Treatment of Lisfranc injuries
1. Introduction
Compartment syndrome
Lisfranc injuries may, in more than 25% of the cases, be associated with or cause compartment syndrome. If compartment syndrome is suspected, decompression may need to be performed. For details on compartment syndrome, follow:
The swelling is unlikely to subside until reduction is achieved. Nevertheless, the status of the soft tissue envelope should be considered before intervening surgically.
Preoperative planning
For these complex injuries, a detailed preoperative plan is strongly encouraged. The planning steps may be as follows:
- Determine which joints are unstable
- Determine whether instability is caused by a bony or a ligamentous injury
- Determine how to best reconstruct each injury
- Identify critical points for restoration of length for both medial and lateral columns
- Evaluate the need for and plan for the stabilization of ligamentous injuries, including ligamentous instability between the columns
General strategy for reconstruction
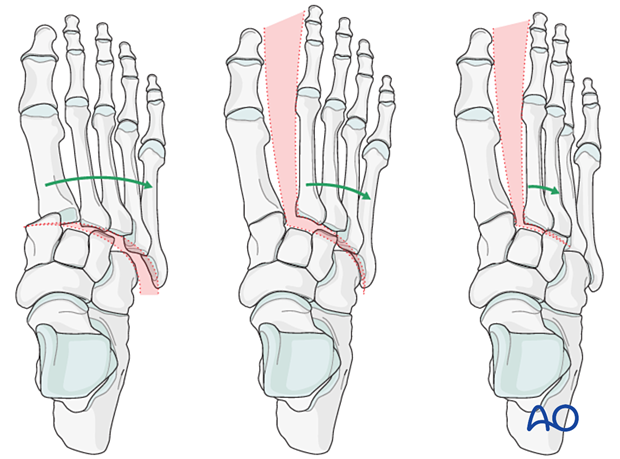
SequenceThe Lisfranc injury can vary widely, and the treatment plan will differ for each case.
One stepwise generic approach to reconstruction of Lisfranc injuries may be:
- Restoration of the relation between the cuneiforms and navicular
- Restore the normal anatomical relationship between the second metatarsal and the middle-cuneiform. This step creates the base for all further reductions.
- Restore the normal anatomical relationship between the second metatarsal and the medial cuneiform.
- Injuries of the tarsometatarsal joints are then addressed in the following sequence: 1st, 3rd, 4th, and then the 5th.
Bony injuries of the 1st-3rd tarsometatarsal joints are reconstructed if possible or otherwise fused.
There is no clear guideline on whether unstable joints without bony injury should be fused or temporarily stabilized until the ligaments have healed. The decision will depend on the surgeon's preference and the overall injury. In general, 1st-3rd tarsometatarsal joints can be fused without significantly impacting foot function.
The 4th-5th tarsometatarsal joints should be left functional or "mobile" and are most often stabilized with temporary K-wires if possible.
Some surgeons prefer first temporarily to stabilize all injuries with K-wires. The stability and function of the foot can then be verified before securing the reconstruction with plates and screws.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Intraoperative determination of joint instability
Stress radiographs under image intensification may be performed to supplement the preoperative workup.
As an alternative to applying valgus stress, preoperative weight-bearing radiographs may be used (if tolerated by the patient).
These images will assist in the determination of ligamentous instability between the cuneiforms and the metatarsals.
AP view with valgus stress
By applying valgus stress, the following can be observed:
- Lateral displacement of 2nd metatarsal on middle cuneiform
- TMT 1 disruption
- A gap between the medial cuneiform and second metatarsal (Lisfranc ligamentous injury)
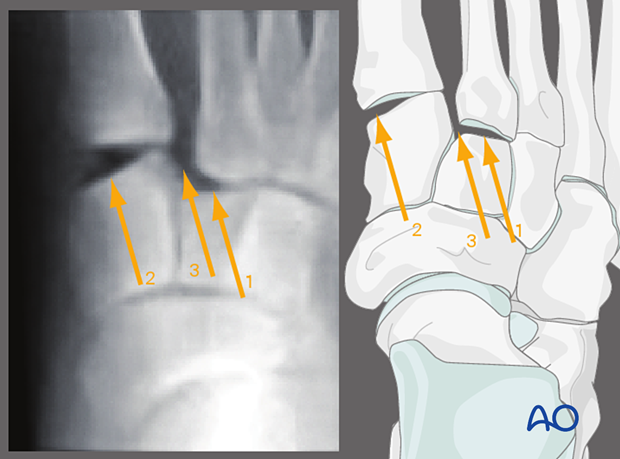
- Lateral displacement of all metatarsals
- Lateral displacement of the middle and lateral column
- Lateral displacement of the middle column
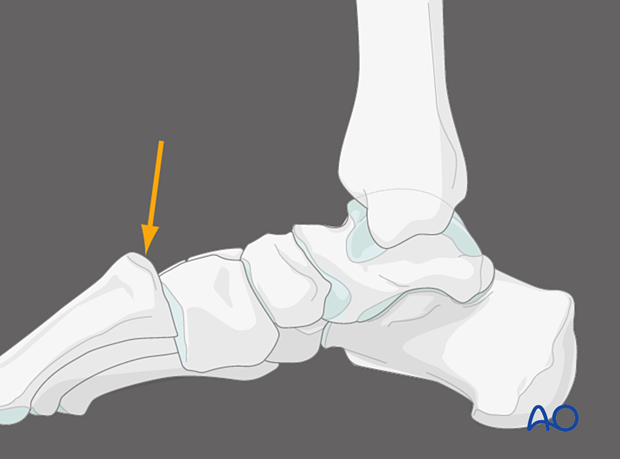
Medial view with plantar pressure over the first tarsometatarsal joint
By applying pressure over the plantar aspect over the first tarsal metatarsal joint, dorsal capsular instability of the first tarsal metatarsal joint can be identified.
The dorsal cortex of the metatarsals should be colinear with the dorsal cortex of the cuneiforms. Dorsal displacement of the metatarsal bases above the cuneiforms level is abnormal and indicates instability of the first tarsometatarsal joint.
3. Reduction
Closed reduction
Under anesthesia, apply manual traction in the axial vector and reverse the mechanism of the injury.
Open reduction
If closed reduction maneuvers are unsuccessful in obtaining an anatomic redction of the joint(s), the failure can be due to bone interference, soft tissue interposition, or both.
A direct open reduction will be necessary.
4. Preparation and approaches
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

Surgical approaches
The fracture configuration will determine the selection of surgical approaches. The following approaches may be useful.
- Dorsolateral approach
- Dorsomedial approach
- Medial utility incision
- Percutaneous approach to the navicular
- Safe zones for pin and K-wire insertion
All Lisfranc injuries will involve the second tarsometatarsal joint. By extending a medial incision slightly, this approach can be used for stabilization of the first and third tarsometatarsal joints.
Additional stab incisions may be needed for lag screw and/or fiber tape insertion (eg, a lag screw from medial to mid cuneiform)
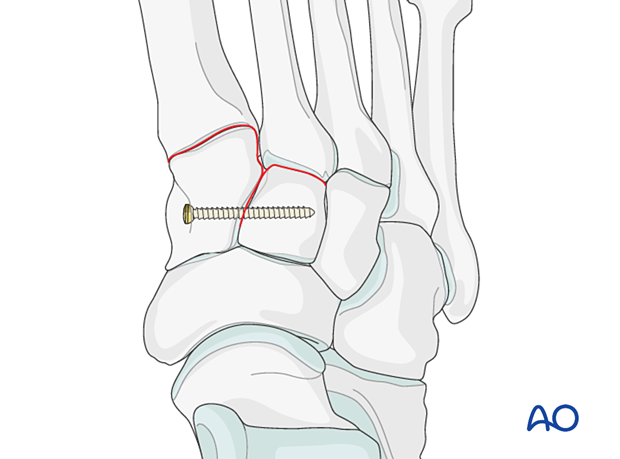
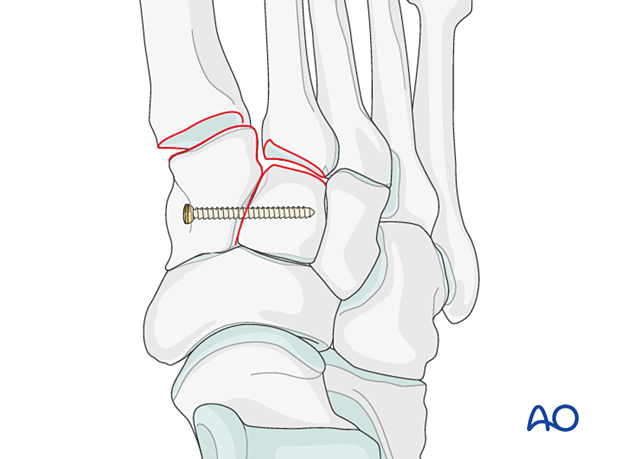
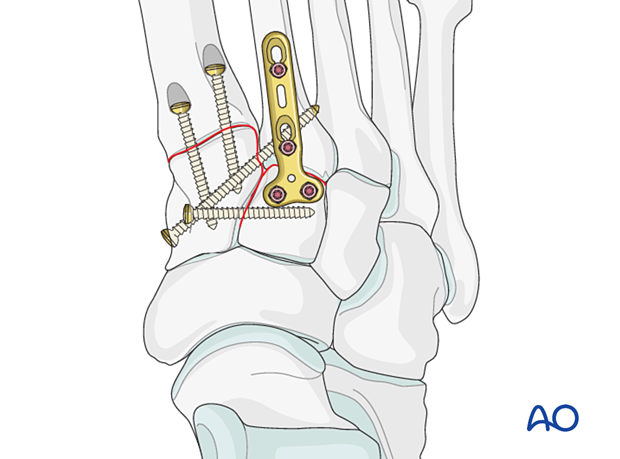
5. Step 1: Instability between medial and mid cuneiform
If the injury also involves instability between the medial and mid cuneiform, this may be addressed by either provisional or definitive fixation and/or fusion:
- Position screw inserted from the medial cuneiform to the middle cuneiform (illustrated)
- Flexible, dynamic fixation
- Fusion of intercuneiform joint with a lag screw (the lag screw should not enter the joint between the medial and lateral cuneiform)
6. Step 2: Instability 2nd tarsal metatarsal joint (if present)
The anatomical relationship between the second metatarsal and the middle cuneiform is restored. As this will be the reference point for reducing all other tarsometatarsal joints, correct alignment in this step is essential.
Ligamentous instability
ReductionInsert a K-wire intramedullary from distal to proximal and use it as a joystick to achieve axial alignment.
Verify the axial alignment in the AP view and the dorsoplantar alignment in the lateral view using image intensification.
The K-wire is advanced across the joint into the middle cuneiform to secure the correct alignment.
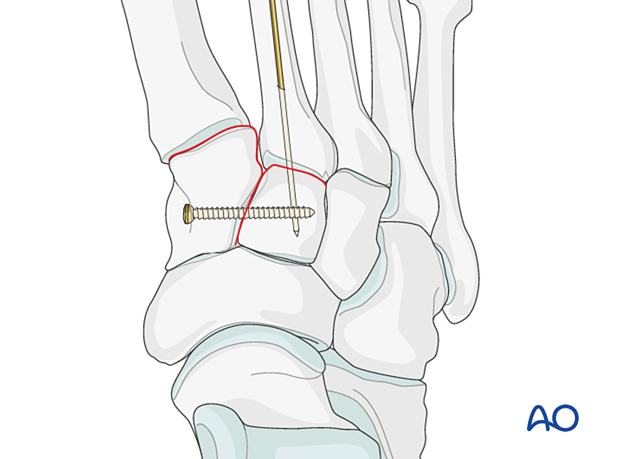
Apply a position screw across the joint to hold the reduction.
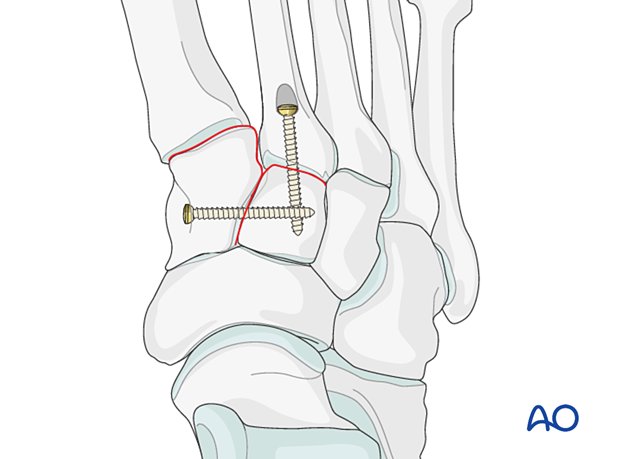
A small T-plate is a reasonable option if there sufficient bone stock for its application.

If arthrodesis is desired, then a transarticular lag screw is inserted. To maintain the anatomic relationship of the midfoot, a bone graft should be used after joint preparation.
Althoug fixation or fusion can be performed using a lag screw, this may interfere with other planned hardware (stabilization of the Lisfranc ligament) or be contraindicated due to comminution of the proximal second metatarsal. In this case, a Lisfranc plate (or a contoured 2.7 locking plate) may also be used.
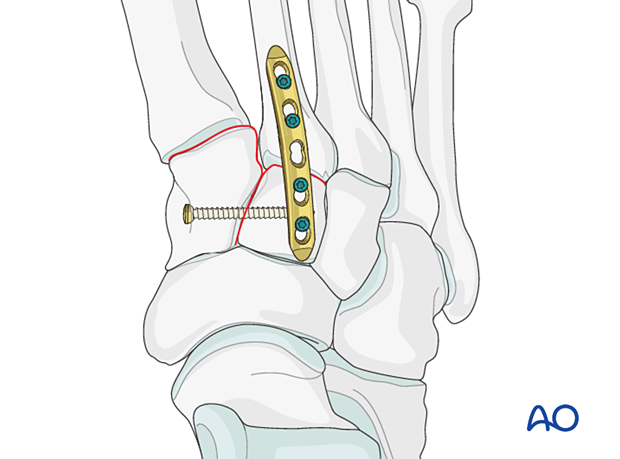
Instability caused by fractures of the proximal 2nd metatarsal
Fractures of the proximal 2nd metatarsal are addressed using one of the following techniques:
- Lag screw (partial articular fracture)
- Plate with or without lag screw (reconstructible complete articular fracture where the articular component is amenable to lag screw fixation)
- Locking plate with or without lag screw (reconstructible complete articular fracture in osteoporotic bone or in cases where a lag screw cannot be inserted)
- Primary arthrodesis of length stable and primary arthrodesis of length unstable fractures (non-reconstructible articular fracture)
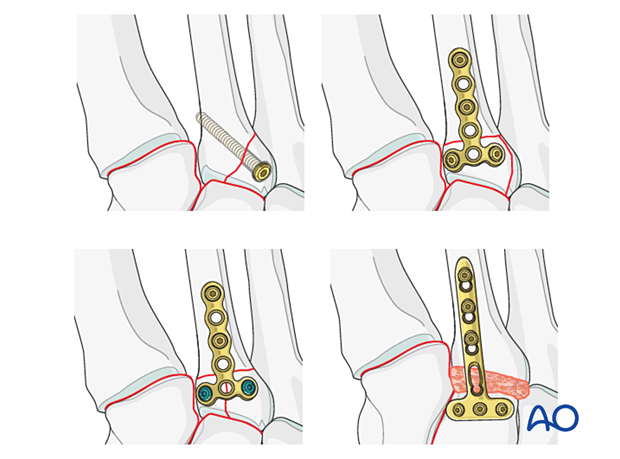
If the reduction and fixation of the tarsometatarsal joint do not provide stability to the joint, a bridge plate can be temporarily applied until union has occurred.
Alternatively, transarticular lag screws can be applied to achieve primary arthrodesis (fusion).
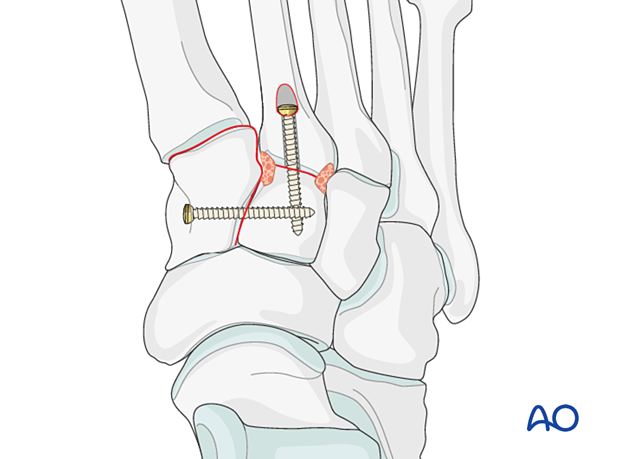
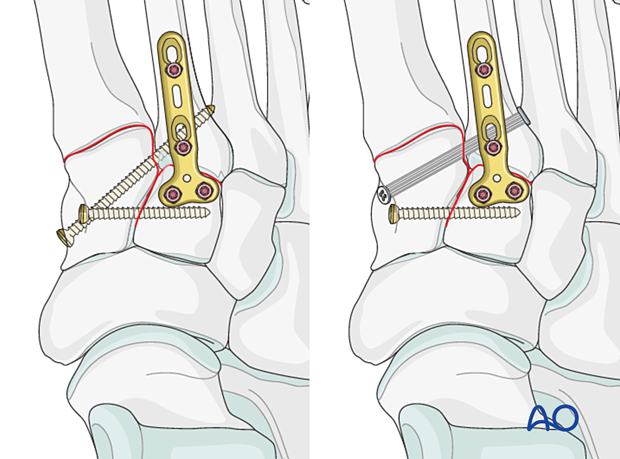
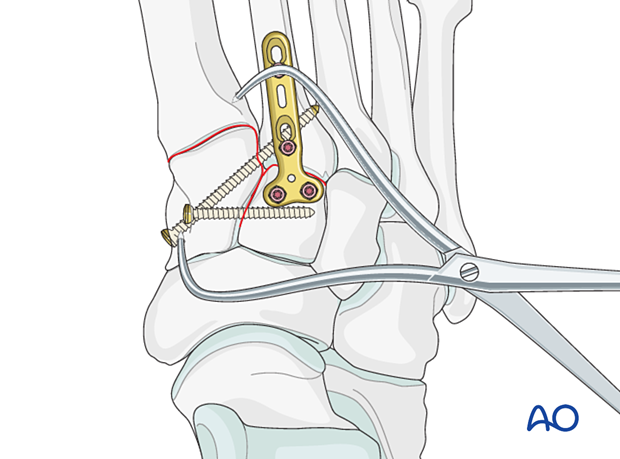
7. Step 3: Lisfranc ligament rupture
The goal is to reduce and compress the second metatarsal base to the medial cuneiform and provide stabilization.
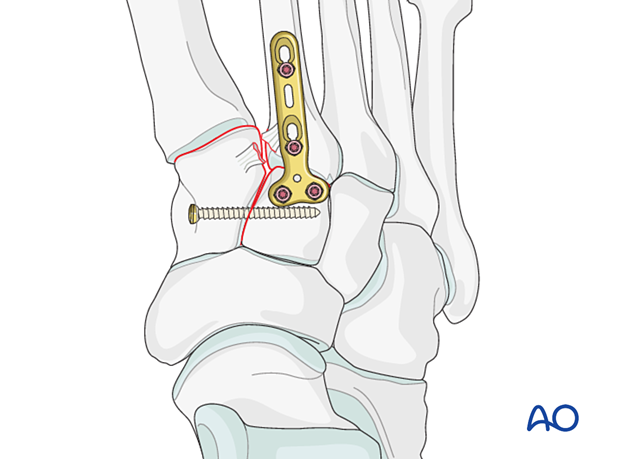
Lisfranc instability
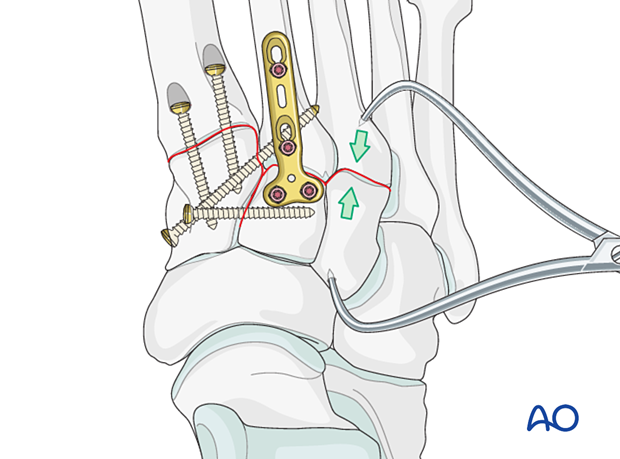
ReductionTo facilitate the application of the reduction forceps, a K-wire may be used to create a recess laterally at the base of the second metatarsal and medially on the medial cuneiform.
Use pointed reduction forceps to reduce the second metatarsal base to the medial cuneiform. Be mindful to place the reduction forceps away from the placement of the planned position screw.
The reduction forceps can be used percutaneously and should be applied to provide compression in the vector of the Lisfranc ligament.
Verify the reduction visually and radiographically.
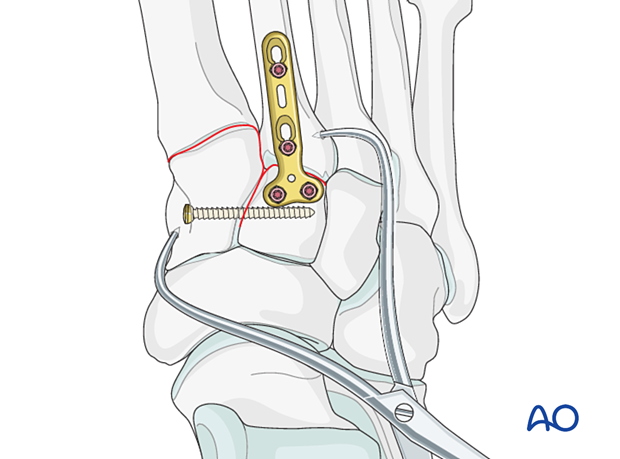
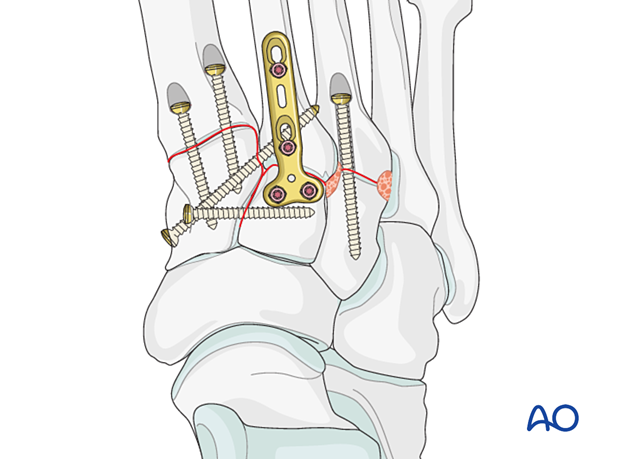
Fixation may be performed using either:
- Position screw inserted from the second metatarsal base to the medial cuneiform or vice versa.
- Flexible dynamic fixation
If the base of the second metatarsal is comminuted, the fixation can be performed by inserting a positioning screw between the first and second metatarsal instead.
8. Step 4: Instability 1st tarsal metatarsal joint (if present)
Ligamentous instability
ReductionIn purely ligamentous injuries, reduce the joint using a pointed reduction clamp.
Stabilization is achieved by inserting a position screw. Two screws may be used for added stability.
The screw holes need to be countersunk to prevent protruding screw heads.
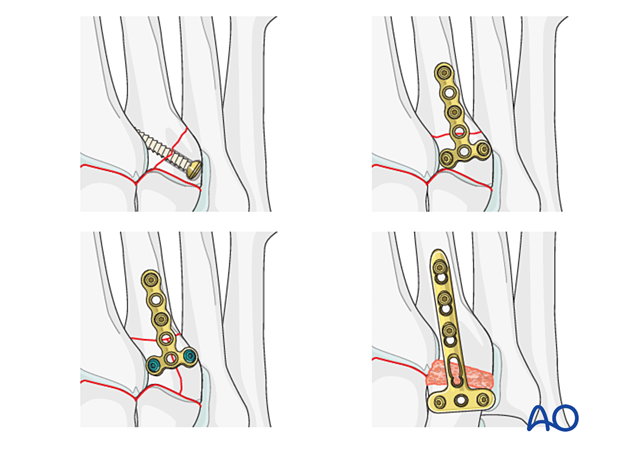
Instability caused by fractures of the proximal 1st metatarsal
Fractures of the proximal metatarsal are addressed using one of the following techniques:
- Lag screw (partial articular fracture)
- Plate with or without lag screw (reconstructible complete articular fracture where the articular component is amenable to lag screw fixation)
- Locking plate with or without lag screw (reconstructible complete articular fracture in osteoporotic bone or in cases where a lag screw cannot be inserted)
- Primary arthrodesis of length stable and primary arthrodesis of length unstable fractures (non-reconstructible articular fracture)
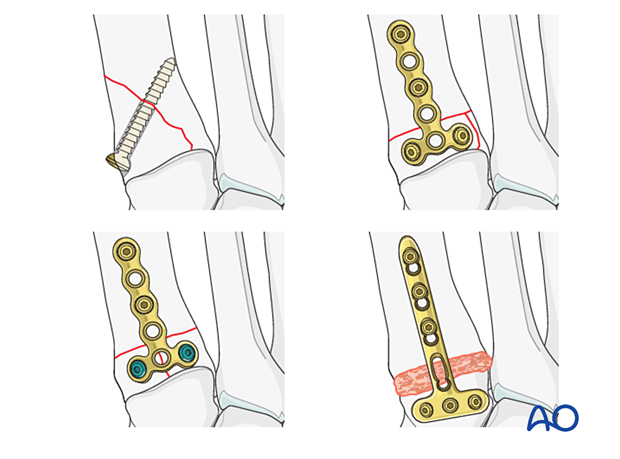
If the reduction and fixation of the tarsometatarsal joint do not provide stability to the joint, a bridge plate can be temporarily applied until union has occurred.
Alternatively, transarticular screws can be applied to achieve primary arthrodesis (fusion).
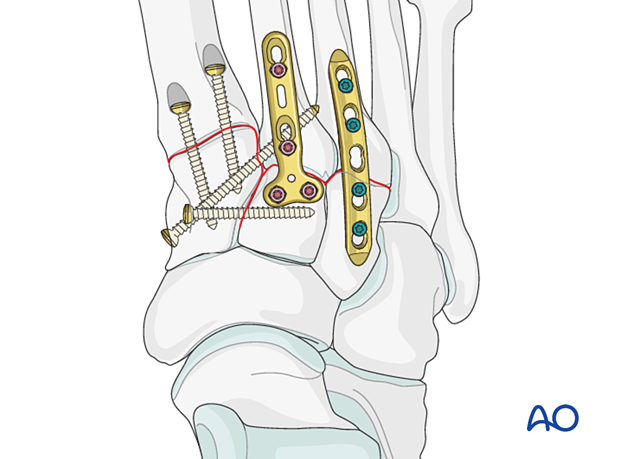
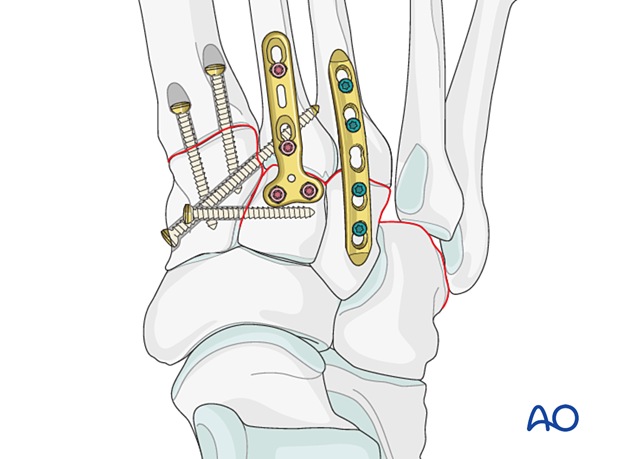
9. Step 5: Instability of 3rd tarsal metatarsal joint (if present)
Ligamentous instability
ReductionReduce the joint using a pointed reduction forceps.
Fixation and/or primary arthrodesis (fusion) may be achieved by inserting at least one intramedullary screw from distal to proximal.
Alternatively, a contoured 2.7 plate may be used in bridging mode to temporarily stabilize the joint until healing has occurred.
In this case, the plate is contoured to fit the bone surface and fixed using locking head screws or screws inserted in neutral mode.
Instability caused by fractures of the proximal 3rd metatarsal
Fractures of the proximal metatarsal are addressed using one of the following techniques:
- Lag screw (partial articular fracture)
- Plate with or without lag screw (reconstructible complete articular fracture where the articular component is amenable to lag screw fixation)
- Locking plate with or without lag screw (reconstructible complete articular fracture in osteoporotic bone or in cases where a lag screw cannot be inserted)
- Primary arthrodesis of length stable and primary arthrodesis of length unstable fractures (non-reconstructible articular fracture)
If the reduction and fixation of the tarsometatarsal joint do not provide stability to the joint, a bridge plate can be temporarily applied until union has occurred.
Alternatively, transarticular screws can be applied to achieve primary arthrodesis (fusion).
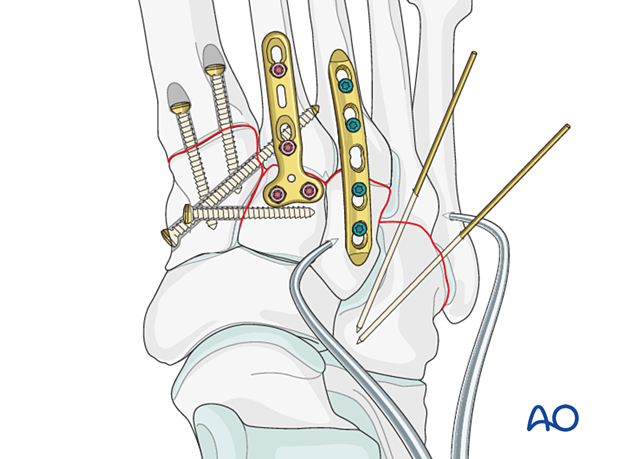
10. Step 6: Instability 4th and 5th tarsal metatarsal joints (if present)
If there are any lateral column fractures, address these individually as outlined in the metatarsal section before securing the 4th and 5th metatarsals to the cuboid using K-wires.
Ligament instability or residual instability after medial column fixation will be addressed as outlined below.
Reduction
If the 4th and 5th metatarsals are displaced laterally, they need to be reduced to achieve the anatomical relation to the cuboid using a pointed reduction forceps.
Visual and fluoroscopic guidance is necessary to confirm anatomic reduction.
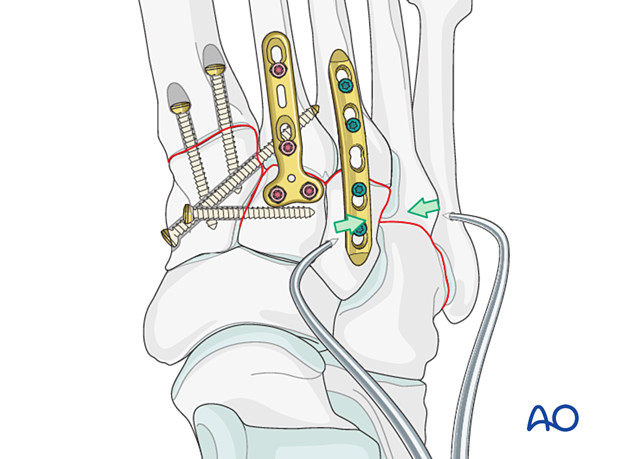
Fixation
The reduction is secured by inserting K-wires from the 4th and 5th metatarsal base to the cuboid.
These K-wires are removed once healing is completed.
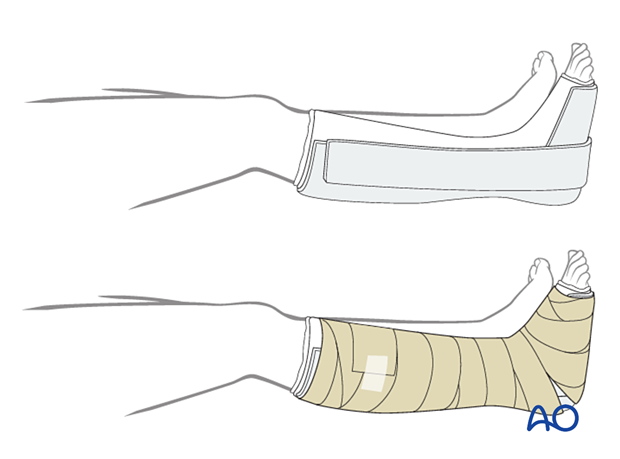
11. Aftercare
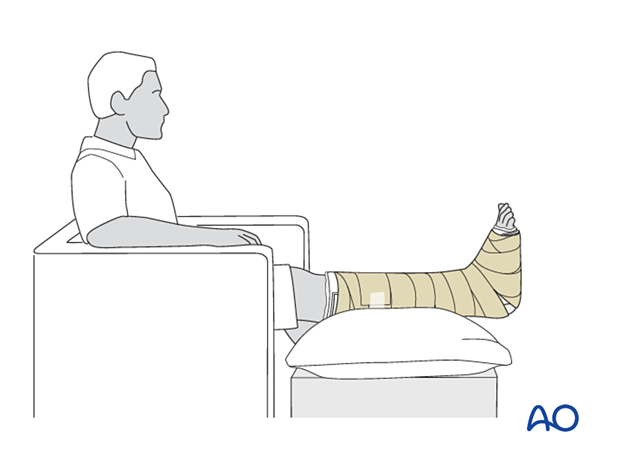
Dressing
The non-adherent antibacterial dressing is applied as a first layer. Sterile undercast padding is placed from toes to knee. Extra side and posterior cushion padding are added.
Immobilization
The foot should be immobilized for the first two weeks, which can be achieved using a three-sided plaster splint. The anterior area is left free of plaster to allow for swelling. Ensure that the medial and lateral vertical portions of the splint do not overlap anteriorly and that the splint does not compress the popliteal space or the calf.
Early weight-bearing and a walking boot may be permitted in the instance of pure ligamentous injury treated with a dynamic fixation device.
Follow-up
The patient should be counseled to keep the leg on a cushion and elevated. Remember not to elevate the leg too much as it may impede the inflow. When the patient is sitting, the foot's ideal position is halfway between the waist and the heart. While seated, the foot should be on a cushion and elevated, but if badly swollen, the patient must be supine since elevating the foot while seated is not as effective in decreasing the swelling.
Avoid direct pressure against the heel during recumbency to prevent decubiti.
The OR dressing is usually left in place and not changed until the first postoperative visit at two weeks when x-rays are obtained once the dressing is removed. If any complication is suspected (eg, infection or compartment syndrome), the dressing must be split and, if necessary, removed to allow full inspection.
The strict non-weight bearing should be maintained until there is evidence of healing and any transfixion K-wires (6-12 weeks) or bridging devices (min 12 weeks) are removed.
Daily toe movement is encouraged.
Formal physical therapy should not begin in the early postoperative period.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid and hind-foot.
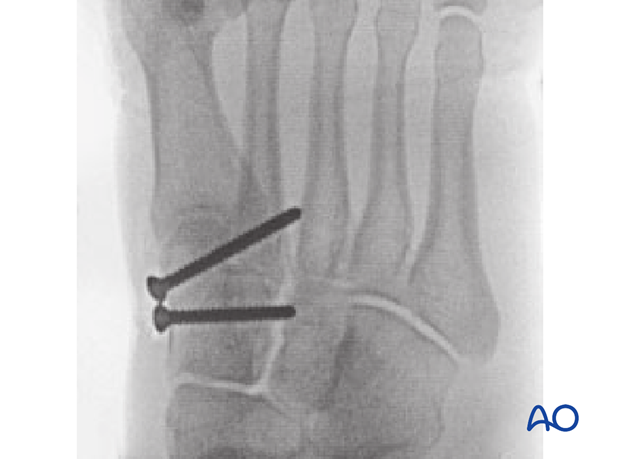
12. Case example 1
This is the preoperative image of a simple ligamentous Lisfranc injury.

This is the lateral view of the above injury.
The lateral image is often less helpful for diagnosis.

Postoperative AP image showing screw reduction between the cuneiforms and the between the medial cuneiform and the base of the second metarsal.

Postoperative oblique view
13. Case example 2
This is the preoperative AP view of a significant Lisfranc injury showing 2nd through 5th metatarsals injuries.
The first ray is less involved than the lateral rays.

Lateral view of the above injury

Postoperative AP and oblique view showing spanning fixation of the Lisfranc joint, which spans the second and fourth rays. The remaining fractures are simply held out to a reduced position by the fixation.
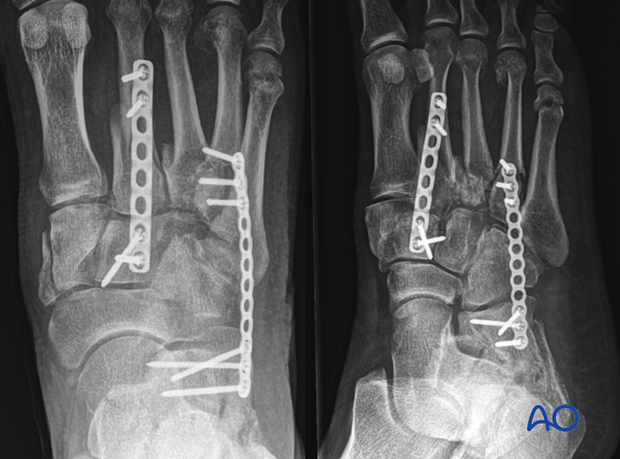
Lateral view of the above fixation

14. Case example 3
This preoperative AP image demonstrates a Lisfranc injury of the 1st, 2nd, and 3rd ray.

Lateral view of the above injury

Three months postoperative image.
Due to the cartilaginous injury, the first and second rays were fused.
Due to the comminuted base of the second metatarsal:
- a screw could not be inserted between the medial cuneiform and the second metatarsal base. Instead, a screw was inserted between the base of the first and the second metatarsal
- The second metatarsal was plated
The fibular plate was already in place due to a previous injury.

Lateral view of the above injury

15. Case example 4
This injury is somewhat unique because it involves disruption between the cuneiforms and between the metatarsals.

Preoperative lateral view

3 Months postoperative AP view. The fixation in this instance needed to go between both cuneiforms and both metatarsals because of the ligamentous disruption in this Lisfranc complex.
In this instance, these four bones were fused, and the screws used in this fashion helped create the most stability for definitive care.

Lateral view of the fixation














