ORIF Plate
1. Introduction
Transverse lower sacral fractures with displacement may injure sacral nerve roots. If perineal sensation or sphincter tone is abnormal, surgical decompression may be indicated. This could involve laminectomy, and if deformity is significant, reduction and fixation of the sacral fracture.
Otherwise, ORIF is indicated for correction of severe deformity or as part of management for open fractures.
Plate fixation of transverse sacral fractures must be performed posteriorly and typically involves the use of two small plates.
The exposure is obtained through a posterior midline sacral approach with the patient in a prone position.
2. Preparation of the fracture site
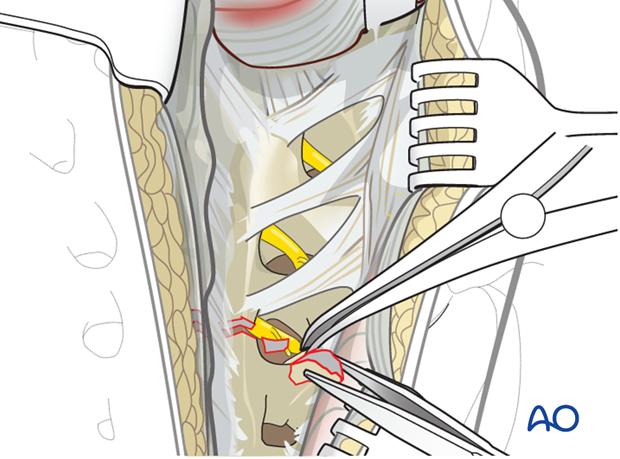
Expose the entire fracture line. Identify and remove small bony fragments from the fracture zone. They may be located in the transforaminal region and hinder fracture reduction.
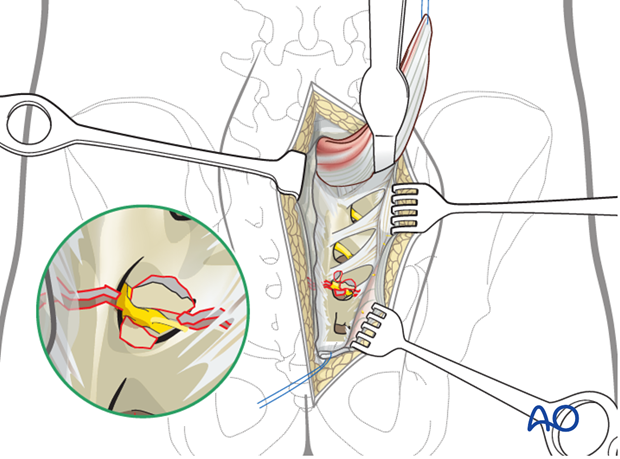
Sacral nerve root decompression
The complete fracture line has to be cleaned out and inspected.
Enhance the exposure by using a lamina (bone) spreader, and carefully placed bone hooks.
Extract bone fragments that may compromise the sacral nerve roots. Fracture reduction may be required to Realign the sacral vertebral canal and restore anterior clearance for the neural elements.
3. Reduction
The typical displacement is flexion with possible anterior translation of the distal fragment.
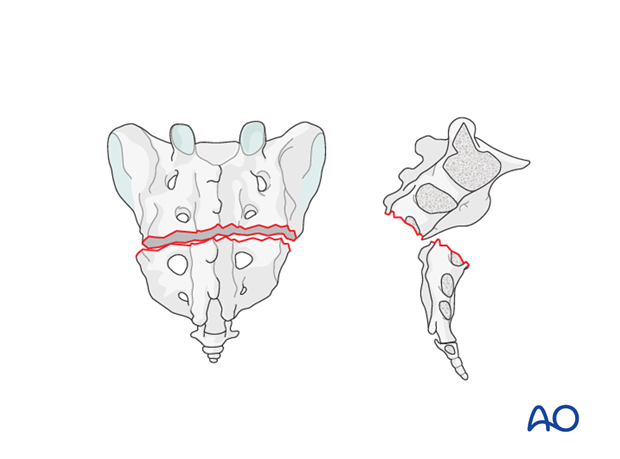
Preliminary fixation
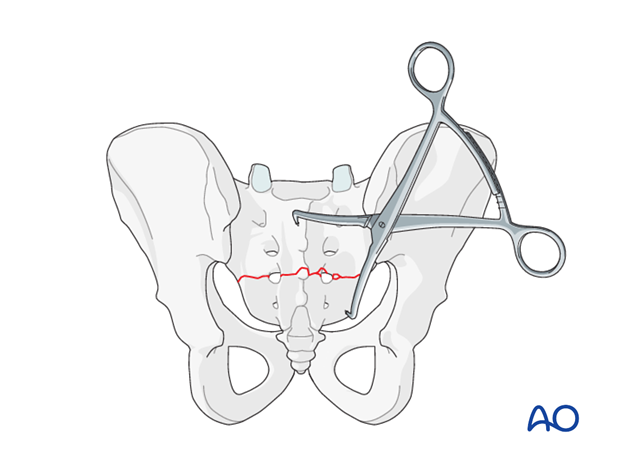
The primary reduction maneuver typically involves the use of two-pointed reduction forceps (Weber clamps).
The distal fragment is grasped and pulled distally to permit reduction. Small elevators can be used laterally to assist.
Once reduced, the distal fragment is clamped to the proximal with pointed reduction forceps.
4. Planning of the internal fixation
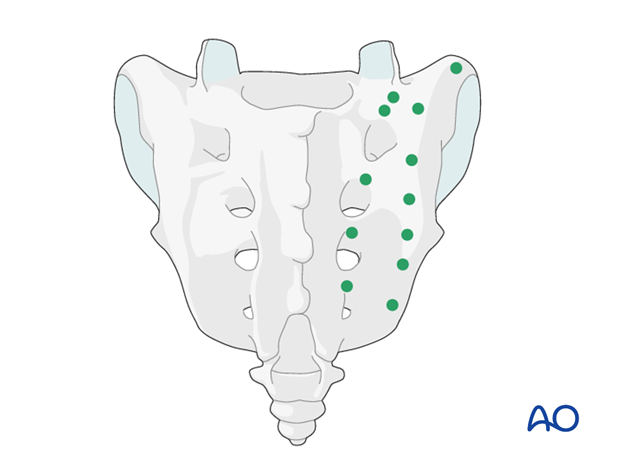
Entry points for sacral screw fixation
Safe placement of screws avoids the spinal canal and sacral nerve root channels by using the illustrated lateral entry points proximal and distal to the fracture bilaterally. This is lateral to the sacral foramina and nerve roots, or between and in line with the sacral foramina.
5. Plate application
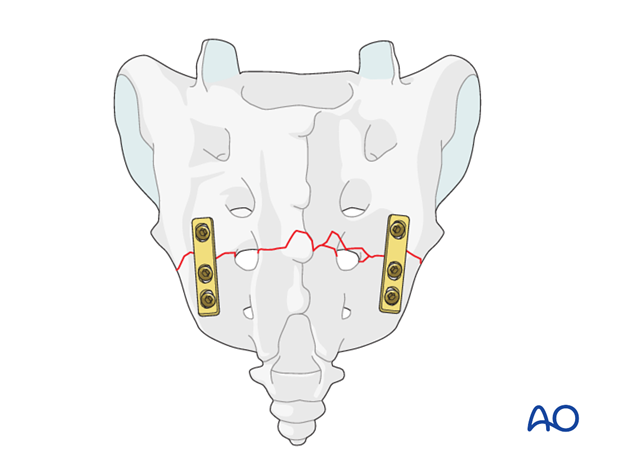
Plate fixation
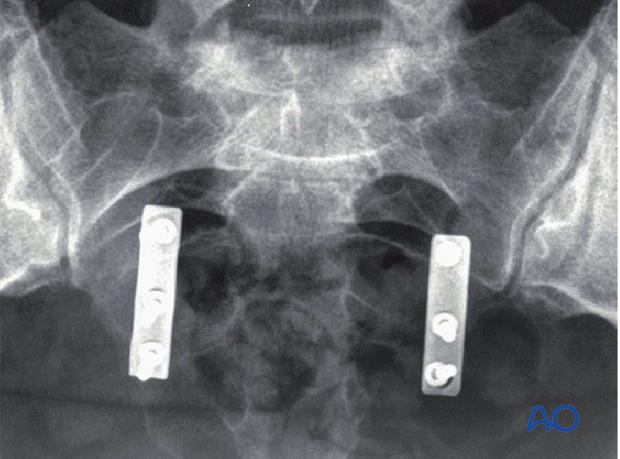
Fixation is performed with two (bilateral) small fragment plates (4-6 holes).
6. X-ray control
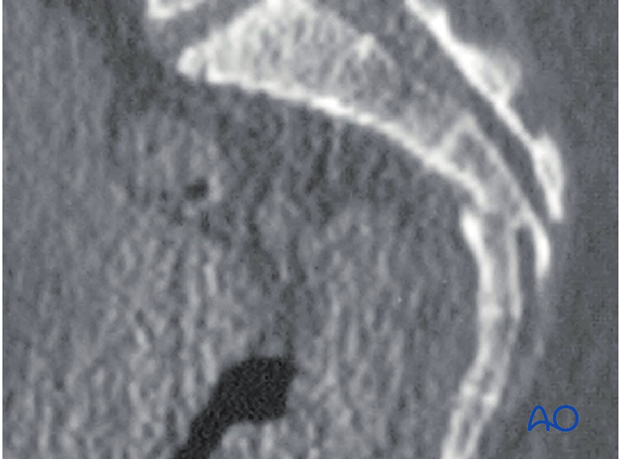
Preoperative lateral CT-view.
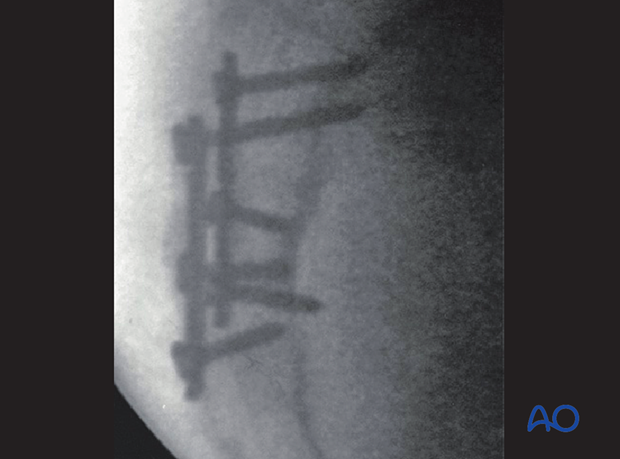
Postoperative lateral X-ray view
Confirm satisfactory reduction and hardware placement on AP & lateral views.
Postoperative AP X-ray view.
7. Aftercare following open reduction and fixation
Postoperative blood test
After pelvic surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Bowel function and food
After extensile approaches in the anterior pelvis, the bowel function may be temporarily compromised. This temporary paralytic ileus generally does not need specific treatment beyond withholding food and drink until bowel function recovers.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary.
Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises.
For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
In unstable unilateral pelvic injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 week but use of crutches may need to be continued for three months. It should remembered that pelvic fractures usually heal within 6-8 weeks, but that primarily ligamentous injuries may need longer protection (3-4 months).
Fracture healing and pelvic alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable pelvic fractures
Extra precautions are necessary for patients with bilaterally unstable pelvic fractures. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair. For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













