ORIF - Spinopelvic fixation
1. Introduction
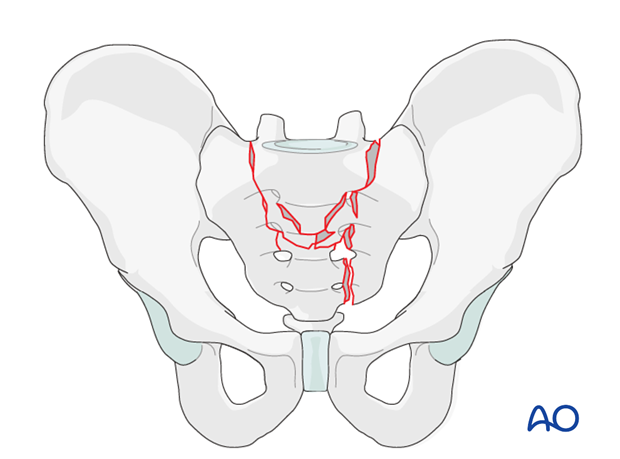
Lumbo-sacral dissociation is caused by high energy and is commonly associated with other fractures as well as neurological deficit.
It is typically a hyper-flexion injury where the sacrum is fractured bilaterally in the vertical plane and horizontally in the vestigial disk space of S1-S2 or less frequently on S2-S3 level.
It is essentially a sacral fracture which results in detachment of the lumbo-sacral spine from the pelvic ring.
The sacrum is the lowest part of the spine and the fracture has the characteristics of spinal fractures.
A multidisciplinary approach is highly advisable.
For the fixation, knowledge of both spinal and pelvis fixation techniques is necessary. In cases of neurological deficit, decompression of sacral nerve roots is mandatory.
The fixation should be strong enough to allow early mobilization; even for patients with neurological deficits.
In cases of large displacement, reduction is difficult and great care should be taken to avoid further damage to the neurological structures.
In slight or moderate displacement without neurological deficit, fixation in situ is recommended.
Spino-pelvic fixation allows a complete exclusion of the fractured sacrum from weight bearing.
The essence of this procedure is to provide a rigid fixation to protect healing, allow rapid mobilization and avoid pseudoarthrosis.
Some malunion can be accepted.
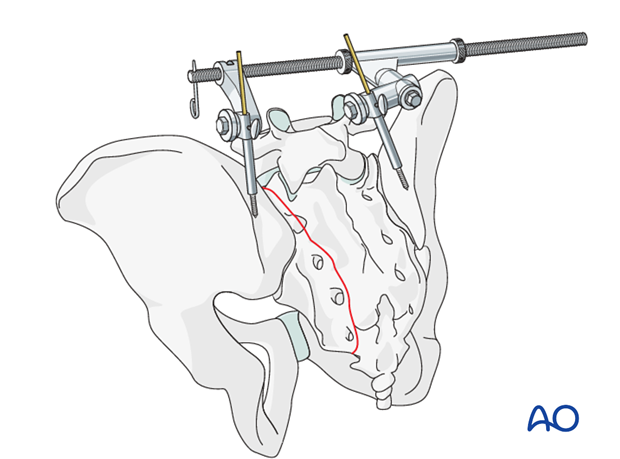
A flexion deformity is often present through the transverse fracture component. This may be corrected by hyper-extension of the hips, with manual traction. The patient is prone, with lateral sacral C-arm imaging
Manipulation of the fracture with the aid of iliac schanz screws can help with exposure for neural decompression and reduction. Laminectomy and removal or impaction of displaced bone fragments is recommended.
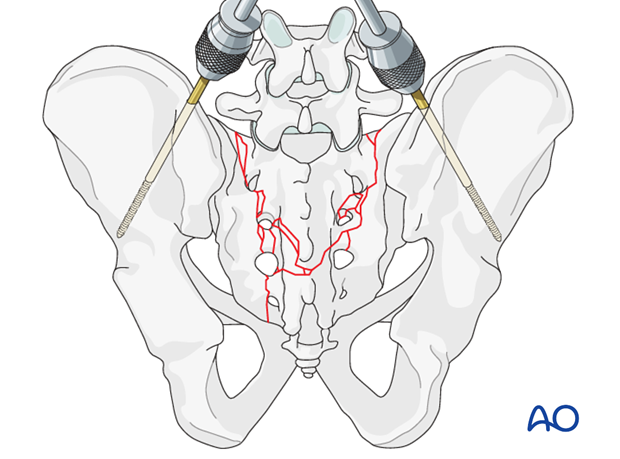
A distractor placed in the posterior iliac crests can open the fracture gap. It also provides a handle with which the pelvis can be lifted gently off the operating table, to correct flexion and axial impaction
2. Patient preparation and approach
Patient preparation
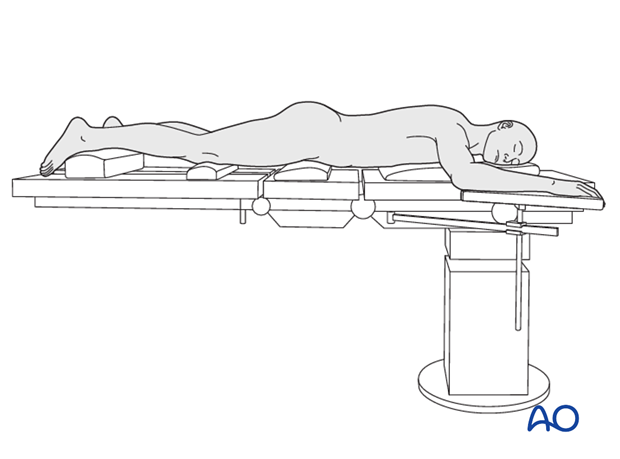
This procedure is performed with the patient in a prone position.
Approach
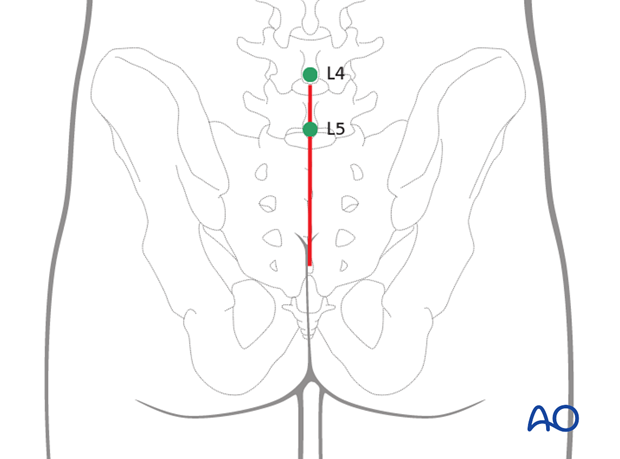
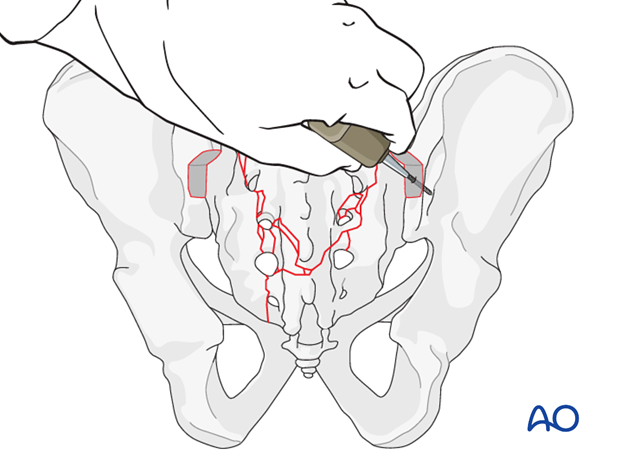
For this procedure a posterior approach to the sacrum is used.
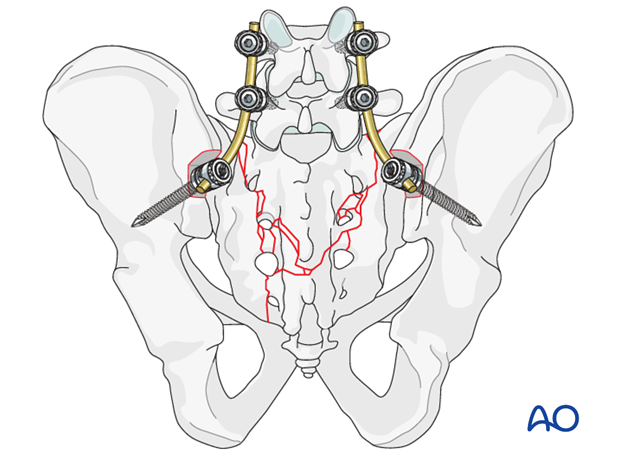
3. Insertion of the pedicle screws
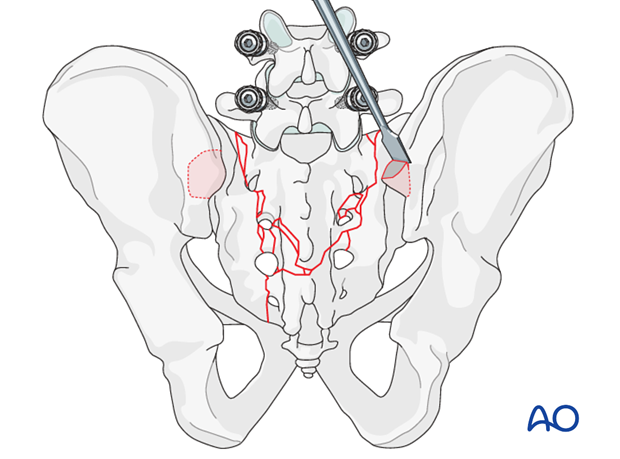
Pedicle screws are inserted in L4 and L5 and connected with the rod.
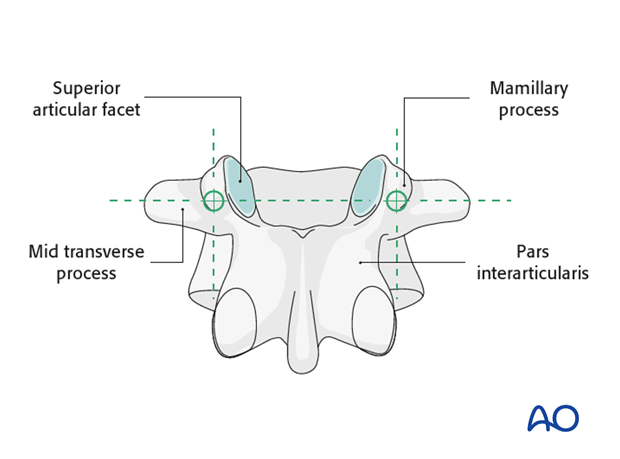
Pedicle screw entry points
The entry point of the pedicle screw is defined as the confluence of any of the four lines:
- Pars interarticularis
- Mamillary process (shown)
- Lateral border of the superior articular facet
- Mid transverse process (shown)
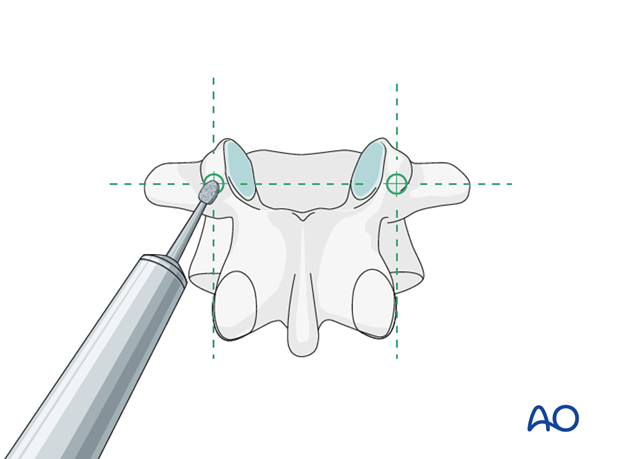
Opening of the cortex
Open the superficial cortex of the entry point with a burr or a rongeur.
Sagittal plane angulation
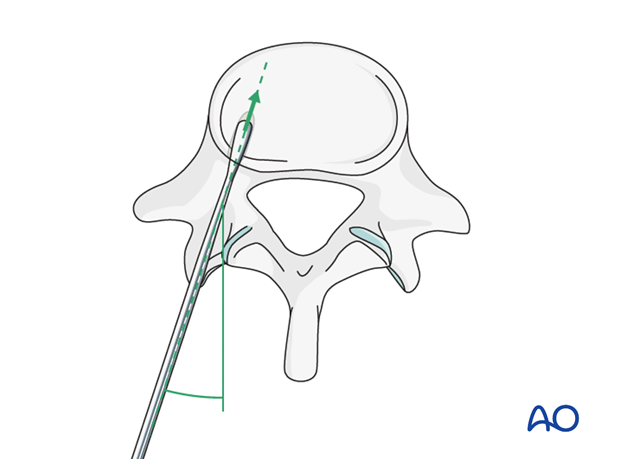
A pedicle probe is used to navigate down the isthmus of the pedicle into the vertebral body.
The pedicle probe should be inserted in a trajectory superimposed on the transverse process and parallel to the superior endplate.
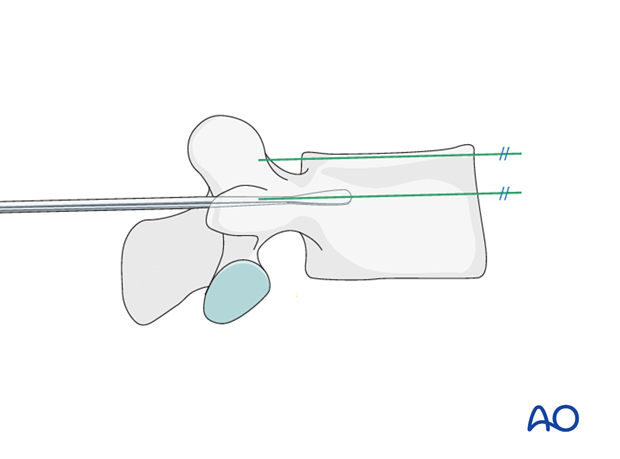
Transverse plane inclination
It is important to avoid medial penetration of the spinal canal superficially or lateral or anterior penetration of the vertebral body cortex at the depth of insertion.
Screw insertion
Once the pedicle track has been created, it is important to confirm a complete intraosseous trajectory by pedicle and body palpation using a pedicle probe. At any point in the process, radiographic confirmation can be obtained.
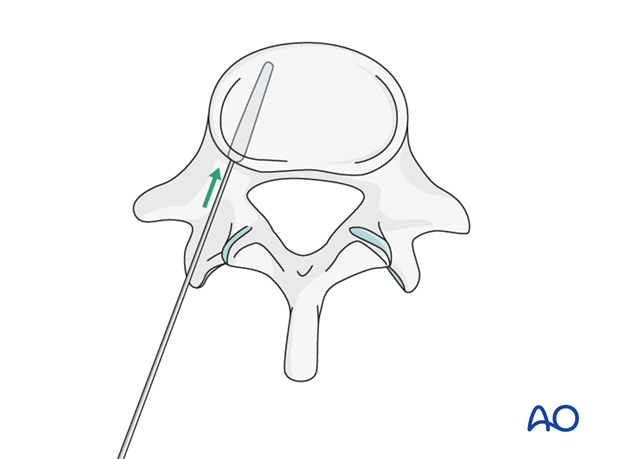
A screw of the appropriate diameter and length is carefully inserted into the prepared track.
4. Iliac screws
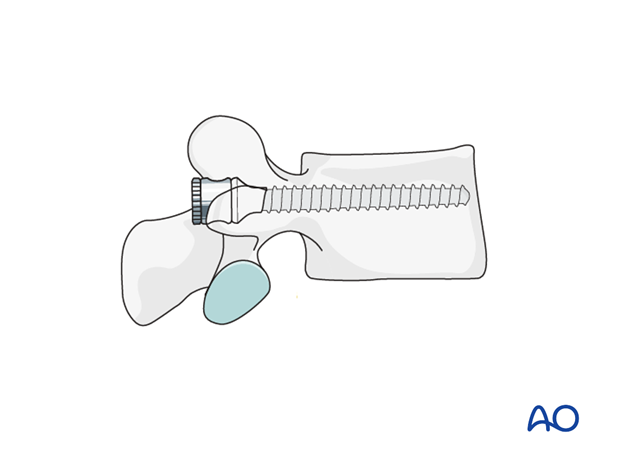
The iliac entry point is medial to the posterior iliac crest to prevent pressure ulcers over the implant.
1 cm3 of bone is removed with a chisel or a saw to recess the implant to the level of the posterior ilium, and thus avoid soft tissue irritation.
Both iliac attachment sites are prepared similarly.
An oscillating drill (3.5 mm) or awl is used to penetrate between the two cortices in a ventral, caudal direction.
When resistance is felt, the length is measured for the insertion of the pedicle screw.
The preferred diameter is 7.0 mm.
Use C-arm images to confirm appropriate screw location. A lateral view and one along the axis of the screw are required.
5. Vertical reduction
Insertion of the connection rod
It is important that the iliac screw heads and connecting rods lie flush to the bone. Avoiding prominent hardware prevents soft tissue irritation.
A template rod could be used to get the shape and length for in situ fixation.
Contouring of the rod may be difficult because of the individual anatomy.
Cut the permanent rod to the appropriate length. Attach it to the screw per the hardware system.
Additional contouring of the rod may be necessary to achieve indirect reduction. This might consist of both under and over bending.
The final rod is prepared and attached to the pedicle screws bilaterally.
The construct should be further stabilized by the insertion of 1-2 transverse connectors at the level of the sacrum.
Resection of any small bony prominence may allow the assembly to lie close to the bone.
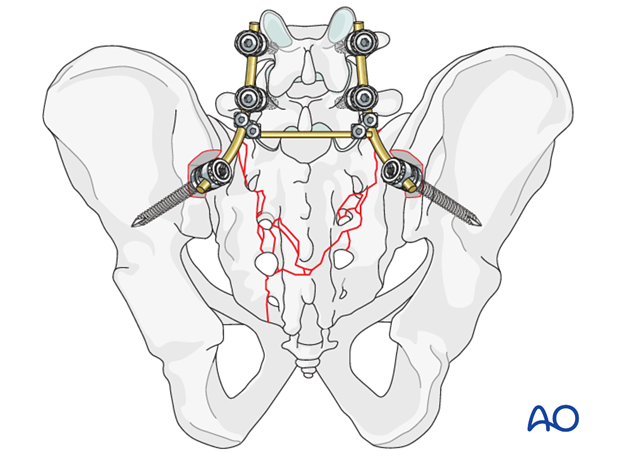
6. X-rays
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.

7. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













