Fusion
1. General considerations
Goal of surgery
The main goals of the surgery are to restore the length and stability of the medial column without compromising the blood supply of the cuneiform.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

Maintenance of column length and relationship
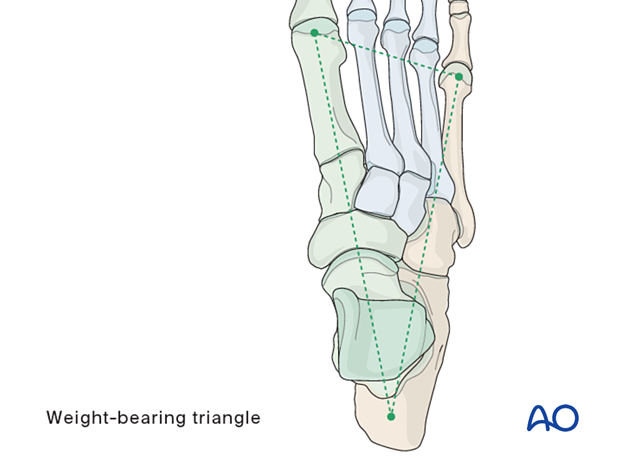
The foot’s form and function depend on the normal relationship between the medial and lateral columns.
If the cuneiform injury has resulted in comminution with loss of length, reconstruction must restore length and normal geometry.
Relative shortening of the medial column leads to cavus, whereas relative shortening of the lateral column leads to flat foot.
Essential versus nonessential joints
The essential joints of the hind and midfoot are the talonavicular, calcaneocuboid, and subtalar joints. Loss of motion in any of these joints will limit the movement of the other two and result in loss of complex hindfoot circumduction.
The tarsometatarsal joints and the naviculocuneiform joint are nonessential for hindfoot motion and can be fused if they cannot be reconstructed.

Primary fusion may be performed for the first tarsometatarsal joint or the naviculocuneiform joint. We will here demonstrate the fusion of the first tarsometatarsal joint.
2. Temporizing measures
Medial and lateral external fixation (with a distractor device to restore columnar length) should be applied as soon as possible to stabilize the foot and decrease further injury to the soft tissues.
Temporary percutaneous K-wires can be used to reduce displaced fragments and are left as temporary fixation.
3. Patient preparation and surgical approach
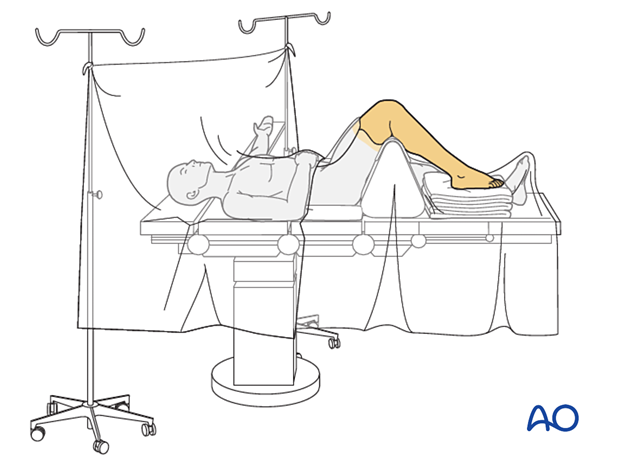
The procedure is performed with the patient placed supine with the knee flexed 90°.
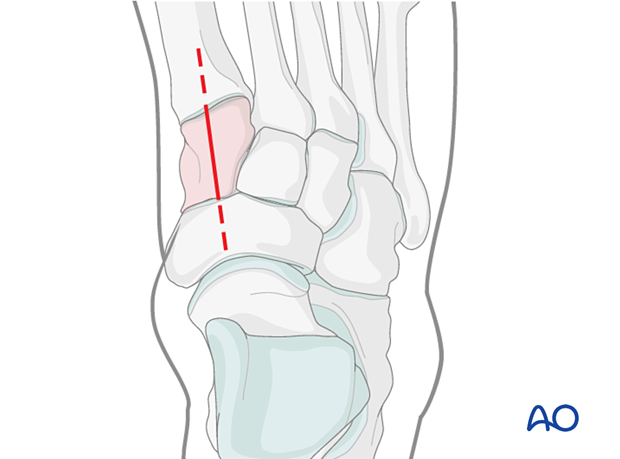
For this procedure, either a dorsomedial approach and/or medial utility incision can be used.
Due to the high-energy injury of these fractures, the soft tissues, including capsule and periosteum, are disrupted. Care should be taken to minimize soft-tissue stripping during the approach. This will help maintain blood supply to the fragments.
4. Visualization
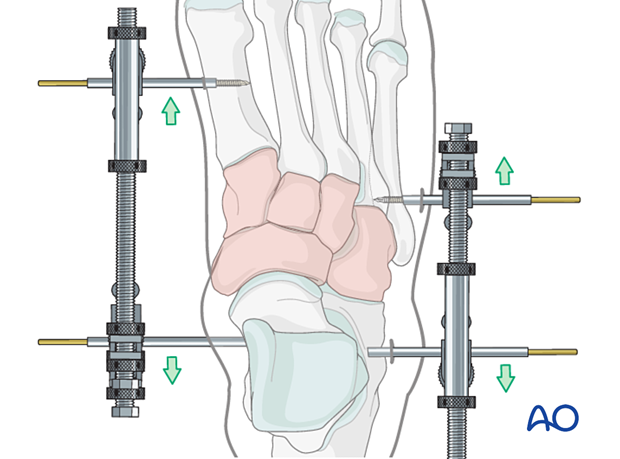
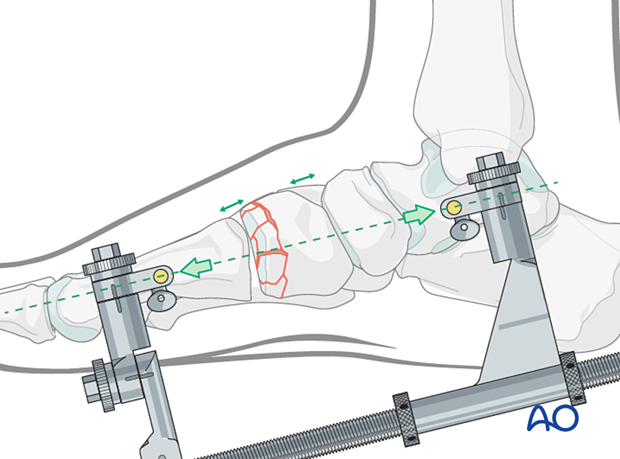
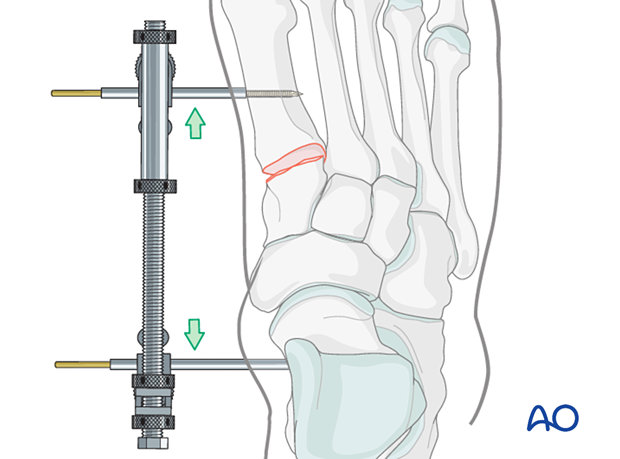
Use a medial-column distractor to achieve the articular surface visualization needed for accurate reduction and fixation.
Distraction is essential when dealing with comminution or a delay between the injury and the definitive reduction.
The proximal pin is inserted into the neck of the talus through a stab incision. Image intensification can be used to ensure correct pin placement outside the articular surfaces. The correct insertion point is often located 1–2 cm posterior to the navicular tubercle.
The distal pin is inserted in the midshaft of the first metatarsal.
The distraction vector needs to be in line with the talus and the first metatarsal in the medial plane.
5. Preparation for the joint for fusion
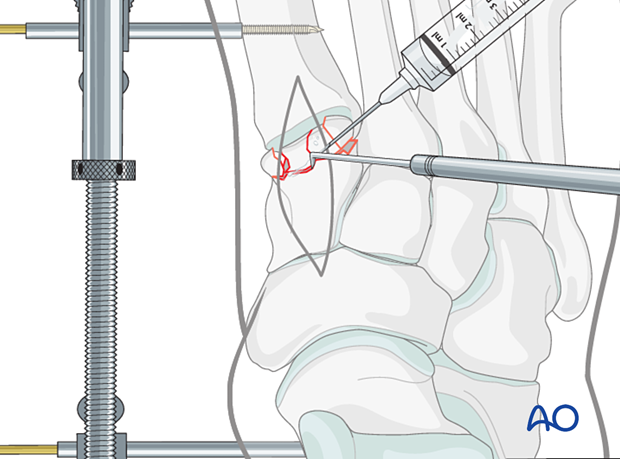
Irrigation
Irrigate the fracture using a syringe.
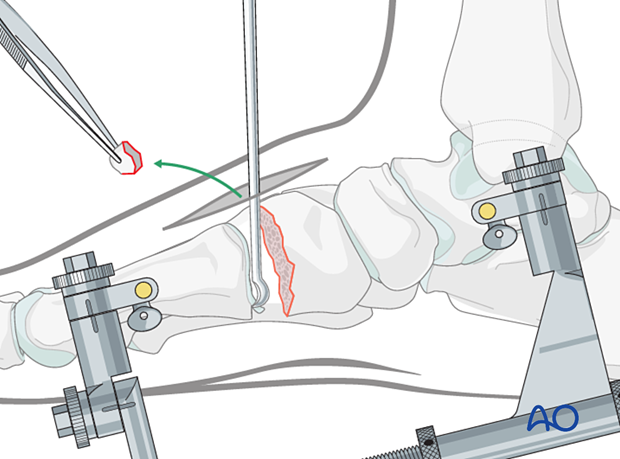
Preparation of the joint
Remove any osteochondral fragments from the joint.
Remove the cartilage of the opposing joint(s) using a curette.
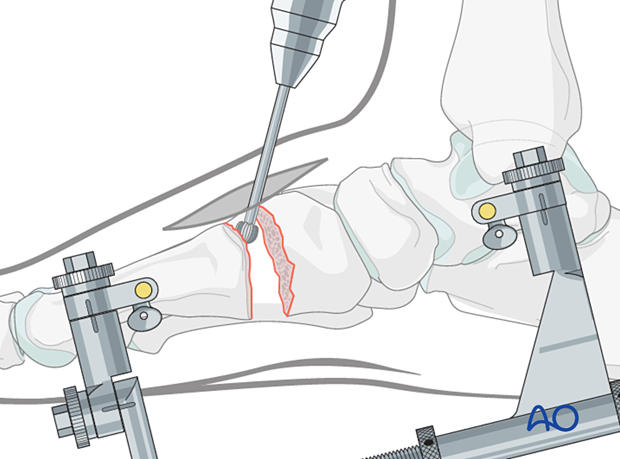
Penetrate the subchondral bone of the opposing bone(s) using a high-speed burr to promote bone growth.
6. Restoration of medial column length
Use the medial-column distractor to restore the length of the medial column.
It is helpful to have comparative x-rays from the uninjured side, allowing proper length and morphology to be judged.
7. Fusion
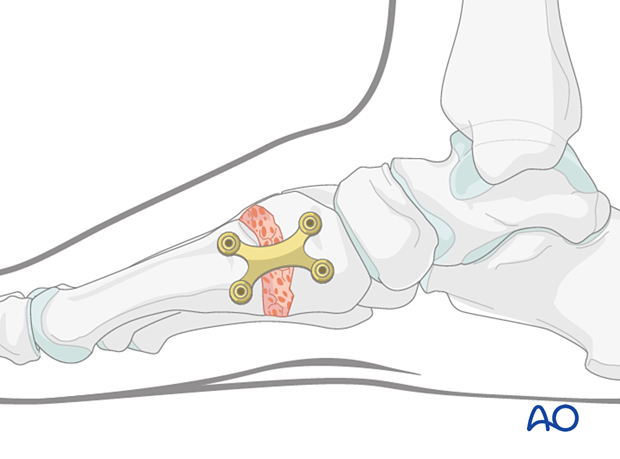
Plate fixation
Apply a plate across the tarsometatarsal joint (or the naviculocuneiform joint) and secure it using screws inserted in neutral mode.
The medial cuneiform is plated medially or dorsomedially.
Any robust plate type can be used for the procedure; precontoured fusion plates may be preferred.
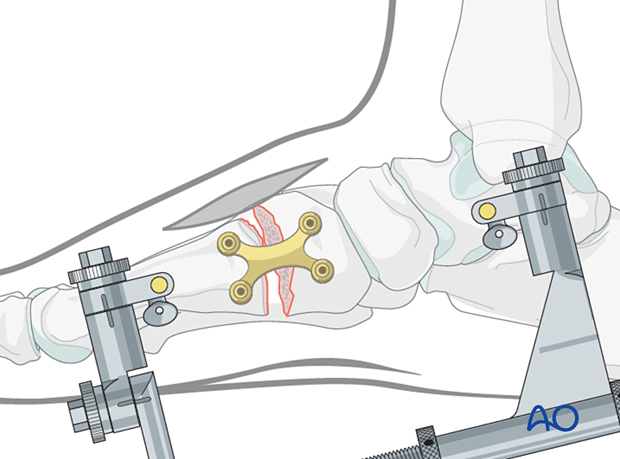
Grafting of bone defect
Bone graft the remaining bone defect using cancellous or corticocancellous bone graft (for structural support) harvested from the distal or proximal tibia.
Remove the distractor.
Before completing the surgery, the medial column length should be assured radiographically.
8. Aftercare
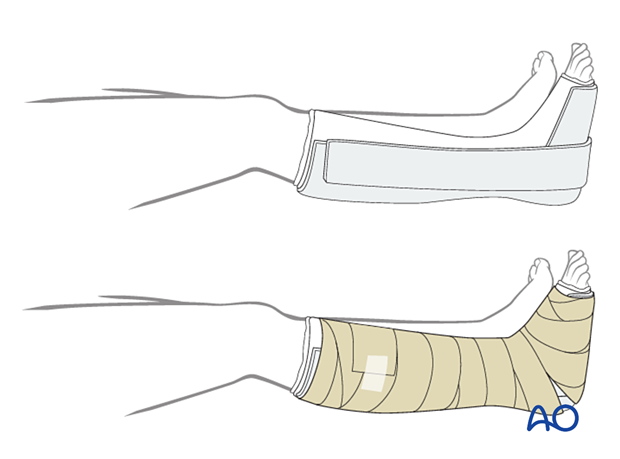
Dressing
The non-adherent antibacterial dressing is applied as a first layer. Sterile undercast padding is placed from toes to knee. Extra side and posterior cushion padding are added.
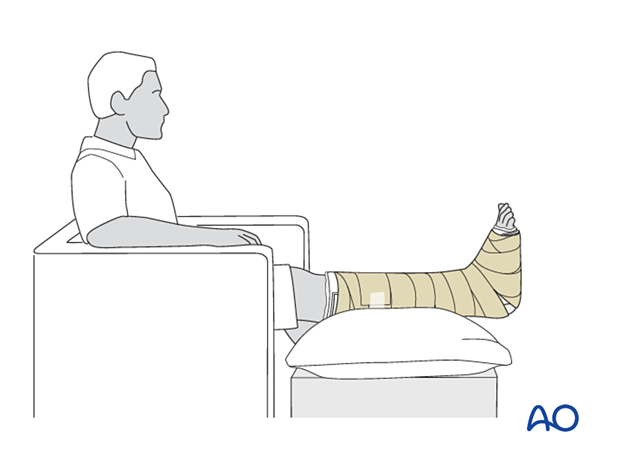
Immobilization
The foot should be immobilized for the first two weeks, which can be achieved using a three-sided plaster splint. The anterior area is left free of plaster to allow for swelling. Ensure that the splint’s medial and lateral vertical portions do not overlap anteriorly and that the splint does not compress the popliteal space or the calf.
Follow-up
The patient should be counseled to keep the leg on a cushion and elevated. Remember not to elevate the leg too much as it may impede the inflow. The foot’s ideal position is halfway between the waist and the heart when the patient is sitting. While seated, the foot should be on a cushion and elevated, but if badly swollen, the patient must be supine since elevating the foot while seated decreases swelling less effectively.
Avoid direct pressure against the heel during recumbency to prevent decubiti.
The OR dressing is usually left in place and not changed until the first postoperative visit at two weeks when x-rays are obtained once the dressing is removed. If any complication is suspected (eg, infection or compartment syndrome), the dressing must be split and, if necessary, removed to allow full inspection.
The strict non-weight bearing should be maintained until there is evidence of healing and any transfixion K-wires (6–12 weeks) or bridging devices (min 12 weeks) are removed.
Daily toe movement is encouraged.
Formal physical therapy should not begin in the early postoperative period.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid and hind-foot.













