Arthrodesis of length unstable proximal articular fractures of the 1st–4th metatarsal
1. General considerations
If fragmentation is such that the joint cannot be reconstructed, the options are:
- Nonoperative treatment
- Primary fusion
None of these options are ideal.
The results may be unsatisfactory because of the fracture’s intraarticular nature, and the patient may complain of pain and stiffness.
As fusion is permanent, the decision to perform fusion should be considered for only significantly damaged articular surfaces.
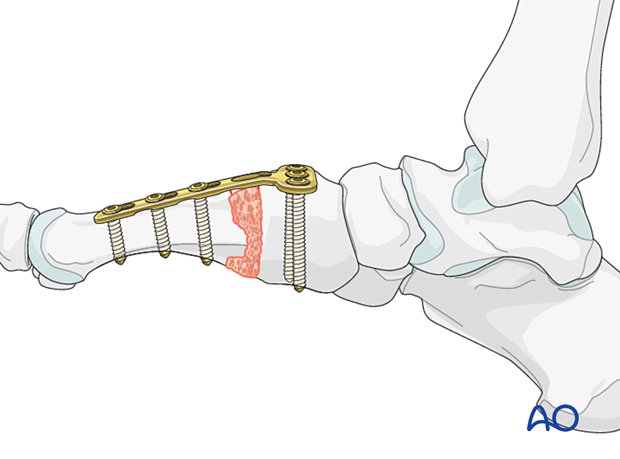
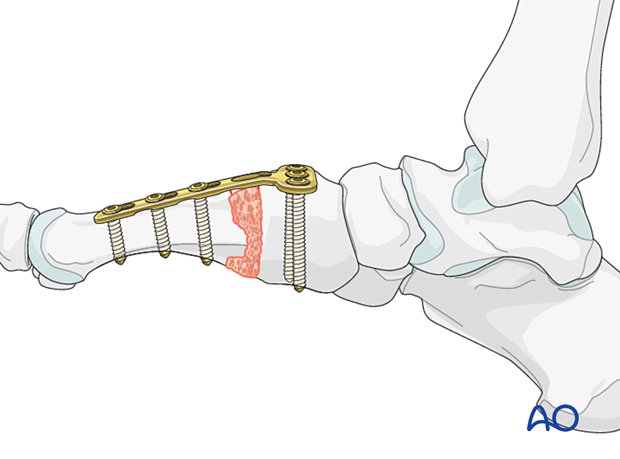
Plates are used in cases with bone loss where maintenance of length is desirable.
A dorsal plate is less prominent than a medially placed plate (first metatarsal).
Associated midfoot instability is common and should be identified if present.
2. Temporizing measures
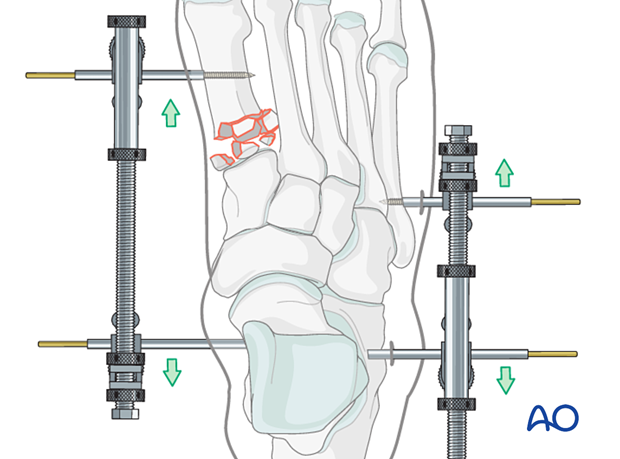
Medial and lateral external fixation (with a distractor device to restore columnar length) may be applied as soon after the injury as possible to stabilize the foot and decrease further injury to the soft tissues.
Percutaneous K-wires can be used to reduce displaced fragments and left as temporary fixation.
3. Approach
Selection of approach
Fractures of the first metatarsal can be approached through a medial or a dorsal approach:
Any single metatarsal injury in metatarsals 2–3 can be approached through the following dorsal approach:
- Dorsal approach to single metatarsals 2–4
- Dorsal approach to multiple metatarsals (when several metatarsals are injured).
Visualization
A medial-column distractor may be used to restore the length of the medial column.
If the medial distraction creates an abduction deformity, applying a lateral distractor may help minimize the angulation.
It is helpful to have comparative x-rays from the uninjured side, allowing proper length and morphology to be judged.
The proximal pin is inserted into the neck of the talus through a stab incision. Image intensification can ensure correct pin placement outside the articular surfaces. The correct insertion point is often located 1–2 cm posterior to the navicular tubercle.
The distal pin is inserted in the first metatarsal.
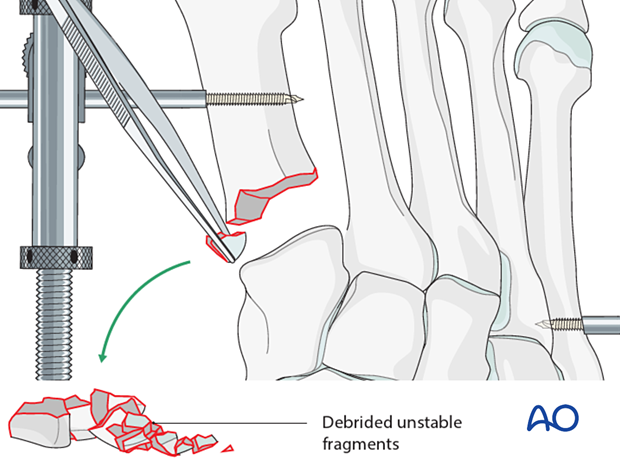
4. Irrigation and debridement
Irrigate the fracture site using a syringe.
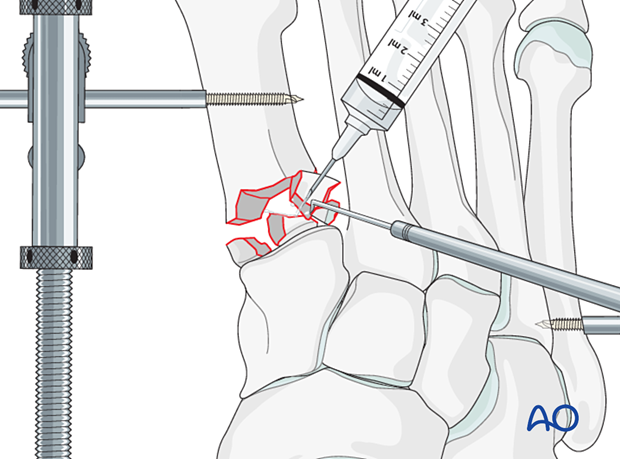
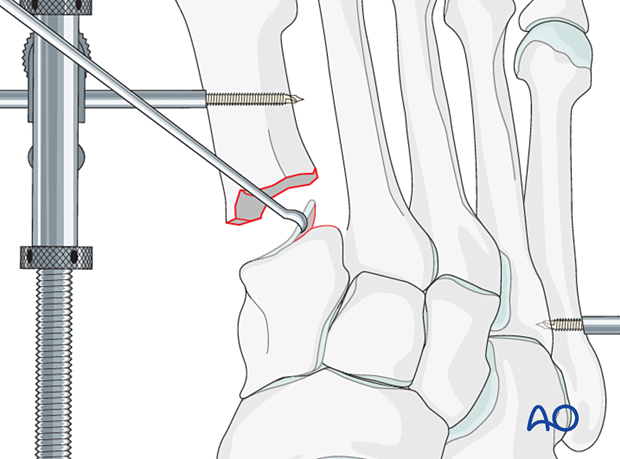
Displaced fracture fragments are debrided and mobilized with a dental pick or Freer elevator. Debrided cancellous fragments should be kept and used as bone grafts at the end of the procedure.
Once adequate visualization has been achieved and the joint thoroughly irrigated, examine the extent of articular surface involvement to validate the preoperative plan of primary fusion versus ORIF.
If joint fragmentation is not extensive and tarsometatarsal instability is absent, it may be possible to perform fixation.
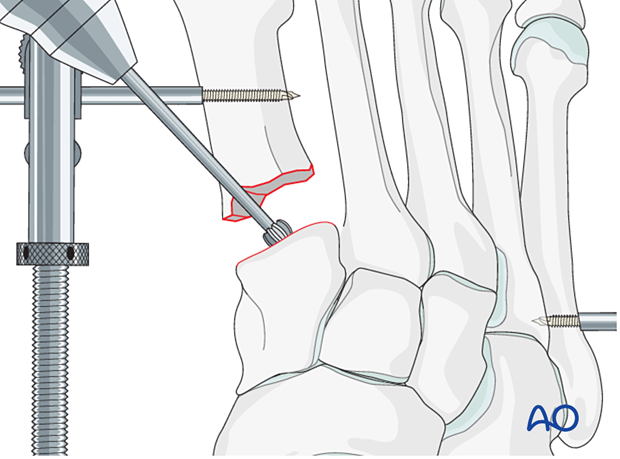
5. Preparation of joint for fusion
Preparation of joint for fusion
Remove the cartilage from the adjacent bone using a curette.
Penetrate the subchondral bone using a high-speed burr to promote bone growth.
6. Fixation of arthrodesis
Plate contouring
Contour a T-plate to fit the bone surface.
For the first TMT joint, a 3.5 mm plate can be used, which allows for three-screw fixation in the distal and proximal segments.
For the second and third TMT joint, a 2.7 mm T-plate can be used, which allows for two screws in the proximal and three screws in the distal segment.
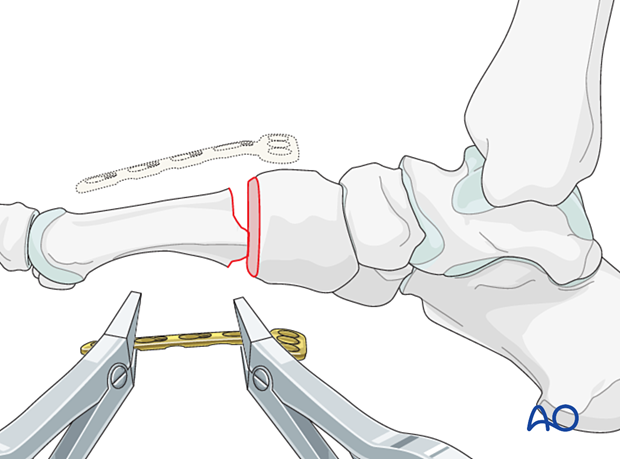
Fixation
Insert screws in neutral mode after appropriate length, alignment, and rotation have been verified.
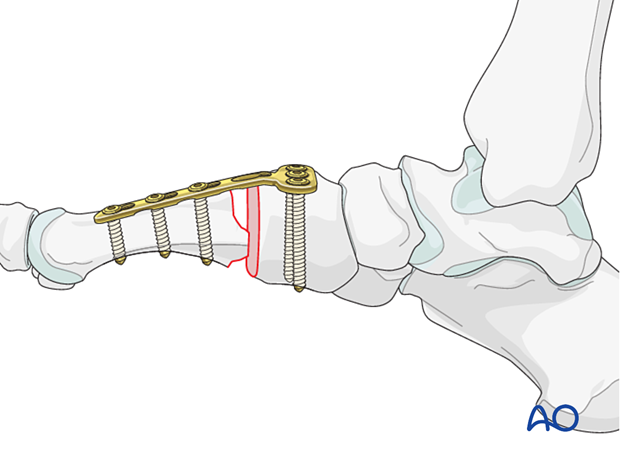
The remaining bone defect should be grafted using cancellous or corticocancellous bone graft for structural support harvested from the distal or proximal tibia.