Lag screw fixation
1. General considerations
Anatomical considerations
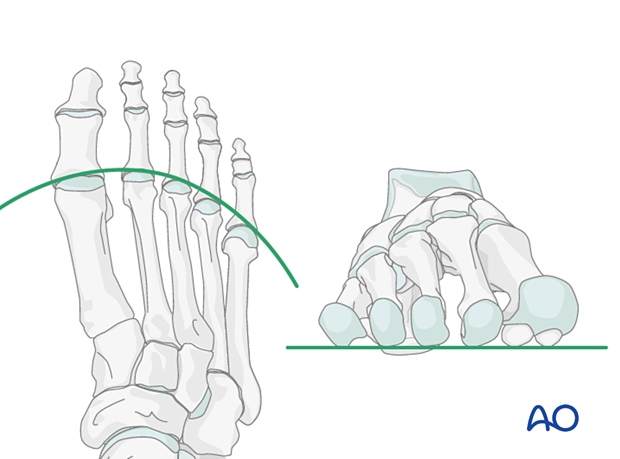
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Strategy options for complete articular fractures
Two options are available:
- Reduce and fix the articular segment to create an A-type pattern. The extraarticular fracture is then reduced to the main fragment and fixed in a second step.
- Reduce all fragments with temporary fixation, followed by definitive screw fixation. Typically, the screw fixation would start with the fixation of the articular block.
Displaced fractures
Displaced fractures may be associated with first tarsometatarsal instability. Reduction of the articular surface and alignment of the first tarsometatarsal joint and its associated soft tissues are essential in treating this injury.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Surgical approach
Fractures of the first metatarsal can be approached through a medial or a dorsal approach:
Any single metatarsal injury in metatarsals 2–4 can be approached through the following dorsal approach:
- Dorsal approach to single metatarsals 2–4
- Dorsal approach to multiple metatarsals (when several metatarsals are injured).
4. Reduction
Visualization
Expose the articular surfaces.
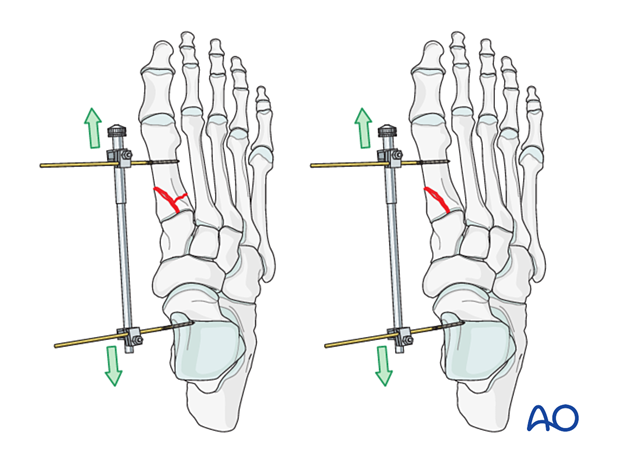
Visualization may be improved by longitudinal manual distraction.
For fractures involving the first metatarsal, a mini distractor may be helpful. Visualization may be improved by releasing the dorsal insertion of the extensor hallucis brevis or extensor digitorum brevis (EHB or EDB).
The extensor hallucis longus should be preserved.
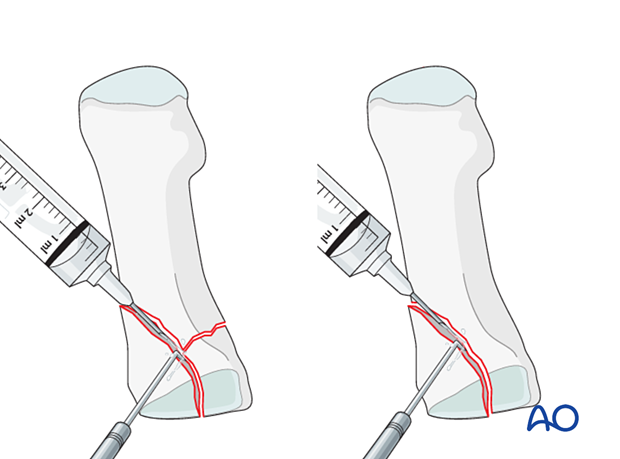
Irrigation
Clean the fracture using a dental pick. Direct suction or irrigation is helpful.
The fracture edges are exposed, and the fragment mobility is assessed. Take great care to avoid comminution of any fragment. It is essential to maintain the vascularity of small fragments.
The extent of articular involvement is assessed, including separate osteochondral fragments.
Reduction
Anatomical reduction of the joint surface is essential to prevent chronic instability or posttraumatic degenerative joint disease.
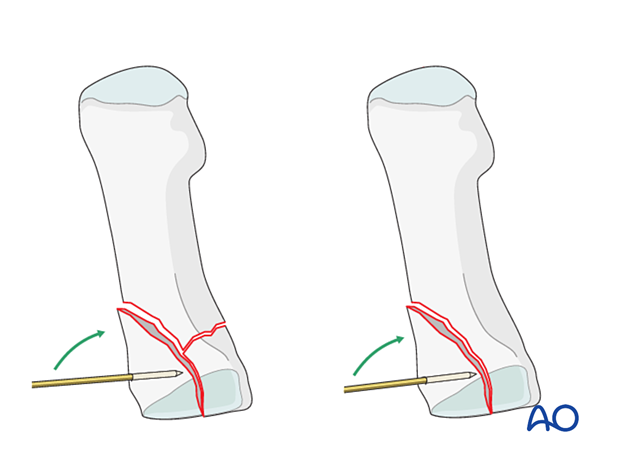
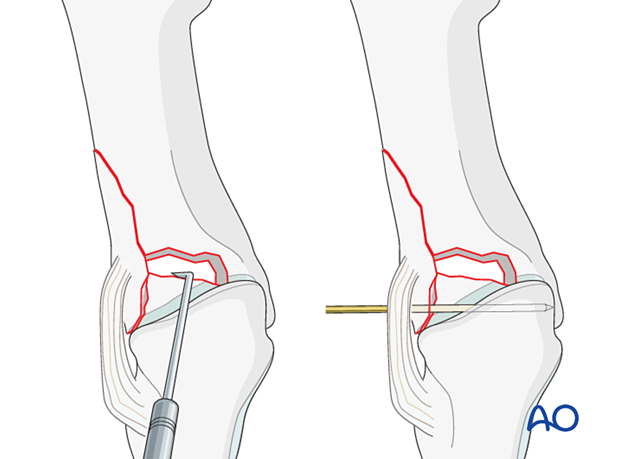
The articular fragments are manipulated using a dental pick, small K-wires as joysticks, or a small periosteal elevator.
If reconstruction of the articular surface is not feasible, a fusion of the joint should be considered.
Small K-wires can be inserted across the fracture line for preliminary fixation.
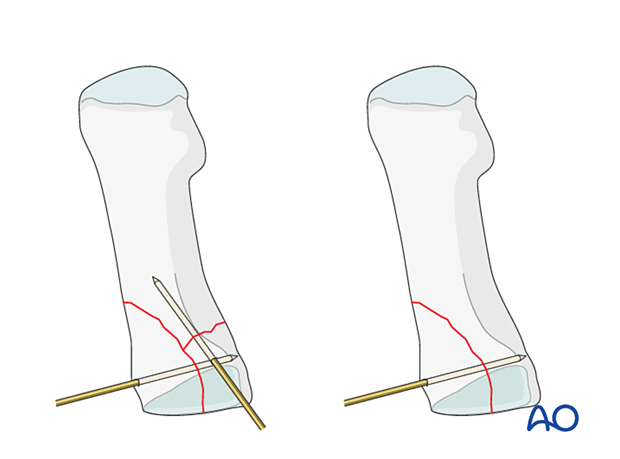
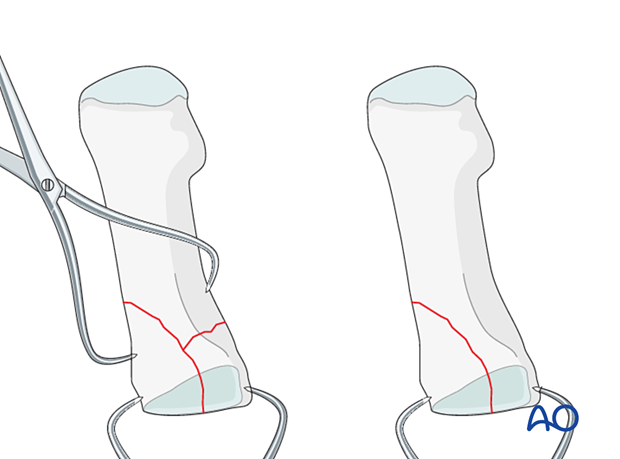
Depending on fracture configuration, pointed reduction forceps may also be used for reduction and preliminary fixation.
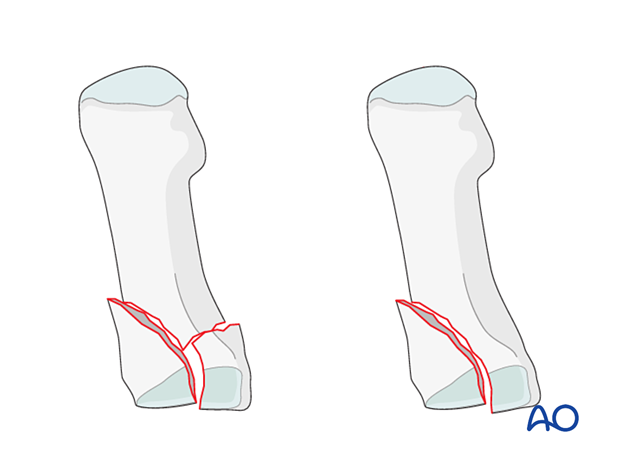
Reduction of impacted fractures
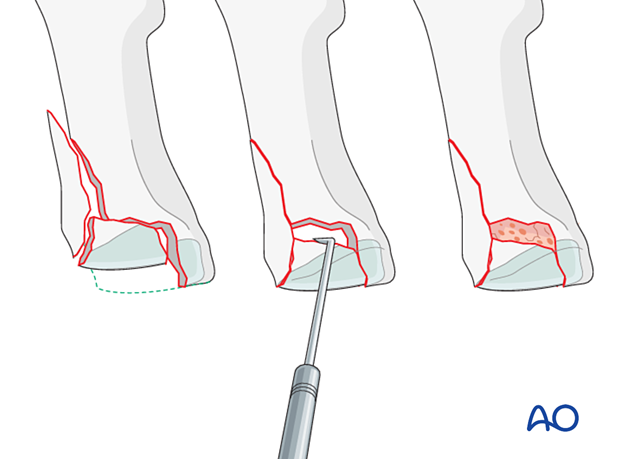
PrincipleCentrally impacted fragments in compression fractures are devoid of soft-tissue attachments and are therefore not reducible by ligamentotaxis.
Direct reduction is necessary.
The key to fixing compression fractures is restoring the joint surface to as close as normal as possible and supporting the reduction with bone graft and internal fixation.
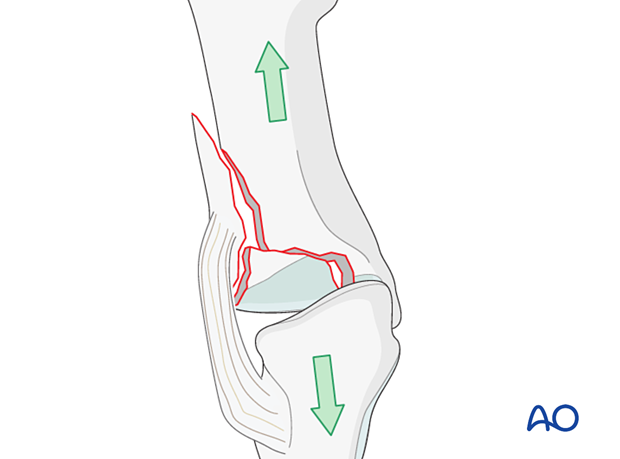
Using a K-wire, or dental pick, the fragments are disimpacted and pushed towards the opposing bone, which is used as a template to ensure congruity of the articular surface.
Since the metaphyseal cancellous bone is impacted, a void may be created by its disimpaction.
This void jeopardizes the fracture in two ways:
- It is a very unstable situation in which the articular fragments may easily displace (collapse)
- The healing process is delayed
The bony defect under the fragments is filled with cancellous bone graft. The bone graft also helps keep the fragments in place when the screw fixation is performed.
Visual inspection of the reduction
Anatomical reduction of the joint surface must be checked under direct visualization and image intensification.
Length, alignment, and rotation of all metatarsals and joints must be maintained.
5. Fixation
Fixation of the articular block
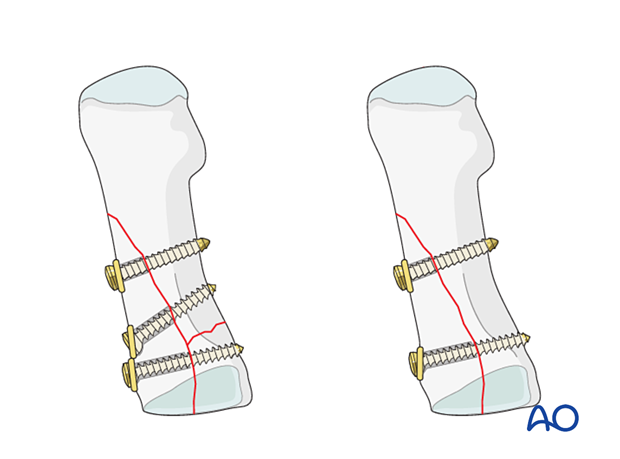
Lag screw fixation of the articular surface should be performed first.
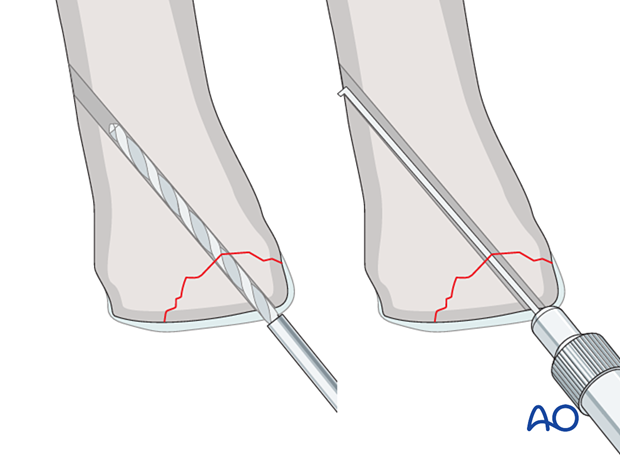
Insert a 2.0 mm or 2.4 mm lag screw perpendicular to the fracture plane.
The lag screws should be placed outside of the articular surface.
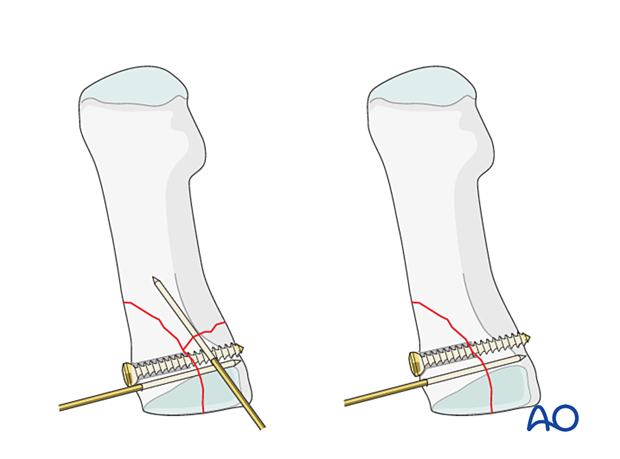
Fixation of the articular block to the shaft
If possible, fix the articular block to the shaft using lag screw.
The extraarticular fracture can be addressed with either a plate or K-wires if lag screw fixation is impossible (see fixation of simple extraarticular fractures).

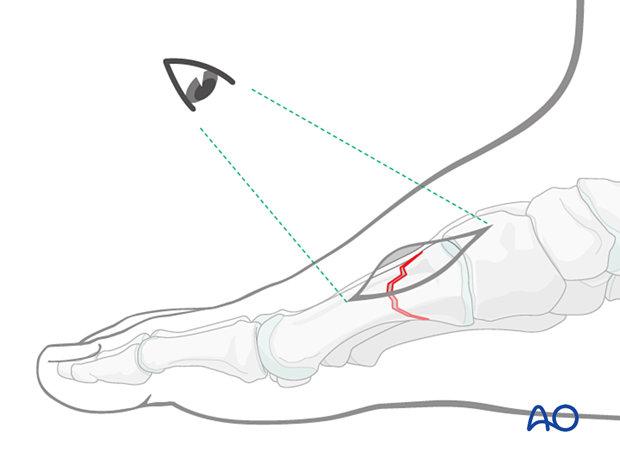
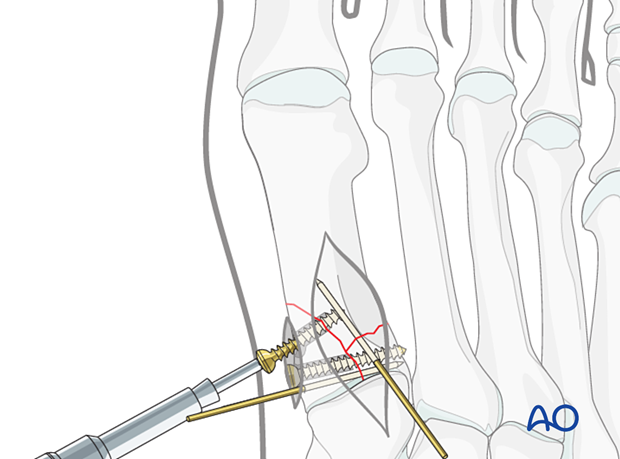
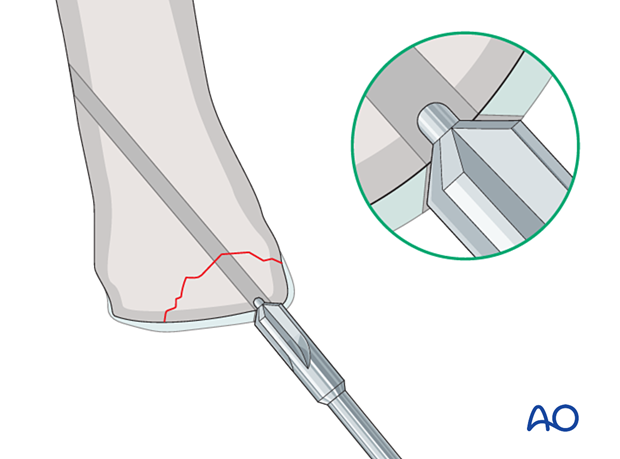
Percutaneous screw insertion
For fractures of the first metatarsal, the lag screws may be inserted percutaneously.
Fixation in osteoporotic bone
If one is dealing with osteoporotic bone, then a washer under the head of the screw is helpful to prevent the head from sinking.
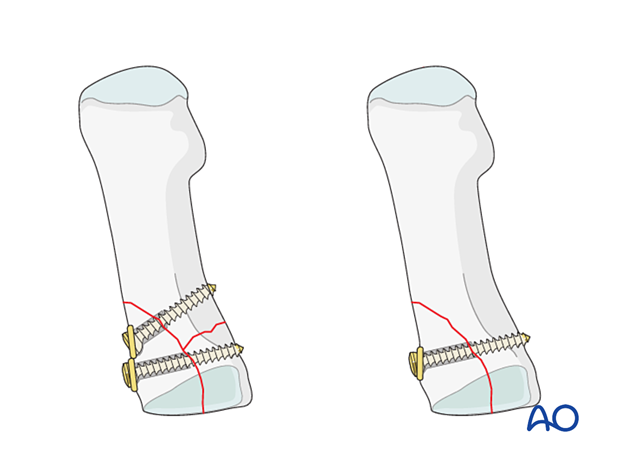
Insertion of additional lag screws for long oblique fractures
A second or third lag screw may be inserted for long oblique fractures. If one is dealing with osteoporotic bone, then a washer under the head of the screw is helpful to prevent the head from sinking.
6. Fixation of osteochondral fragments
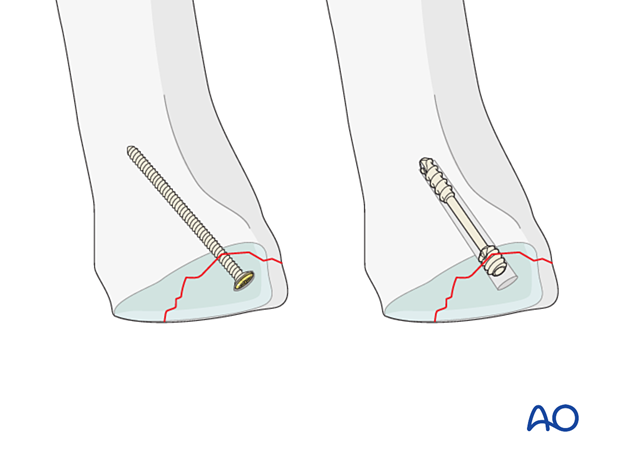
Small fragments are best stabilized with screws inserted through the articular cartilage.
Choose the smallest possible screw diameter to minimize the damage to the joint surface.
If headless screws are available in very small sizes, they have the advantage that they can be inserted deeper into the fragment without protruding.
The opposite cortex may be engaged depending on the fracture configuration and available screw lengths.
Drilling and measuring
Drill carefully not to displace the fragments.
Measure the correct screw length with a depth gauge. When measuring, be careful not to displace the reduced fragments.
Countersinking the articular cartilage
When standard (headed) screws are used, the cartilage is countersunk to facilitate the burial of the screw head.
Screw insertion
Carefully insert the screw without displacing the reduced fragments. Ensure that the screw head is buried in the articular cartilage and does not protrude into the joint.
Insert additional screws as needed using a similar technique.
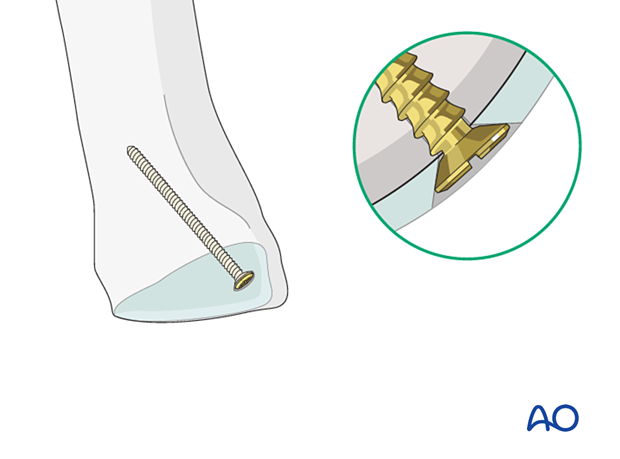
Intraoperative radiologic and visual assessment of joint motion is critical to verify sufficient countersinking.
7. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













