Compression plate
1. Principles
Indication
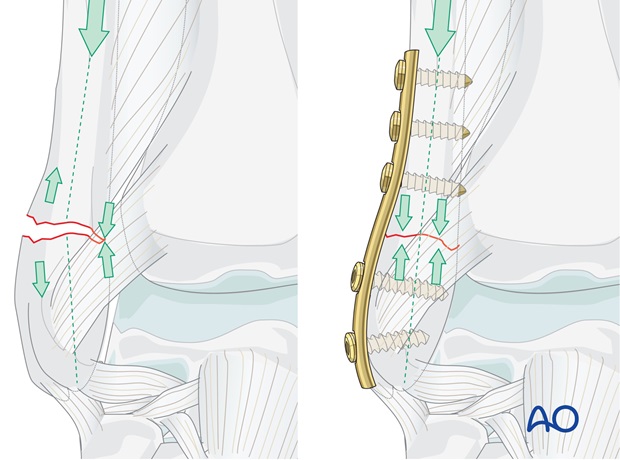
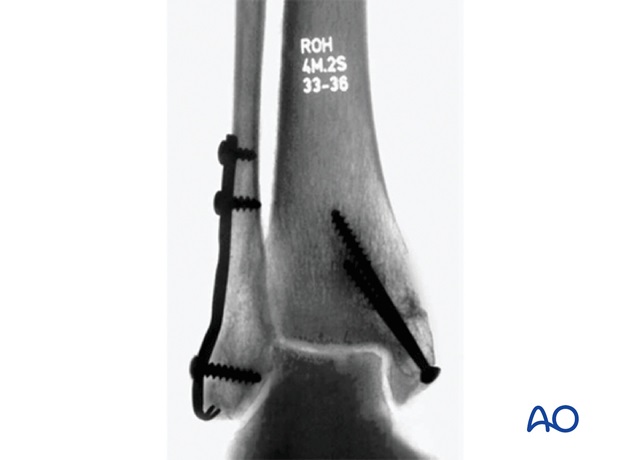
With good bone quality, large infrasyndesmotic fragments of the lateral malleolus with a transverse fracture line can be fixed with a well-contoured plate.

To be able to use a compression plate, the opposite cortex needs to have contact and must be able to resist compression.
Note: the “Compression plate” was referred to as a “Tension band plate”. We now prefer the term “Compression plate” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
2. Patient preparation and approach
The patient may be placed in the following positions:
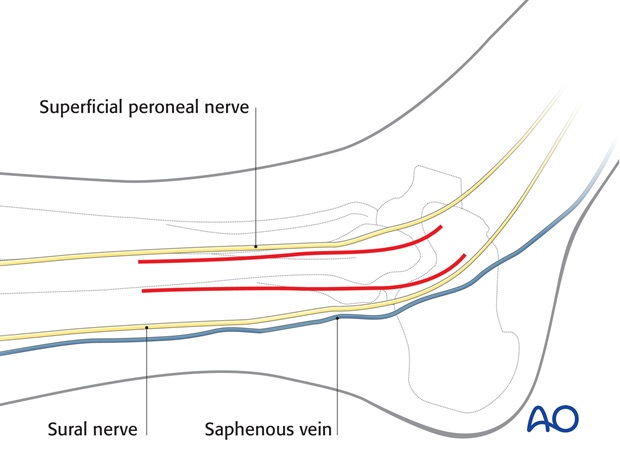
For this procedure a lateral approach is normally used.
3. Reduction
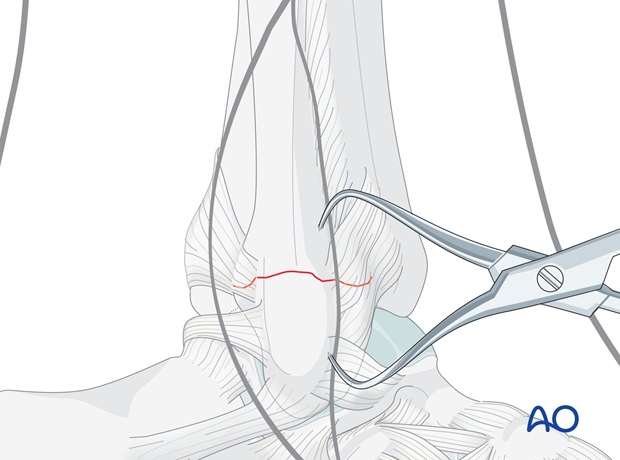
Do not strip the periosteum other than minimally, on either side of the fracture site, to control anatomical reduction of the fragments.
Reduce and temporarily hold the fracture with small pointed reduction forceps.
4. Plate preparation
Choosing length and contouring the plate
Choose the length of a one-third tubular plate as determined by preoperative planning. At least two screws must find a secure hold in each of the distal and the proximal fragments. Usually a five- or six-hole plate is used.
Before the plate is applied, it must be contoured.
Contouring is best done with the help of an appropriate aluminum template. The plate should fit the contour of the bone surface perfectly throughout its entire length.
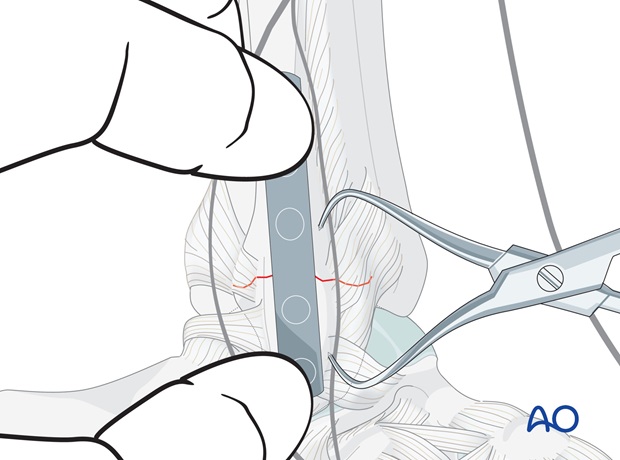
Plate position
Place the contoured plate firmly onto the bone, and determine the position of the first proximal screw near the fracture site.
Remove the plate.
5. Fixation
Plate application
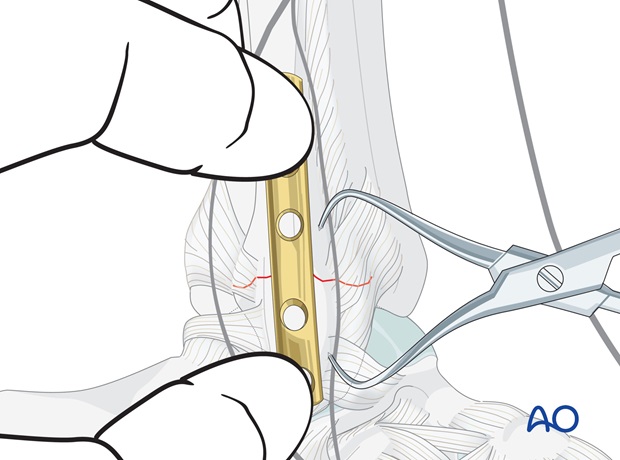
Drill a 2.5 mm hole through both fibular cortices at the planned screw site.
Measure the screw length through the plate, and tap with the 3.5 mm cortical tap in its tap sleeve.
Carefully apply the plate. Insert the first proximal screw. The screw should just penetrate the far cortex.
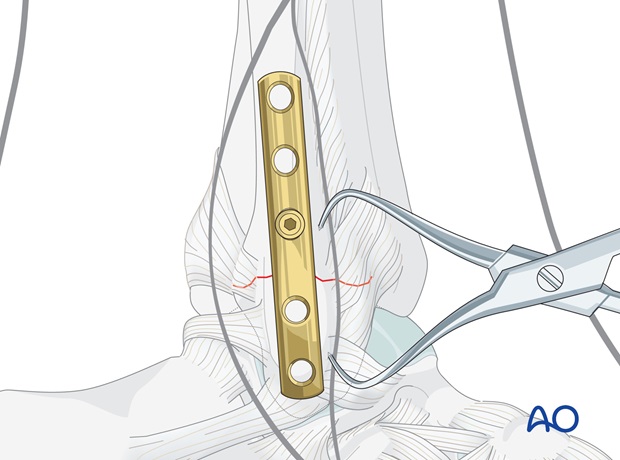
Insertion of the first distal screw
Next, insert a screw into the first distal plate hole. All distal screws are aimed towards the articular surface of the lateral malleolus. Ensure that their tips do not protrude into the joint by aiming the drill slightly posteriorly.
Carefully predrill an eccentric hole (at the distal edge of the plate hole) until the drill bit just penetrates the far cortex. Measure the length and select a cortex screw approximately 2 mm shorter. Tap threads only into the near fibular cortex and then insert the screw.
Note
In osteopenic bone, fully threaded cancellous bone screws can be used in the distal fragment.
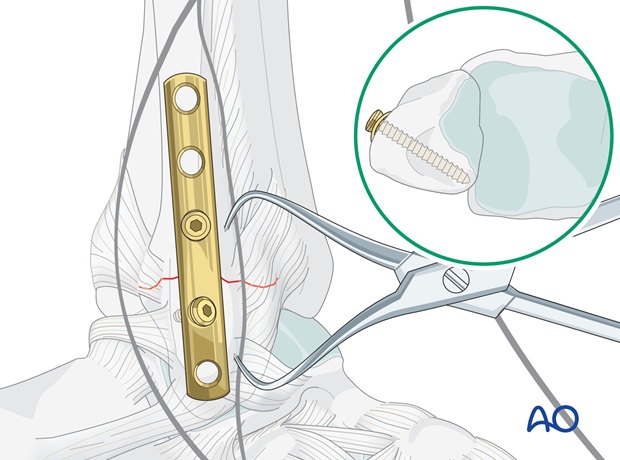
Completing screw insertion
Insert the remaining screws as described above in the sequence of the preoperative plan.
The most distal screw is inserted slightly obliquely, from distal to proximal, in a posterior direction. Again, choose the screw 2 mm shorter than measured and tap the threads only in the near cortical bone.
Gently tighten all screws.
Check under image intensification in both planes to ensure that no screw protrudes into the ankle joint or the syndesmosis.

6. Pearl
A one-third tubular plate molded as a hook plate can be used to fix a small lateral fragment (where there is space for only one screw), or a severely osteoporotic bone.
The sequence of the application of the hook plate differs from the procedure described above.
First, place the tip of the hook through the ligament into the tip of the lateral malleolus.
Use an impactor for anchoring the hook tip in the bone.
Insert a screw into the hole immediately above the hook to secure the plate onto the distal fragment.
Insert a proximal cortical screw in an eccentric position to obtain compression.
Complete the fixation by inserting the other screws in the planned sequence.
7. Postoperative treatment of infra- and trans-syndesmotic malleolar fractures
A bulky compression dressing and a lower leg backslab, or a splint, are applied, and the limb is kept elevated for the first 24 hours or so, in order to avoid swelling and to decrease pain.
In anatomically reconstructed, stable malleolar fractures, early active exercises and light partial weight bearing are encouraged after day one. In osteoporotic bone, weight bearing should be postponed.
X-ray evaluation is made after 1 week and then monthly until full healing has occurred. Progressive weight bearing is recommended as tolerated.













