Lateral approach to the malleoli
1. General considerations
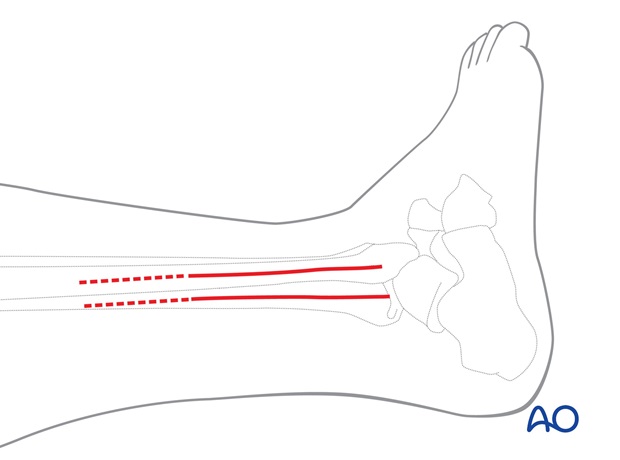
The longitudinal lateral incision is the standard approach for most lateral fractures.
If a lateral plate is required for the lateral malleolus, the incision should be placed either slightly anteriorly or posteriorly, so that the plate does not come to lie directly beneath the incision.
If a posterior plate is planned, place the incision slightly posteriorly, so that the soft-tissue dissection can be minimized.
If access to the anterior syndesmosis is required, or a lag screw from anterior to posterior (Chaput lesion) is planned, place the incision slightly anteriorly.
Make a 10-15 cm incision in line with the fibula, starting proximally. If necessary, continue distally a further 2 cm, curving slightly, anteriorly in relation to the tip of the lateral malleolus, in order to increase exposure and release tension.
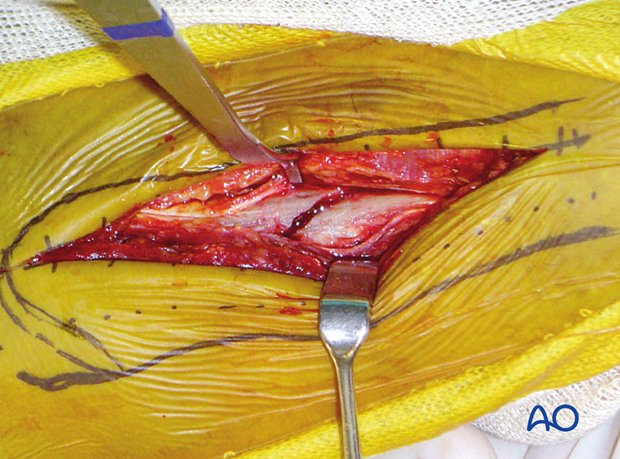
2. Superficial surgical dissection
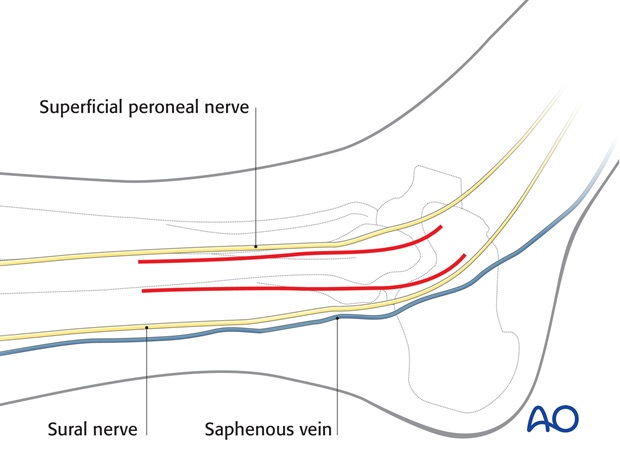
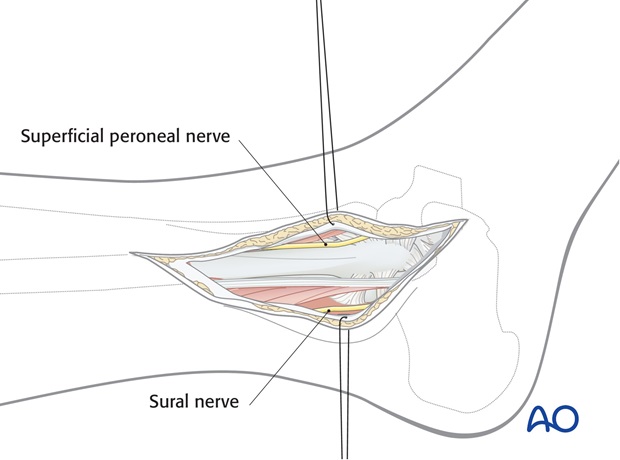
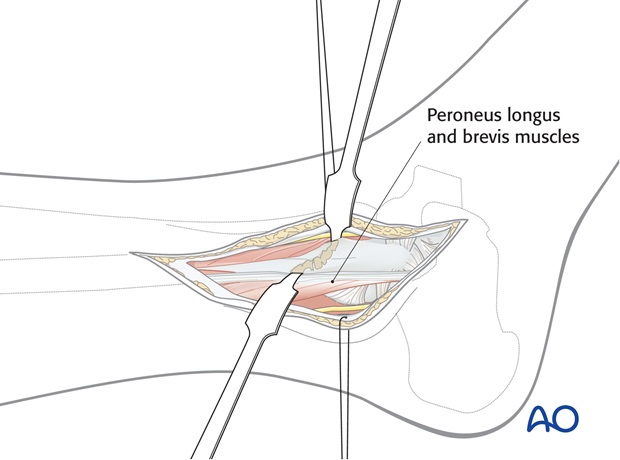
The dissection plane is between the peroneus tertius anteriorly and the peroneus longus and brevis posteriorly. The figure shows a long incision, such as would be used for suprasyndesmotic fractures.
Handling the damaged soft tissue is crucial. Use small retractors only in good soft-tissue conditions. Retracting with protecting sutures is a safe method.
Note
Be careful not to damage the superficial peroneal nerve, which lies very closely anteriorly, especially in the proximal part of the incision. In more anterior incisions, it should be identified and protected. When dissecting posteriorly, be careful not to damage the short saphenous vein and the sural nerve.
3. Deep surgical dissection
Free the periosteum at the fracture site. In order to minimize devascularization, reflect only as much of the periosteum as is needed to expose the fracture site. Unnecessary stripping of the periosteum reduces the blood supply of the bone.
If it is necessary to extend the dissection, keep it close to the periosteum, in order to avoid damage to terminal branches of the peroneal artery.
The fracture site is now exposed. Debris which interferes with accurate reduction should be removed, but fracture hematoma and exposed BMPs are helpful in encouraging new bone growth and fracture healing, so should not be excessively washed out.
4. Extension to the lateral distal tibia (Volkmann lesion)
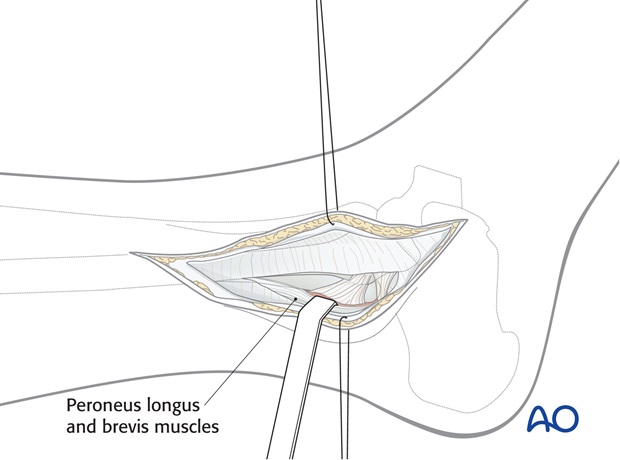
Option 1: Limited exposure
A sizeable Volkmann fragment may be reduced indirectly and fixed with a lag screw from anterior to posterior. When indirect reduction is not anatomical, a limited posterolateral exposure may be used to reduce and fix the fragment.
Incise the fascia parallel to the posterior border of the distal fibula as far as necessary, avoiding damage to the peritenon of the peroneal tendons.
Retract the peroneal muscles and tendons dorsally and approach the postero-lateral edge of the distal tibia directly.
Expose the fracture and elevate the periosteum only sufficiently to control reduction of the dorsal posterior tibial fragment.
Fixation of the Volkmann's fragment may be easier via a Posterolateral approach.
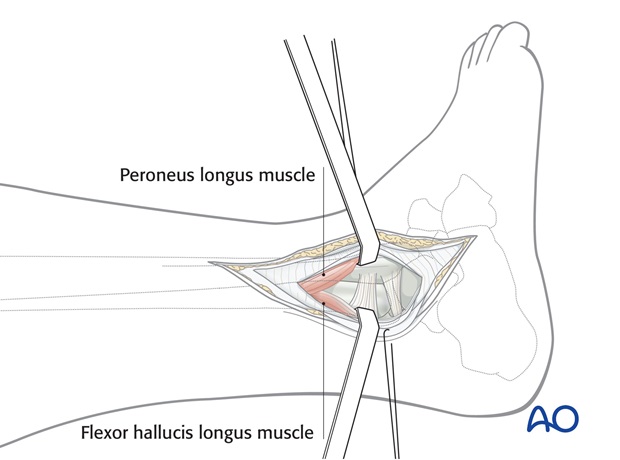
Option 2: Extended exposure
If the limited exposure is not sufficient for the reduction and fixation of a large Volkmann’s triangle, or if an antiglide plate is to be used, incise the fascia dorsal to the peroneal muscles at the border of the flexor hallucis longus muscle.
Beware of the sural nerve posteriorly.
Retract the peroneal muscles anteriorly and the flexor hallucis longus and the Achilles tendon dorsally.
Expose the posterior surface of the tibia.
Expose the fracture, and reflect the periosteum only sufficiently to control reduction of the dorsal posterior tibial fragment.
5. Proximal extension
If a distal fracture extends proximally, the incision can be extended proximally.
The plane of dissection is the same, but particular care must be taken with the superficial peroneal nerve. In this case it is advisable to identify and protect the nerve.