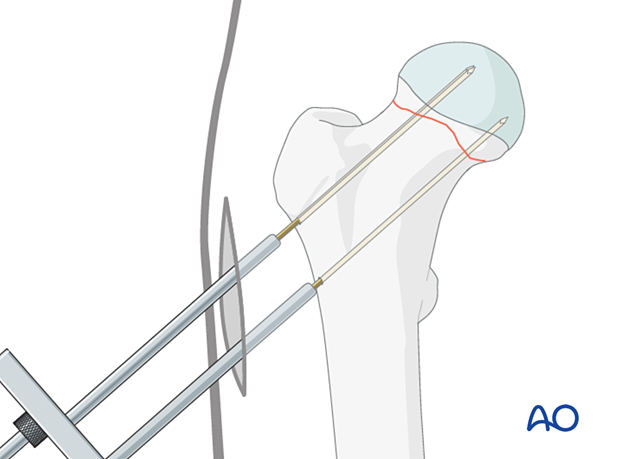
Guide-wire insertion
Insert the guide wires freehand under image intensifier control to ensure they are parallel to the head-neck axis and each other, or with an aiming device if available.
If K-wires have been used for provisional fixation, identify the K-wire with the optimal track in both views and introduce other guide wires parallel to it.
Make sure the tip of each wire stops in the subchondral bone of the femoral head and does not penetrate into the hip joint.
Confirm correct wire insertion with image intensification in AP, lateral, and axial views.
If using an aiming device, expose the proximal femoral lateral cortex through an incision just large enough for the device.
The first wire may be placed along or within 3 mm of the endosteum of the proximal aspect of the medial neck. This provides a fulcrum for optimal three-point fixation (head-neck-lateral cortex) to resist postoperative varus displacement.
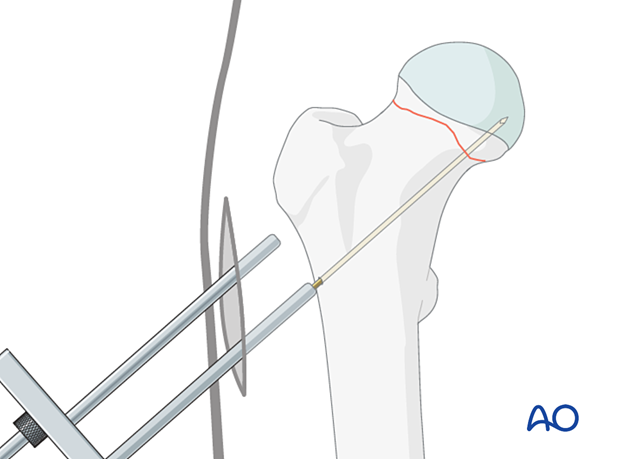
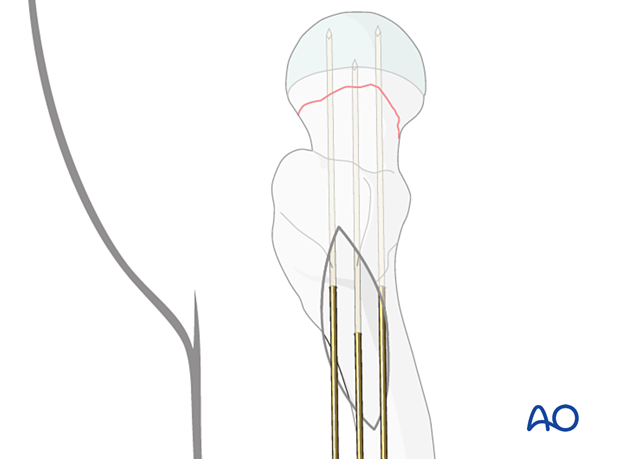
The two superior wires are then placed parallel to the first. Optimally, the posterior cortex of the neck must be within 3 mm of the posterior wire to minimize the risk of retroversion collapse.
Lateral view with the guide wires inserted
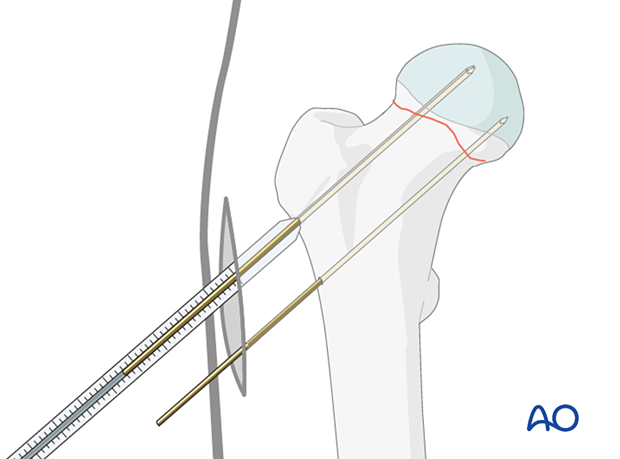
Determining the screw length
Determine the length of the screws with the aid of the measuring device.
Choose the length of the drill and screws 5 mm shorter than the length of the guide wires so that the screw tip will end 5 mm short of the subchondral bone.
The thread of the selected screws should not be across the fracture line.
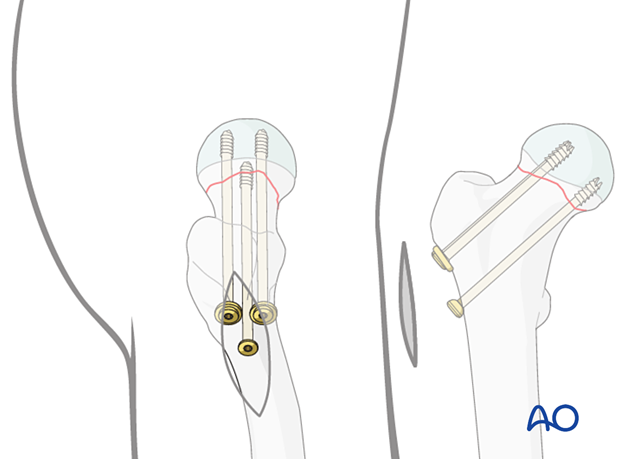
Insertion of the cannulated screws
To prepare the path for the core diameter of the screws, drill over the wires with a 3.6 mm cannulated drill bit. Then insert three 7.0 mm or 7.3 mm cannulated cancellous screws over the wires.
In younger patients with dense cancellous bone, the cannulated tap may be necessary to precut the thread.
Washers may be used with the proximal screws to avoid penetration of the screw head through the thin cortex of the greater trochanter.
The screws must be tightened carefully and repeatedly during the procedure. If a fracture table is used, traction must be released before screw tightening.
6. Final assessment
Obtain final x-rays in all views.
7. Aftercare
Postoperative mobilization
The elderly patient may start with weight bearing as tolerated with walking aids the day after surgery.
Initial restricted weight bearing is required for the young patient. This can be reassessed at 6 weeks.
Unrestricted range-of-motion exercises of the hip joint are allowed.

Pain control
To facilitate rehabilitation and prevent delirium, it is important to control the postoperative pain properly, eg, with a specific nerve block.
VTE prophylaxis
Patients with lower extremity fractures requiring treatment require deep vein prophylaxis.
The type and duration depend on VTE risk stratification.
Follow-up
Follow-up assessment for wound healing, neurologic status, function, and patient education should occur within 10–14 days.
At 3–6 weeks, check the position of the fracture with appropriate x-rays.
Recheck 6 weeks later for progressive fracture union.
Longer follow-up, at 6 months and 1 year, is indicated to assess the development of posttraumatic arthritis and/or avascular necrosis.
Implant removal
Removal of the internal fixation devices is performed only if they are prominent and thought to be the cause of painful irritation. If so, the implants should not be removed before fracture union. The surgeon and patient should be aware that after implant removal, risk of refracture exists.
Prognosis of proximal femoral fractures in elderly patients
For prognosis in elderly patients, see the corresponding additional material.













