Suture repair
1. Principles
The reattachment of such a strong soft-tissue structure as the patellar tendon to the inferior pole of the patella, requires a technique which not only achieve an excellent suture hold in the tendon, but also preserves its vascularity. The Krackow suture realizes these goals.
2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position with the knee flexed 30°.

Approach
For this procedure a mid-axial longitudinal approach is used.

3. Reduction and fixation
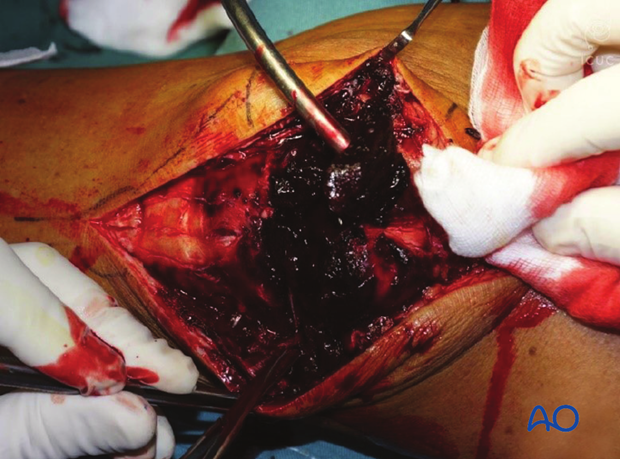
Fracture debridement
The knee joint and fracture lines must be irrigated and cleared of blood clots and small debris to allow exact reconstruction.
An image intensifier should always be available so that the final result can be checked in the AP and lateral planes.
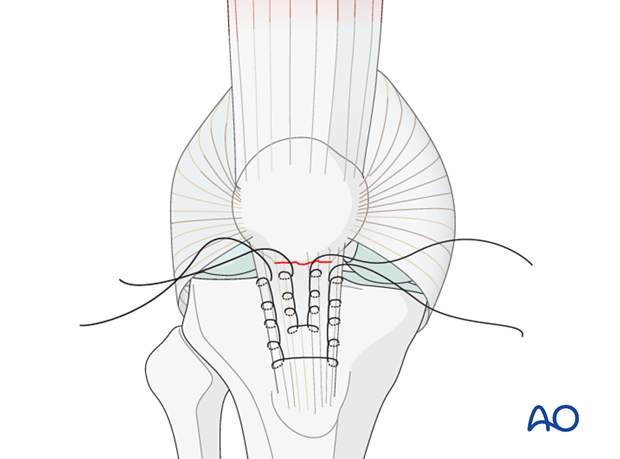
Krackow whip stitch
The Krackow whip stitch uses 2 or more locking loops inserted into each side of the patellar tendon. The Krackow whip stitch is stronger than the Kessler, or Bunnell, stitches that are used for repairing smaller tendons.
Open the patellar tendon retinaculum longitudinally. Insert two Krackow stitches of #5 non-absorbable suture into the patellar tendon, as illustrated.
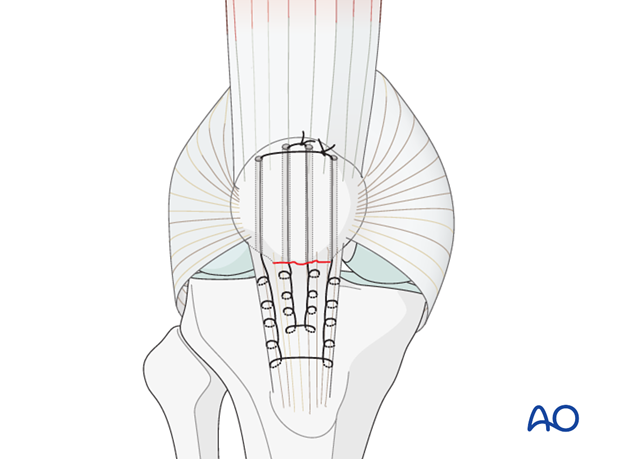
Make holes in the main fragment
Make 4 longitudinal drill holes in the proximal patellar fragment.

Ligament fixation
Using a suture passer from proximal to distal, pull the free ends of the sutures through the proximal segment.
The sutures are then tightened and tied deep to the quadriceps tendon, with the knee in full extension.
Be sure that there is good contact between the tendon and the bone.
Augmentation of patella ligament tendon repair - patella baja
To protect this suture repair during the healing process, a protective cerclage wire can be passed around the upper pole of the patella and through a transverse drill hole at the tibial tubercle.
This wire frequently breaks later, and it is best to remove it once healing is assured at 3-4 months.
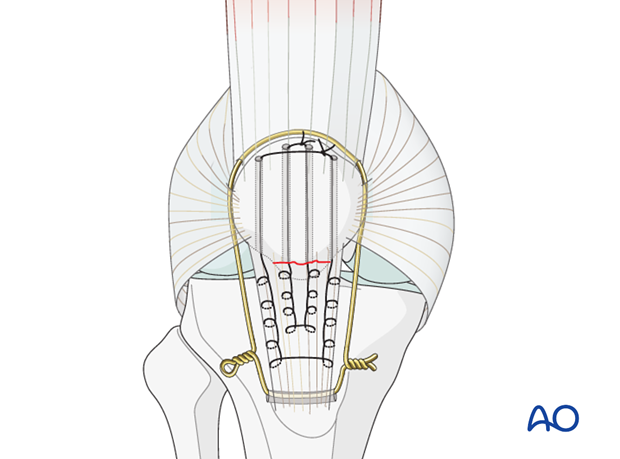
If the cerclage wire is tightened too tightly it will not be possible to flex the knee and a patella baja will occur.
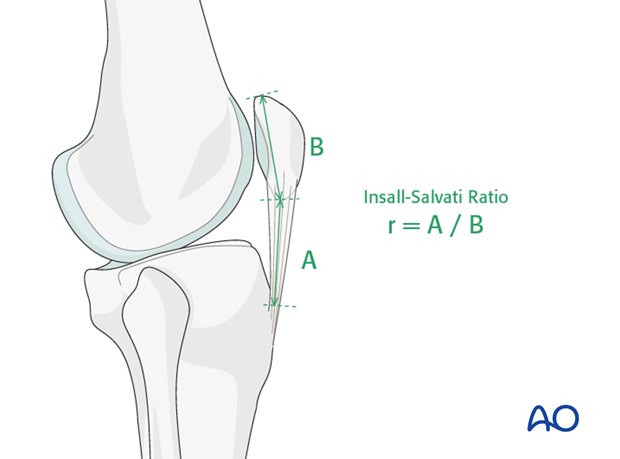
This complication must be avoided and can cause severe limitation of knee flexion. If there is need for a cerclage wire to protect the patellar tendon, a patella baja can be produced by misjudging the exact length of the patellar tendon. The opposite knee will indicate the correct position of the patella as described under x-ray evaluation.
4. Aftercare following Krackow whip stitch fixation
Introduction
Active knee function requires an intact knee extensor mechanism, a mobile patella, a well-preserved patello-femoral joint and muscle strength. Knee stiffness and muscle weakness can become a problem after the necessary period of knee extension splinting. Once deemed to be healed, a regimen of progressive knee mobilization and muscle strengthening must be supervised closely by the rehabilitation team.
Functional treatment
Patellar tendon suture is not completely stable. Aftercare follows in general the principle of tendon suture repair. At the time of surgery, the surgeon determines how much flexion the repaired knee can tolerate. A knee extension splint or hinged knee brace is then used to protect the knee from flexion beyond this. For example, the surgeon may determine that the repair is stable to a 100 degrees. Then a hinged knee brace with an arc of motion of 0-90 degrees would then be used for 4-6 weeks and would be slowly increased.
Weight bearing
Full weight bearing with the knee in full extension is theoretically possible immediately.
Follow-up
Wound healing should be assessed regularly within the first two weeks. X-rays should be taken at 2, 6 and 12 weeks. A longer period may be required if the fracture healing is delayed.
Thrombo-embolic prophylaxis
Consideration should be given to thrombo-embolic prophylaxis, according to local treatment guidelines.













