Lag screw fixation of tarsometatarsal joint
1. Introduction
Instability of the tarsometatarsal joint due to capsular injuries may occur.
They may occur in isolation or as part of a Lisfranc injury.
A high index of suspicion is warranted when making the diagnosis.
If the surgeon desires to fuse the joint, a lag screw technique is used.
If the surgeon decides to preserve the joint, a positioning screw is used.
2. Approach
The following surgical approaches may be helpful:
3. Removal of joint cartilage (when fusion is desired)
Visualization
The cartilage on both articular surfaces needs to be removed to allow fusion.
Manual distraction or a medial-column distractor can be used to facilitate visualization.
The proximal pin is inserted into the neck of the talus through a stab incision. Image intensification can ensure correct pin placement outside the articular surfaces. The correct insertion point is often located 1–2 cm posterior to the navicular tubercle.
The distal pin is inserted in the first metatarsal.
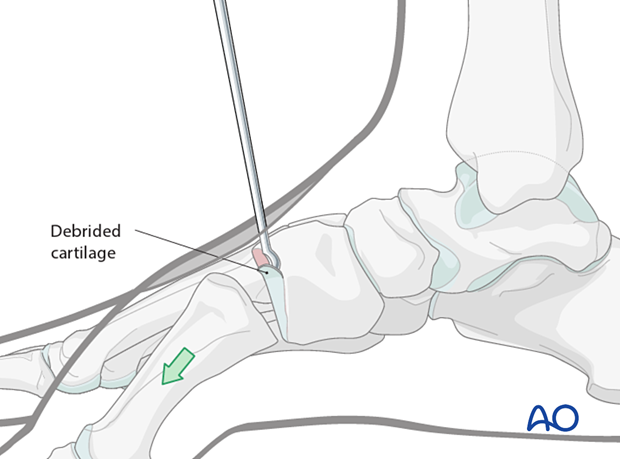
Use a curette or burr to denude the cartilage on both sides of the joint.
Disrupt the subchondral bone using a high-speed burr to promote bone growth.

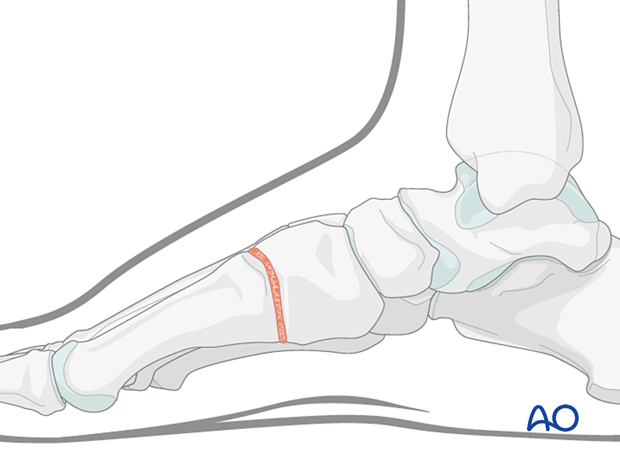
After cartilage removal, the ray length is reestablished using a bone graft before reduction and fixation.
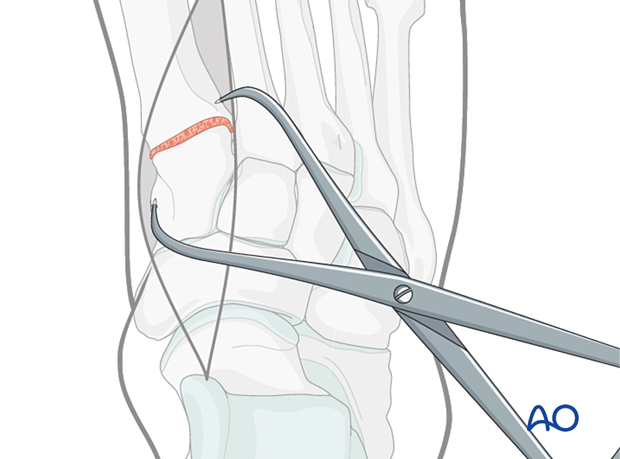
4. Reduction
Reduce the joint using pointed reduction forceps.
Take care to prevent angulation in all planes.
5. Screw insertion
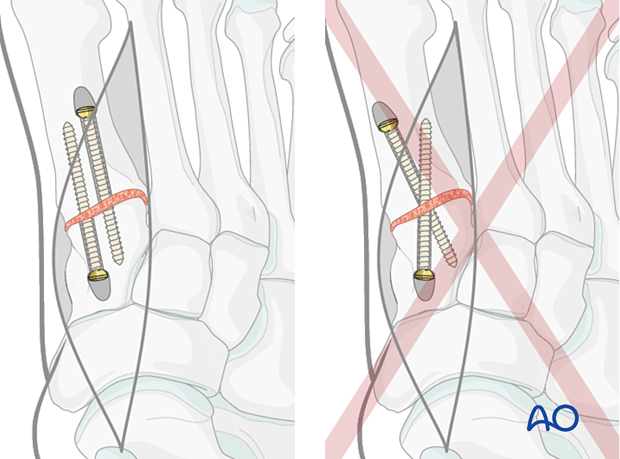
Insert screw(s), 2.7 mm or larger, either from distal to proximal or vice versa.
The first TMT joint typically accepts two screws, while the second and third only accept one screw.
Due to the small size of the bones, screw position and trajectory need to be planned carefully to avoid interference from one another.
The screw holes need to be countersunk to prevent prominent screw heads,
Ideally, the screws should not cross each other at the fusion site.