ORIF - Ilioiliac plate
1. Introduction
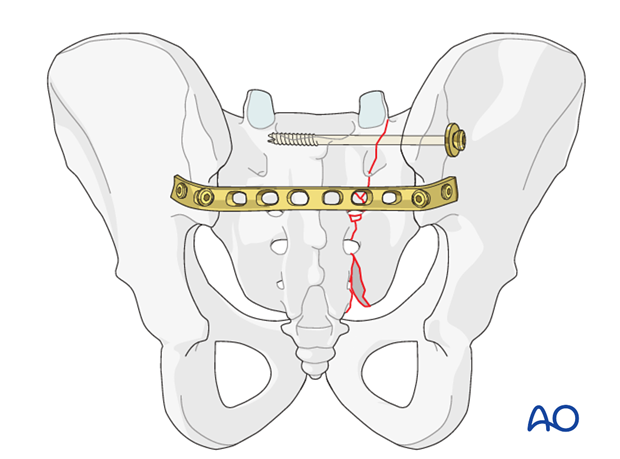
Posterior fixation of displaced sacral fractures is frequently enhanced by the use of transiliac plate fixation. This is usually an adjunct to transiliac sacral screw fixation but some constructs can be used as stand-alone alternatives.
This form of fixation is especially advantageous in cases of large comminuted zones to bridge the comminuted zone.
Two basic types of plate utilization are possible:
- Neutralization plate as an adjunct to one or more transiliac sacral screws
- Solitary bridging fixation which typically requires a stronger plate in combination with fixation through the plate to the sacrum
Plating variations
There are two commonly anatomic variations for plate placement:
- Plate between the interspinous zones of the ilium, either anterior or posterior to the paraspinal muscles.
- Submuscular at the level of S2 bridging to the innominate bones just cranial to the greater sciatic notch.
2. Patient preparation and approach
Patient preparation
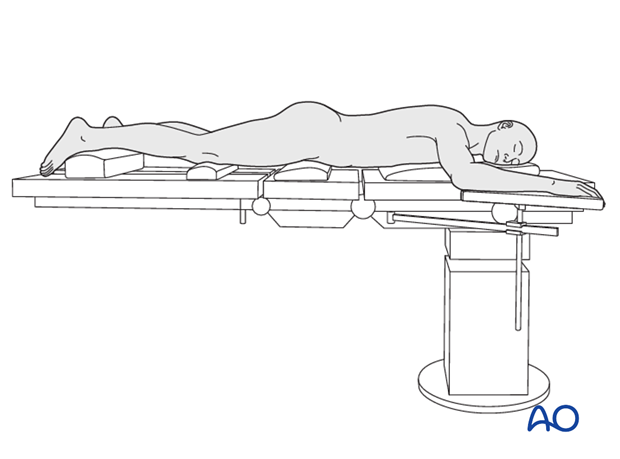
This procedure is performed with the patient in a prone position.
Approach
For this procedure a posterior approach to the sacrum is used.
3. Reduction
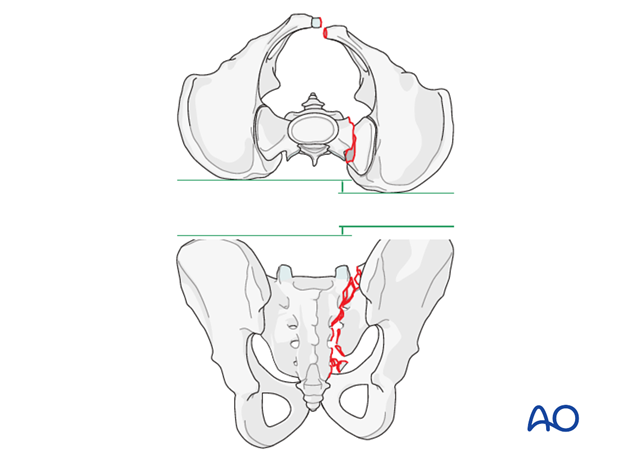
The typical displacements are cranial and posterior together with sagittal plane rotation.
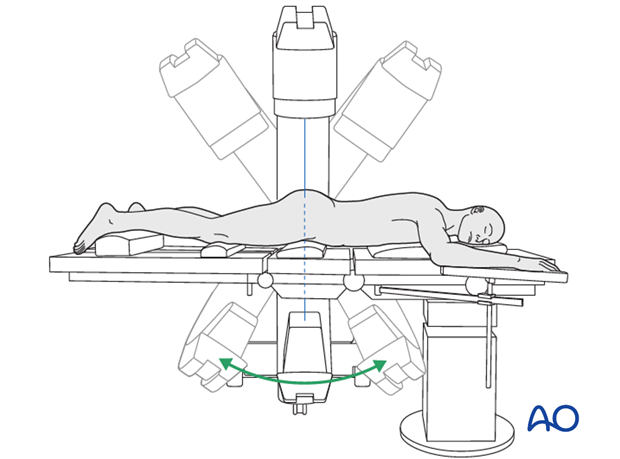
Prior to starting the procedure fluoroscopic AP, inlet and outlet x-rays should be obtained to ensure adequate visualization.
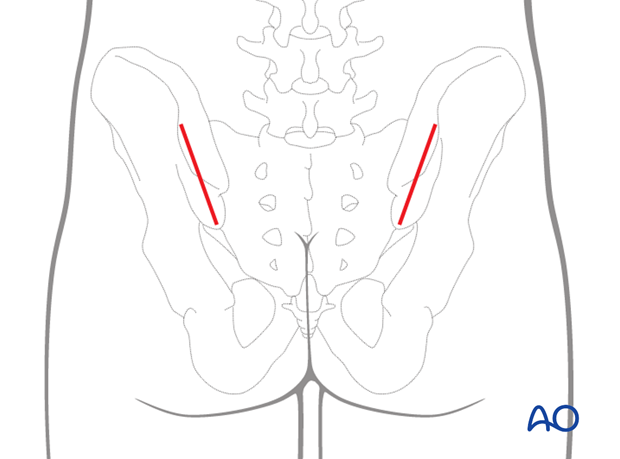
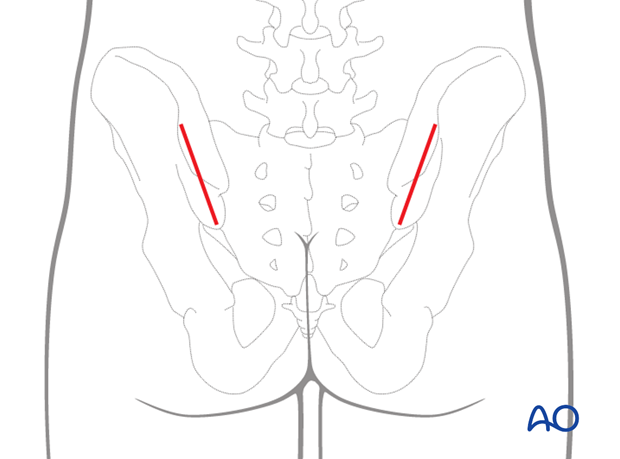
Two vertical contralateral incisions are made over the iliac crests which provide access for the fixation of the plate in both iliac wings.
Preliminary fixation
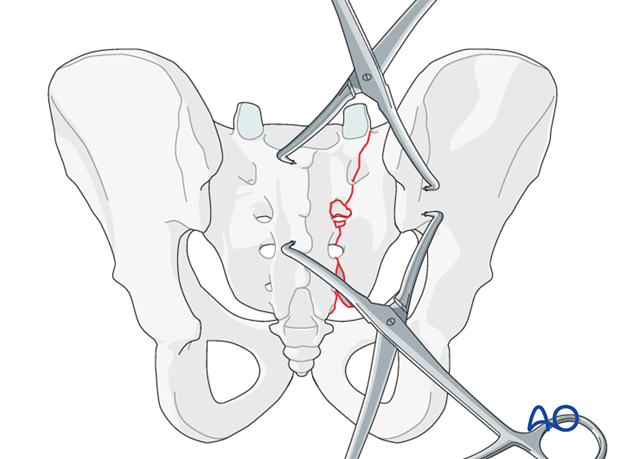
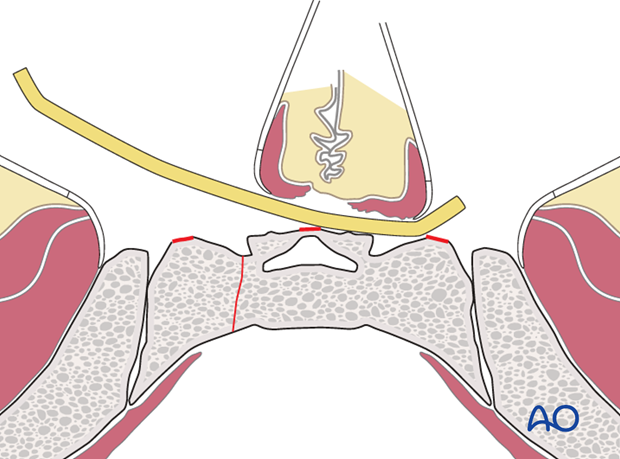
The primary reduction maneuver typically involves the use of two pointed reduction forceps (Weber clamps).
These span from the spinous process to the lateral ilium and are used to obtain a reduction incrementally by alternating translation and clamping.
Additional reduction techniques
Fix the anatomic reduction with pointed reduction forceps.
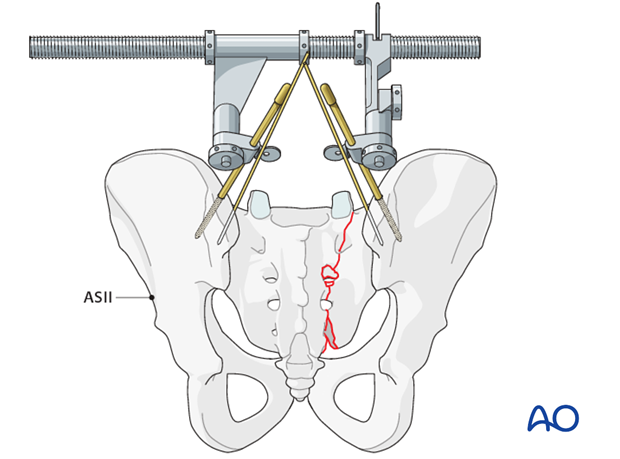
If needed, insert Schanz screws to both posterior iliac crests as a reduction aid for better rotational alignment.
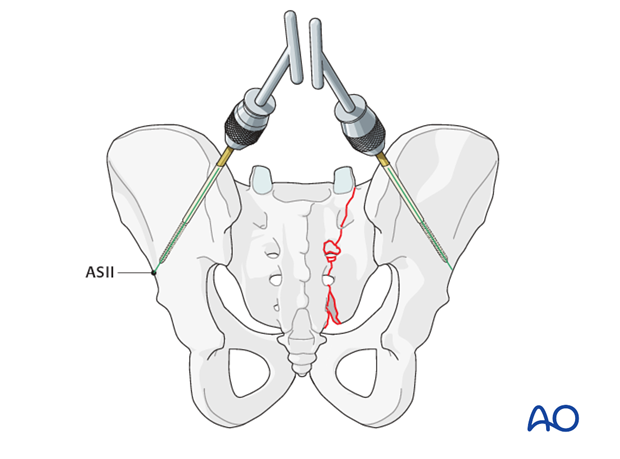
The AO distractor may be used as a distraction aid.
K-wires may be placed into the SI joints in order to determine the joint orientation.
4. Neutralization plate
After reduction and initial iliosacral screw placement, a plate is added to neutralize deforming forces, particularly distraction. This has traditionally been thought of as a “tension band” plate, although recent research questions this.
More information on the tension band principle can be found here.
Remove the tip of the spinous process of (S2/S3) if it is in the way of the plate.
Use a small chisel if the approach with two vertical incisions is performed.
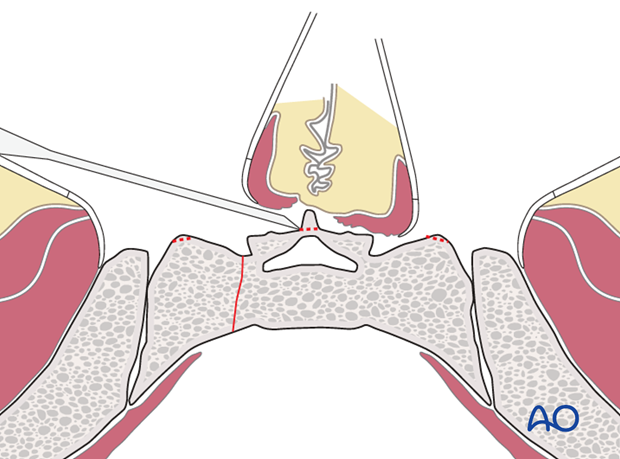
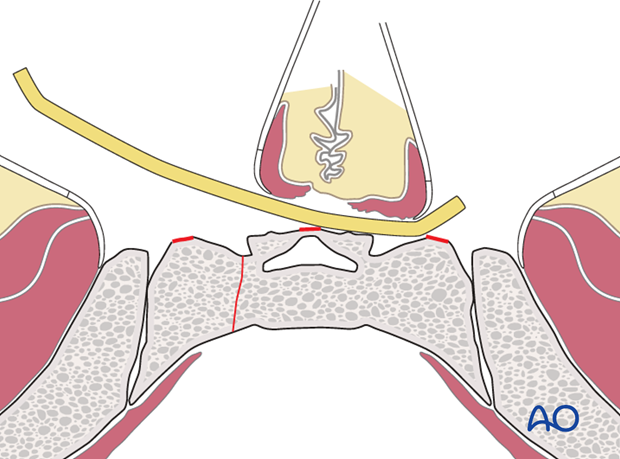
Apply the contoured plate onto the fracture site by sliding it underneath the paraspinal muscles. The plate is turned 180° along its axis to facilitate insertion.
The initial screws are inserted into the sciatic buttress and sequentially tightened to compress the plate against the ilia.
The advantage of this anatomic location is the additional fixation provided by longer screws into the densest bone in the ilium.
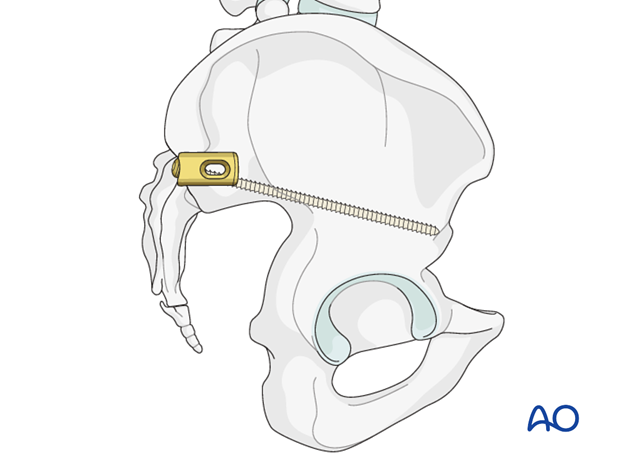
The ends of the plate are then contoured in situ and additional short screws, which may or may not cross the IS joint, are inserted into the innominate bone.
5. Alternative fixation technique
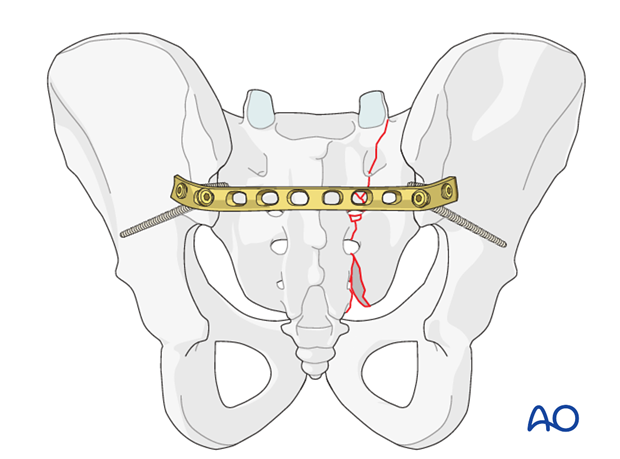
Achieve posterior fixation by applying a contoured 4.5 mm DC-plate.
Choose the plate long enough to reach from one iliac wing across the sacrum to the opposite ilium.
Use a short bending template to determine the correct shape of each side. Then bend the ends of the plate to fit.
The plate crosses the sacrum in the midline of the second and third sacral foramen.
When applied, the plate should reach over the posterior inferior spines providing space for fixation with at least two additional screws (3-4 screws if needed).
Remove the tip of the spinous process of (S2/S3) if it is in the way of the plate.
Use a small chisel if the approach with two vertical incisions is performed.
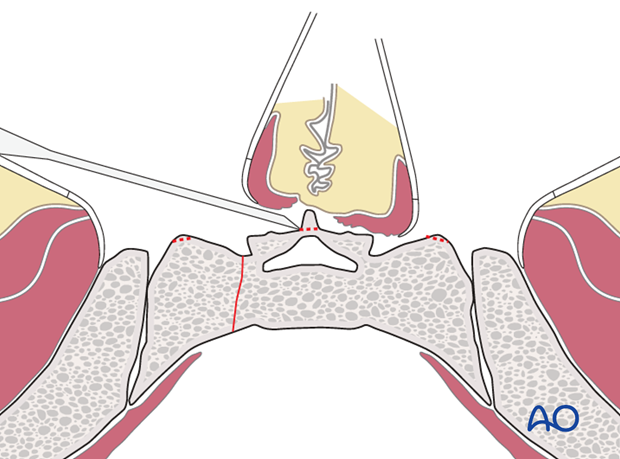
Apply the contoured plate onto the fracture site by sliding it underneath the paraspinal muscles. The plate is turned 180° along its axis to facilitate insertion.
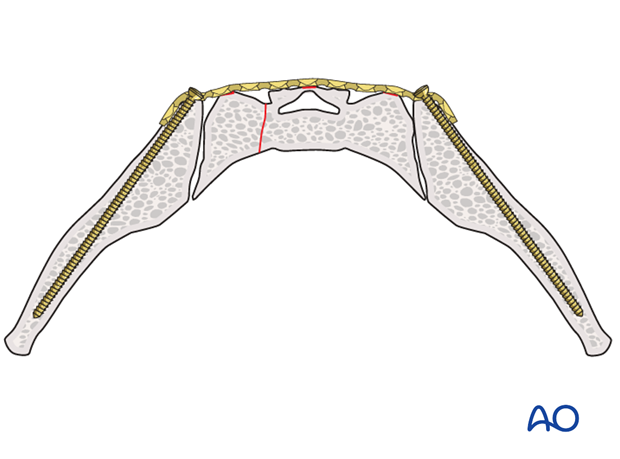
The plate will be attached to the ilia with screws inserted between the two iliac cortices.
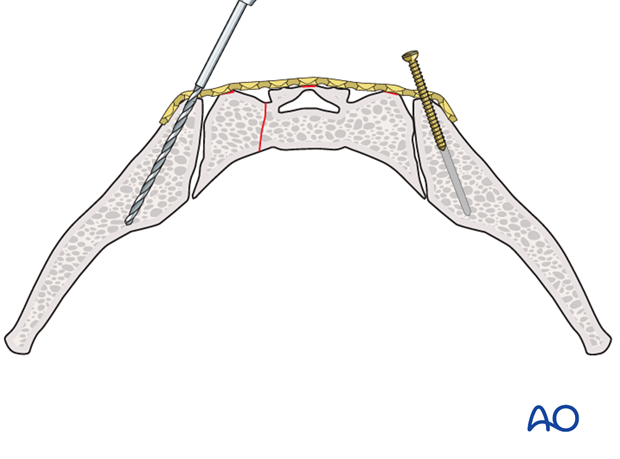
Start fixing the plate to the uninjured (contralateral) side by using a 3.2 mm drill bit in the direction of the two iliac cortices. Stop drilling when you reach cortical resistance.
After measurement, insert a 4.5 mm screw. Screw length is typically 50-60 mm.
Repeat this on the injured side.
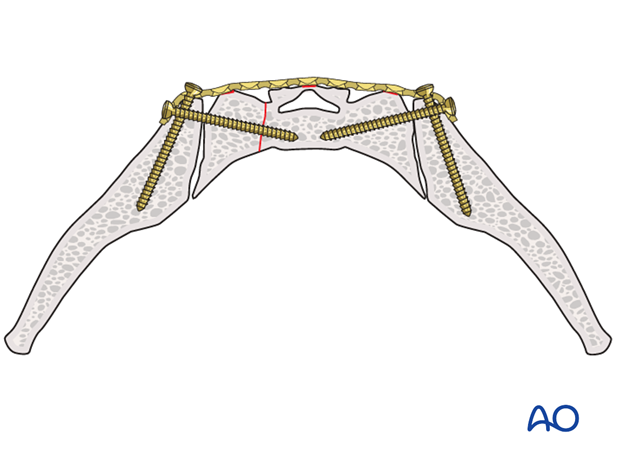
Tighten the screws sequentially before applying the second pair of screws.
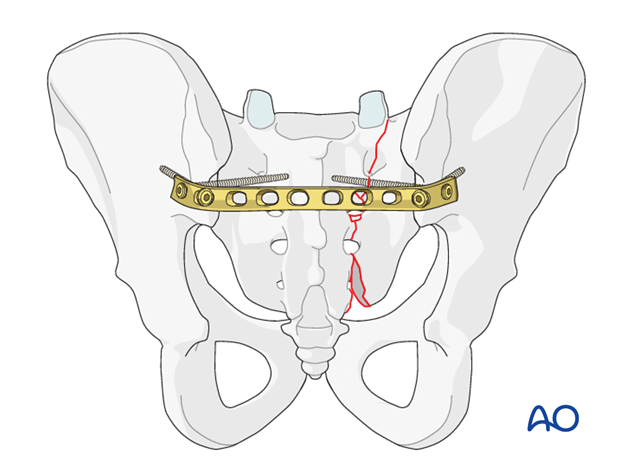
For the second screw on each side, which will cross the SI-joint into the sacrum, aim medially and cranially with the drill bit (outer half sacral ala).
Two 4.5 mm screws of correct length is inserted through each end of the plate.
Note
If applicable, apply additional screws into the “save zones” of the sacrum, to increase the stability of the whole “construction”.
6. Alternative plate and screw fixation
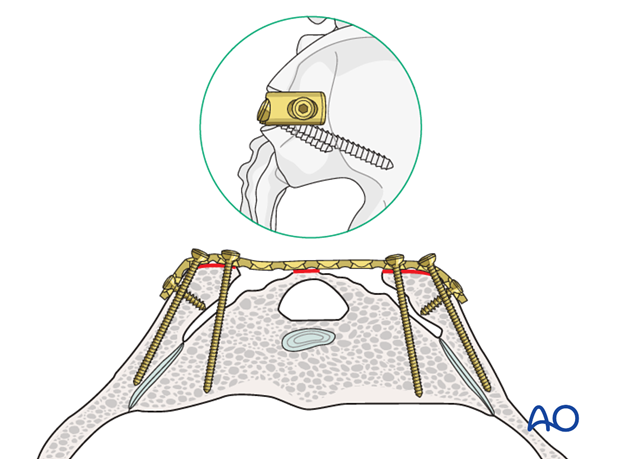
Transverse plating at the level of the posterior superior iliac spine can be made less prominent by creating a bony notch for seating the plate. Screw placement in this location usually is into the pedicle of S1 and between the tables of the ileum.
7. Additional stability
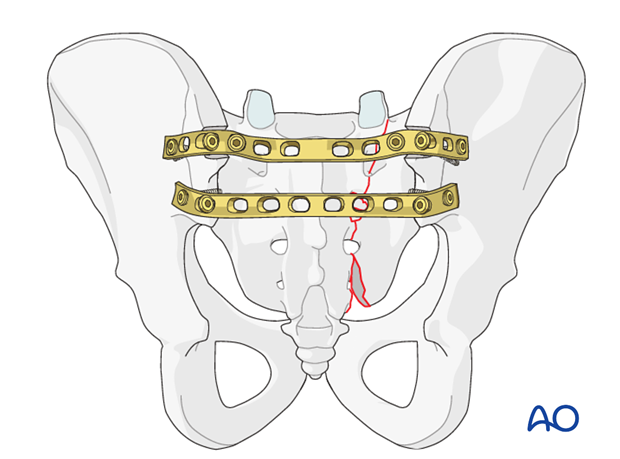
In case of a very comminuted fracture, the placement of two plates will give additional stability.
Make a trough in both iliac crests at the level of S1, deep enough so that the plate lies on the sacrum.
8. X-rays
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.

9. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













